Andreas Grabinsky
I. Initial Trauma Evaluation and Resuscitation
The treatment of seriously injured patients is time-sensitive and requires a coordinated and systematic approach from all medical providers. This should include those with anesthesiology training who are providing acute resuscitative care in the emergency medical setting or perioperative care in the operating room and intensive care unit (1). Rapid assessment of injuries and institution of life-saving therapies is guided by tenets of the American College of Surgeons’ Advanced Trauma Life Support (ATLS) program. ATLS management of injured patients consists of the primary survey (identification of life-threatening injuries), resuscitation (immediate treatment of such injuries as they are identified), the secondary survey (comprehensive assessment of all other injuries and associated conditions), and definitive care (medical, surgical, or critical care).

The primary survey and initial resuscitation of the severely injured patient follow the ABCDE acronym: Airway, Breathing, Circulation, Disability (neurologic function), and Exposure (completely expose and examine the patient so that no injury is missed).
A. Airway Evaluation and Management
Assessing and securing the airway of the trauma patient is the first step of the primary survey and associated resuscitation. Chapter 20 provides comprehensive details of airway management in elective and emergent settings, including application of the American Society of Anesthesiologists (ASA) difficult airway algorithm (see Appendix F).
Airway assessment (Tables 20-4, 20-5, 20-6) can be limited in the trauma setting by lack of patient cooperation and preclude use of the Mallampati classification (Fig. 20-3). Thus, trauma airway assessment largely relies on visual inspection of the patient’s face, head, and neck. A short, fat neck with fewer than three finger-breadths from the thyroid notch to the jaw tip (i.e., thyromental distance) is concerning for a difficult airway. Obvious facial asymmetry further suggests an underlying anatomic abnormality, be it traumatic, congenital, or neoplastic. Limited neck range of motion further suggests a more challenging airway, although cervical motion should not be assessed in patients with suspected cervical spine injuries.
Mask ventilation and tracheal intubation can both be challenging in trauma patients due to head and neck injuries, recent oral intake that increases aspiration risk, and possible lung injury that can negatively impact both oxygenation and ventilation. Adherence to the ASA difficult airway algorithm is essential, including planning and preparation of multiple backup airway management techniques.
To assist the laryngoscopist with visualization of the vocal cords, cricoid pressure is typically applied in a backward, upward, rightward fashion (i.e., BURP). Although this is common practice, the literature supporting cricoid pressure is controversial, and the technique may in some cases interfere with vocal cord viewing or tracheal tube placement. Cricoid pressure is not intended to prevent aspiration in a vomiting patient, but rather to prevent passive reflux of gastric contents into the posterior pharynx and facilitate laryngeal viewing. In fact, if a patient begins to vomit, one must release cricoid pressure, turn the patient on his or her side (if possible), and suction the emesis. Maintenance of cricoid pressure during active vomiting risks esophageal injury.
Manual in-line stabilization (MILS) of the cervical spine is routinely used in emergency airway management of trauma patients in whom a spinal cord injury is suspected. Patients with documented spinal cord injuries rarely have worsening of their neurologic injury with proper MILS during direct laryngoscopy and tracheal intubation. Cadaveric studies have shown that MILS does not ensure spine immobility, however. Persisting with rigid adherence to MILS in the context of a poor view of the vocal cords can increase the difficulty and duration of tracheal intubation; therefore, application and possible relaxation of MILS must be considered in the context of the overall clinical picture.
B. Breathing Evaluation and Management
Respiratory assessment is a critical component of the primary survey and resuscitation phases. Indications for tracheal intubation include obvious respiratory distress, inability to speak in complete sentences, an elevated respiratory rate, poor oxygenation, poor ventilation, or significant traumatic brain injury.
Patients who arrive with an airway device placed prior to hospital arrival must be immediately evaluated to ensure proper position and function of the device. End-tidal carbon dioxide and the presence of bilateral breath sounds should be evaluated and documented to confirm satisfactory ventilation. Alternative airway devices such as the King LT (King System, Noblesville, IN) airway, Combitube (Moore Medical, Farmington, CT), or laryngeal masks do not protect the airway from aspiration of stomach contents, blood, saliva, or tooth fragments. They should be replaced with a cuffed endotracheal tube as soon as possible. A gastric tube should also be placed soon after tracheal intubation to further mitigate the risk of aspiration.
C. Circulation Evaluation and Shock Management
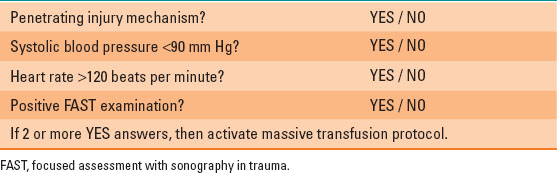
Shock is defined as inadequate tissue perfusion. Delayed capillary refill, cold and “clammy” skin, impaired mentation, and oliguria are classic signs in trauma patients that most often suggest hypovolemic shock due to massive hemorrhage. Blood pressure and heart rate can help provide more quantifiable assessment of systemic perfusion and shock. For example, low blood pressure is typically compensated for with an elevated heart rate (see Chapter 3). The assessment of blood consumption score (Table 32-1) is a tool that uses four simple clinical assessments to determine the likelihood of hemorrhagic shock and the associated need for early massive blood transfusion.
Table 32-1 Assessment of Blood Consumption
The immediate treatment goals for hemorrhagic shock are to stop ongoing bleeding and restore tissue perfusion by replacing intravascular volume (see Chapter 23). The use of tourniquets for massive bleeding from extremities is supported by recent military experience with blast injuries. Ultimately, any patient in extremis must have his or her blood volume restored and be rapidly transported to the operating room for definitive control of internal or external bleeding.
D. Neurologic Evaluation and Management
A prompt neurologic evaluation during the primary survey is important for establishing a baseline examination for future treatments. Given that the anesthesiologist is often the last person to speak to a conscious patient prior to induction of anesthesia or tracheal intubation, an understanding of the Glasgow coma scale (Table 32-2) is critical to rapidly evaluate the mental status and motor function of trauma patients. It also guides the need for tracheal intubation in patients with traumatic brain injury (TBI). Of note, the iris contains no nicotinic acetylcholine receptors; therefore, neuromuscular blocking agents do not affect pupil size.
Table 32-2 Glasgow Coma Scale
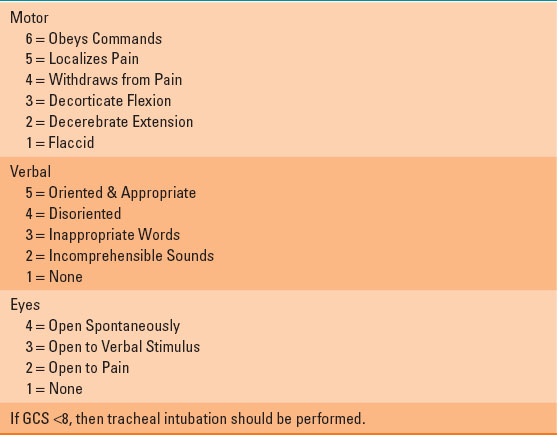
TBI is the leading cause of death in trauma. Any suspicion of TBI should be evaluated with a head computed tomography (CT) scan to identify primary injuries (e.g., intracranial hematoma) that require immediate surgery or specialized critical care. Throughout the initial evaluation and treatment period, however, priority is given to maintaining adequate blood pressure and oxygenation to avoid secondary brain injury due to neuronal ischemia. Guidelines from the Brain Trauma Foundation recommend that systolic blood pressure be >90 mm Hg and oxygen saturation be >90% at all times. Even transient reductions in blood pressure or oxygen saturation can profoundly affect the mortality of these patients (2). Perioperative anesthetic management of TBI is discussed in detail in Chapter 30.

The 15-point Glasgow coma scale requires cooperative motor responses and verbal skills that are found in older children and adults, but not in younger children or infants; thus, a similar, but modified 15-point pediatric Glasgow coma scale is available and should be used in preverbal children and infants.
In patients who have sustained a spinal cord injury (SCI), it is important to assess the anatomic level of the neurologic deficit as soon after the event as possible. Sensory level is determined by dermatome level of touch or pain. Motor function is assessed using the American Spinal Injury Association score (Table 32-3). Assessment of anal sphincter tone is also an important component of the motor examination.
Table 32-3 American Spinal Injury Association (ASIA) Spinal Cord Injury Classification
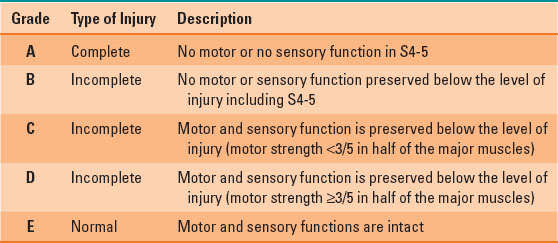
In the past, patients with SCI were treated with methylprednisolone infusions to decrease spinal cord swelling and enhance recovery of function. Recent literature, however, has not demonstrated a significant benefit of such therapy and instead showed an increased risk of infection. Thus, steroid administration is not currently recommended in SCI.
Initial management of suspected cervical spine injuries includes placement of a rigid cervical collar to minimize cervical motion. Because it is often challenging to rule out SCI in intoxicated or head-injured patients, these patients should remain in a cervical collar until definitive imaging can be performed. Recent data support removal of a cervical collar in adult patients with normal cervical spine CT scans who spontaneously move all four extremities.
E. Other Major Vascular Injuries
Initial evaluation of major vascular injuries includes assessment of the affected extremity for presence and character of pulse as well as skin color and temperature. A cool and poorly perfused limb must be immediately evaluated for possible arterial injury and revascularization. Similarly, obvious vascular injury with external hemorrhage must be immediately addressed with hemorrhage control and fluid resuscitation. Placement of temporary tourniquets on a limb with life-threatening bleeding is a simple and effective hemostasis measure. In cases of significant pelvic trauma and retroperitoneal bleeding, placement of a pelvic binder can reapproximate pelvic fractures to a degree sufficient to temporarily limit blood loss. Interventional, endovascular radiology techniques are frequently used to control pelvic and liver bleeding, thereby avoiding complications associated with open surgical repairs. Aortic injuries are evaluated with a contrast CT scan of the chest and abdomen. Transesophageal echocardiography can be used to evaluate the ascending aorta, aortic arch, and descending aorta for potential disruption.
F. Interdisciplinary, Team-Based Management
Crew resource management is a concept developed by the aviation industry in which each member of the multidisciplinary team has equal responsibility for passenger safety. For example, any member of a flight crew can alert the pilot in command of a potential hazard. This concept is particularly relevant to trauma, when care is necessarily multidisciplinary and critical events must occur in a timely fashion. Central to the concept of crew resource management is clear and free communication between all parties, regardless of hierarchy. When several events and therapies must occur simultaneously, it can be valuable to use a checklist to ensure that no critical steps are overlooked (3). The recommended checklist for trauma and emergency anesthesia is shown in Figure 32-1. Assigning predetermined positions to members of the anesthetic resuscitation team is also an effective way to maintain organization in the trauma operating room (Fig. 32-2).
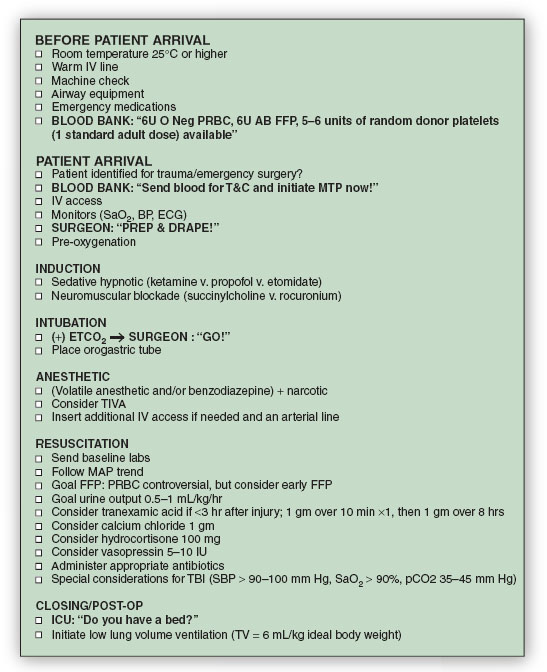
FIGURE 32-1 Emergency and trauma anesthesia checklist. Critical preparation and treatment strategies are shown for each successive step in the emergent, perioperative care of the major trauma victim. PRBC, packed red blood cells; AB FFP, type AB fresh frozen plasma; T&C, type and cross; MTP, massive transfusion protocol; SaO2, oxygen saturation; BP, blood pressure; ECG, electrocardiogram; ETCO2, end-tidal carbon dioxide; TIVA, total intravenous anesthesia; MAP, mean arterial blood pressure; TBI, traumatic brain injury; SBP, systolic blood pressure.
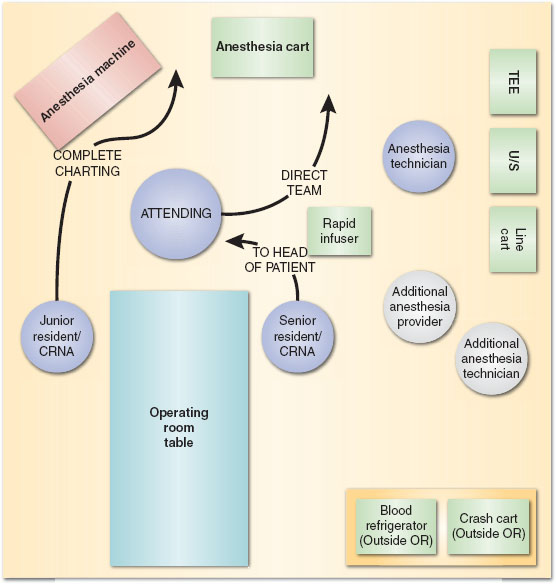
FIGURE 32-2 Trauma anesthesia team work flow diagram. The ideal floor plan setup for anesthetic care of the major trauma patient includes assigned spaces for various anesthesia providers, the anesthesia workstation, and critical equipment.
II. Operative Management: General Considerations
A. Monitoring
Standard ASA monitors are described in Chapter 15. In emergencies, the oxygen saturation monitor can provide reasonably accurate heart rate and numeric oxygen saturation information. It also is an indirect indicator of peripheral perfusion, as a poor quality waveform suggests poor peripheral perfusion. An arterial line can provide accurate beat-to-beat measurement of blood pressure and facilitate frequent blood sampling. It can also use emerging technologies for arterial waveform analysis (see Chapter 23) to estimate cardiac output and intravascular volume status. Placement of an arterial line, however, should never delay the start of an emergent surgical case.
B. Anesthetic and Adjunct Drugs
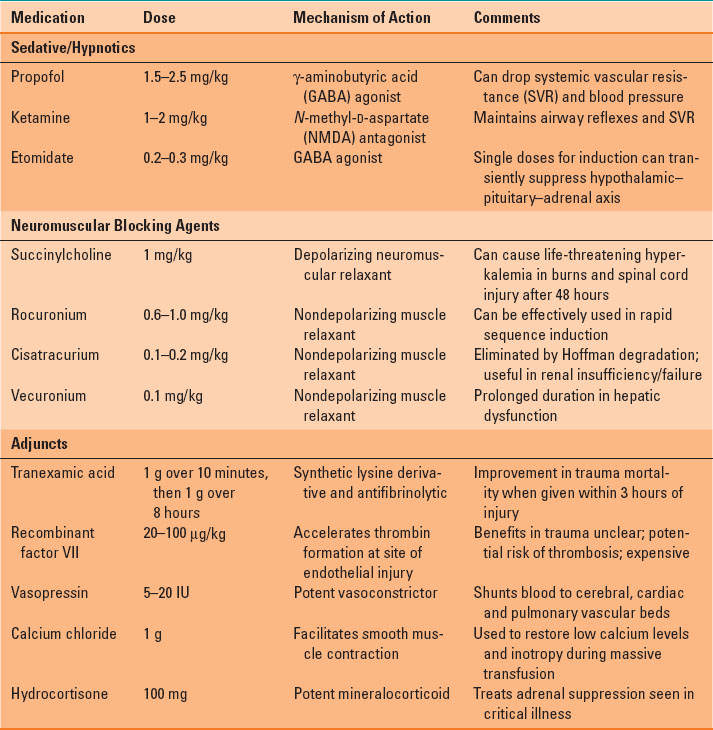
Severely injured patients with hypovolemia are very susceptible to the negative inotropic and vasodilatory effects of anesthetics, especially volatile anesthetics. Thus, all anesthetic drugs should be slowly and carefully titrated to avoid cardiovascular collapse in such patients. A partial list of commonly used perioperative anesthetic and adjunct drugs, along with specific cautions for use in trauma patients, is provided in Table 32-4.
Table 32-4 Anesthetic and Adjunct Drugs Commonly Used for Trauma Anesthesia and Resuscitation
C. Induction and Airway Management
Rapid sequence induction (RSI) is the process by which an endotracheal tube is rapidly placed by direct laryngoscopy during emergency airway management (see Chapter 20). RSI is commonly employed in trauma patients. When it is combined with MILS in patients at risk for cervical spinal cord injury, it is a safe, effective method to secure the airway. When a hard cervical collar is in place, the front portion of the collar can be removed (with MILS applied) immediately after induction to facilitate mandible subluxation and laryngeal viewing.

Whereas rapid sequence induction and intubation is generally a two-person procedure, a minimum of three providers are required when performing the procedure in a patient with possible cervical spin injury: one to hold manual in-line neck stabilization, one to provide cricoid pressure, and one to perform tracheal intubation.
Video laryngoscopy (e.g., Glidescope, Verathon Inc., Bothell, WA) is increasingly used in emergency settings. Although video laryngoscopy can improve visualization of the vocal cords, it does not decrease time to intubation or improve successful first attempt intubation (4). The benefit of video laryngoscopy may be confined to patients with difficult airway anatomy (e.g., limited mouth opening or neck mobility) or to novices or those who do not perform direct laryngoscopy regularly (5). Supraglottic airways (e.g., laryngeal mask) provide a blind insertion alternative to tracheal intubation. In the prehospital environment, such devices may be easier to place by providers with limited tracheal intubation experience. In the hospital setting, they serve as effective rescue devices in “can’t intubate, can’t ventilate” scenarios.
D. Hypotension
As noted previously, ongoing blood loss frequently leads to hypovolemic shock in patients with major or multiple injuries. Aggressive resuscitation in the presence of untreated injuries can actually worsen blood loss by increasing intravascular pressure in injured vessels. The concept of “hypotensive resuscitation” aims to mitigate blood loss in these cases by targeting a lower-than-normal blood pressure—yet still provide vital organ perfusion—until source control of hemorrhage is achieved. Although animal models have offered encouraging results with hypotensive resuscitation, human data have been less encouraging, and documented benefit appears limited to victims of penetrating injury.
Although it is difficult to quantify the ideal blood pressure goal during resuscitation, mean arterial pressure trends often provide a better assessment of resuscitation progress than reliance on discrete systolic blood pressure values. Recent literature suggests that the risk of acute kidney or myocardial injury is increased with mean arterial pressures below 55 mm Hg (6), thus supporting this value as a lower target limit during resuscitation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








