Isuta Nishio
Nonoperating room anesthesia (NORA) refers to anesthesia services that are provided outside of traditional surgical operating rooms. These locations include, but are not limited to, radiology departments, endoscopy suites, magnetic resonance imaging (MRI) and computerized tomography (CT) scanners, and cardiac catheterization (cardiac cath) and electrophysiology (EP) laboratories. NOR cases account for a significant proportion of the procedural work of hospitals, and, increasingly, patients or the proceduralists require or request anesthesia or sedation to facilitate these procedures. This chapter will discuss the care of patients requiring anesthesia or sedation for procedures in NOR locations. Anesthesia for surgical procedures performed in offices and ambulatory surgery centers is addressed Chapter 25, and anesthesia and analgesia provided for labor and delivery is discussed in Chapter 31.
I. The Three-Step Approach to Nonoperating Room Anesthesia
NORA covers a diverse spectrum of patients, procedures and locations and a systematic approach is recommended. The simple three-step paradigm—the patient, the procedure, and the environment—may be a useful mnemonic for NORA (Fig. 38-1).
FIGURE 38-1 A simple three-step paradigm for nonoperating room anesthesia.
A. The Patient
Patients may require sedation or anesthesia to tolerate NOR procedures for a number of reasons (Table 38-1). Children often require sedation or anesthesia for diagnostic and therapeutic procedures. Patients with significant comorbidities or surgical disease may be too ill to tolerate a major operative procedure, whereas a palliative, less-invasive NOR procedure may be possible. All patients presenting for NORA require a thorough preanesthesia assessment and the development of a sound anesthetic plan with appropriate levels of monitoring.
B. The Procedure
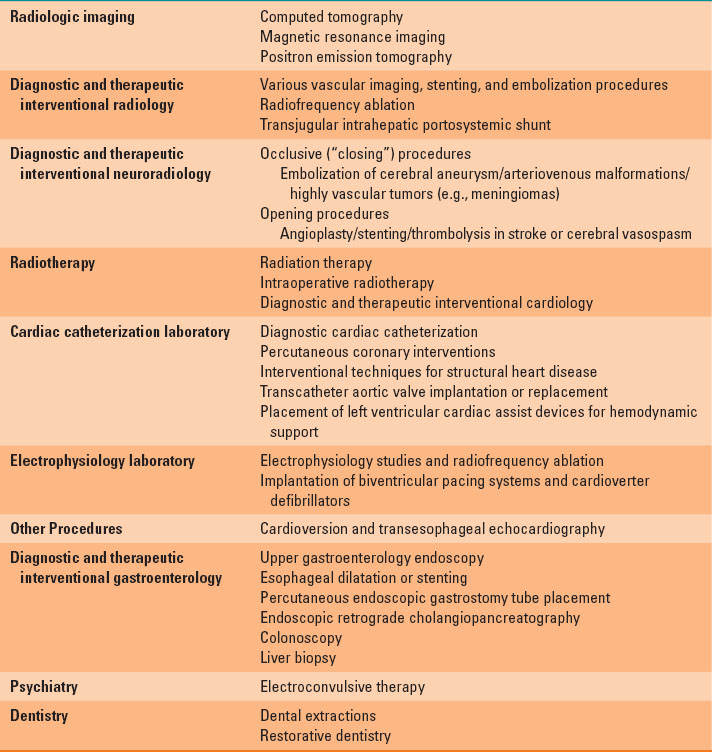
Common NOR procedures for which the patient may require anesthesia or sedation are listed in (Table 38-2). The anesthesiologist must understand all the details of the NOR procedure, specifically the position the patient will be in, how painful the procedure will be, how long it will take, and any special requirements (such as use of contrast media or the need to wake the patient up halfway through). Preoperative communication with the proceduralist is essential and must include discussion of contingency plans for emergencies and complications.
C. The Environment
Unlike in operating rooms, the conditions under which NORA services are delivered may vary greatly in terms of the space, equipment, and staff available. A number of factors contribute to NORA sites being unfamiliar and less optimal environments for anesthesia providers (Fig. 38-2):
 VIDEO 38-1
VIDEO 38-1
Anesthesia in Remote Locations
1. These locations were often designed before or without considering whether anesthesia would be needed for patients undergoing care. Access to the patient by the anesthesia provider is often limited by diagnostic and therapeutic equipment such as CT and MRI scanners, fluoroscopes, or endoscopy towers.
2. Hazards unique to specific locations exist such as radiation in fluoroscopy and CT and the magnetic field in MRI.
3. Proceduralists and ancillary staff may be unfamiliar with the requirements for safe anesthesia care and how to assist anesthesia providers when a difficulty is encountered.
4. Away from the operating room, immediate help from anesthesia colleagues in case of emergency may not be readily available.
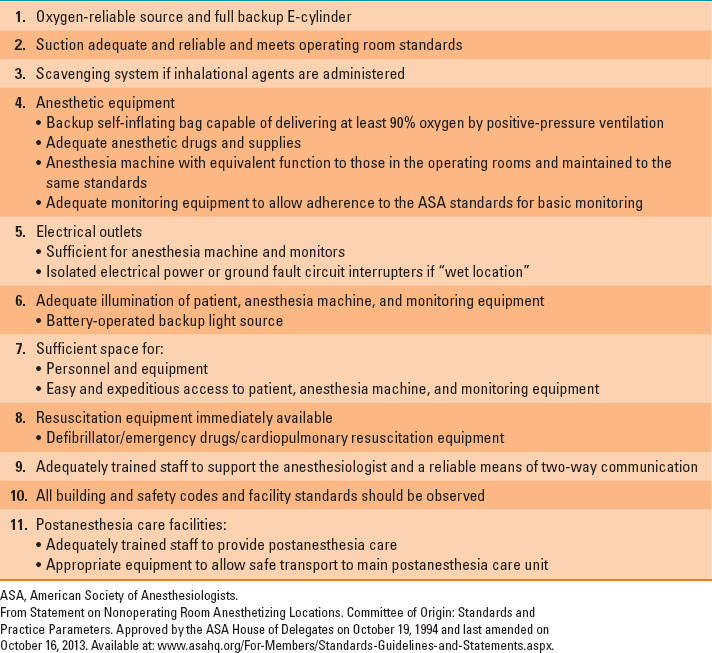
The American Society of Anesthesiologists (ASA) has developed standards for NORA (1). Prior to the anesthetic, the presence and proper functioning of all equipment needed for safe patient care must be established; this is described in Table 38-3.
The location of immediately available resuscitation equipment should be noted and protocols developed with the local staff for dealing with emergencies, including cardiopulmonary resuscitation and the management of anaphylaxis.

FIGURE 38-2 A radiology suite showing a C-arm and the high density of equipment that may separate the anesthesiologist from the patient.
Table 38-1 Patient Factors Requiring Sedation or Anesthesia for Nonoperating Room Procedures
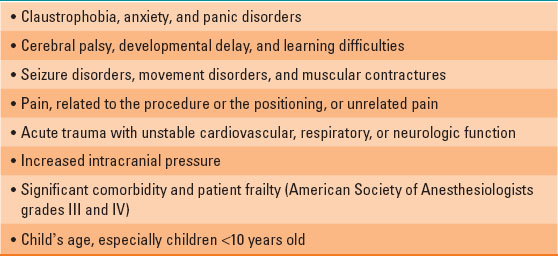
Table 38-2 Common Nonoperating Room Anesthesia Procedures
II. Standards of Care for Nonoperating Room Anesthesia
Many NOR procedures are performed under sedation or monitored anesthesia care. Anesthesia care may be thought of as a continuum, with a gradual transition from the awake state, through progressively deepening sedation to general anesthesia (Table 38-4) (2).
As sedation deepens, progressive blunting of the airway reflexes, with the potential for airway obstruction, together with depression of spontaneous ventilation can ensue. The individual responsiveness of patients to different sedative agents varies, as do the levels of stimulation during the course of a procedure. Consequently, during the course of a NOR procedure under sedation, the patient may drift to a deeper level than is intended, resulting in airway and respiratory depression. It is, therefore, essential that the person providing sedation be properly trained to care for a patient who drifts to a deeper level of sedation than the level originally intended.
At the conclusion of the NOR procedure, the patient should be transported by a member of the anesthesia team to a recovery area that is equipped to the same standards as for all postoperative patients.

The same standards for operating rooms should be applied to patients being cared for in all nonoperating room sites.
III. Adverse Events
Significant adverse events in NORA are rare; however, the number of deaths associated with NORA is higher than for operating room anesthesia (3). Complications related to the airway and respiratory system, such as airway obstruction and respiratory depression as a result of oversedation, are the most common complications associated with NORA. This is particularly relevant in patients with obstructive sleep apnea, who are more prone to airway and respiratory complications during and after anesthesia and sedation.

More than 80% of surgical patients are unaware that they have obstructive sleep apnea prior to undergoing surgery.
Table 38-3 American Society of Anesthesiologists’ Standards for Nonoperating Room Anesthesia Locations
IV. Environmental Considerations for Nonoperating Room Anesthesia
A. X-rays and Fluoroscopy
Fluoroscopy (C-arm) is widely used in many NOR locations, including interventional radiology, cardiac catheterization, electrophysiological procedures, and in the gastroenterology suite. The C-arm moves back and forth around the patient during the procedure, requiring large amounts of space, limiting access to the patient, and serving as a means of dislodging intravenous lines and endotracheal tubes (Fig. 38-2).
B. Computed Tomography
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








