Jonathan B. Mark
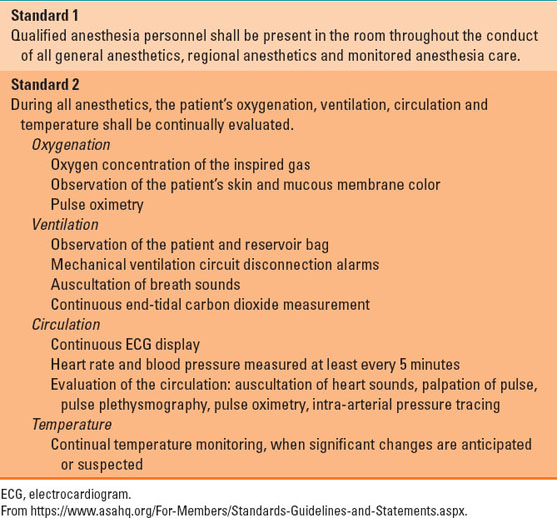
Monitoring of patients during anesthesia begins with a vigilant anesthesia provider—visual inspection of chest rise and patient color for ventilation and oxygenation and palpation of the pulse for heart rate and blood pressure estimation. Although technology has enhanced the anesthesia provider’s ability to monitor and treat patients during anesthesia and surgery, a vigilant anesthesia provider with good clinical decision-making skills is still required. Standards for basic anesthetic monitoring published by the American Society of Anesthesiologists emphasize the need for a qualified anesthesia provider to be in the room for all anesthetics and monitored anesthesia care (Table 15-1).
 VIDEO 15-1
VIDEO 15-1
Monitoring Standards
Table 15-1 Summary of the American Society of Anesthesiologists “Standards for Basic Anesthetic Monitoring”
I. Basic Anesthesia Monitoring
The “Standards for Basic Anesthetic Monitoring” were first published in 1986 and updated in 2011 (Table 15-1) (1). These standards lay the foundation for the minimal monitoring needed during all anesthesia care, and they begin with the continual presence of a qualified anesthesia provider. Depending on the clinical judgment of this provider, more intensive monitoring may be needed in some cases.
A. Oxygenation
Proper oxygenation of the patient is ensured in two ways. During general anesthesia using an anesthesia machine, the provider needs to confirm that there is a sufficient concentration of oxygen being delivered. Most anesthesia machines use a galvanic cell analyzer located in the inspired limb of the anesthesia circuit and are equipped with a low oxygen concentration alarm that will alert the provider to a dangerous hypoxic gas mixture. The oxygen analyzer may require daily calibration and intermittent replacement. If a patient is receiving supplemental oxygen by nasal cannula or facemask during regional anesthesia or monitored anesthesia care, the provider must ensure the proper flow of oxygen from the wall oxygen supply or gas cylinder.
After ensuring sufficient oxygen delivery to the patient or the breathing circuit, oxygenation of the patient’s blood must be monitored qualitatively, most often via the patient’s skin or mucous membrane color, and quantitatively with a pulse oximeter. This device has become ubiquitous both inside and outside the operating room because it provides a continuous, noninvasive, and accurate measurement of arterial hemoglobin oxygen saturation.
The pulse oximeter emits two wavelengths of light (red and near infrared) and uses a photo detector to measure the absorbance of oxygenated and deoxygenated hemoglobin in the blood. The oximeter then uses an algorithm to calculate the percentage of the total hemoglobin that exists as oxyhemoglobin, and displays this as the hemoglobin saturation (SpO2). This monitor must also differentiate the pulsatile arterial signal (and thus the arterial hemoglobin oxygen saturation) from the nonpulsatile venous (and other tissue) saturation. Although a pulse oximeter is considered to be a continuous monitor, there can still be a significant delay (of up to 15 to 30 seconds) before it alarms to note a decrease in the SpO2.

The pulse oximeter has a significant delay (15 to 30 seconds) in the detection of changes in arterial oxygen saturation.
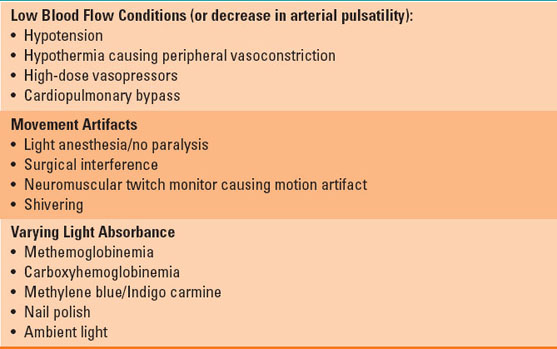
The pulse oximeter is an extremely important monitor during anesthesia, and an abnormally low or suddenly decreasing SpO2 (<90%) triggers the monitor to provide an audible warning alert of impending patient deterioration. However, like any monitor, the pulse oximeter is subject to artifacts and inaccurate readings (Table 15-2). A vigilant anesthesia provider is necessary to determine whether a low SpO2 on the monitor is artifactual or a real event that necessitates intervention.
Table 15-2 Limitations of the Pulse Oximeter
Beyond measurement of SpO2, the pulse oximeter may have other features that are useful during anesthesia. The pulse oximeter plethysmographic waveform provides a measurement of heart rate (pulse rate) and a crude estimation of blood pressure, because the waveform will appear dampened when there is severe hypotension. Newer generations of pulse oximeters are less influenced by patient motion and other sources of artifact. Some devices measure the concentration of other forms of hemoglobin (i.e., carboxyhemoglobin and methemoglobin) and even measure the total hemoglobin concentration (2). Pulse oximeter waveform analysis may also be used to estimate intravascular volume status and volume responsiveness through analysis of the changes in pulse wave contour during the respiratory cycle. Although the pulse oximeter is mostly used with a finger probe, other probes can be used on the ear, nares, or cheek. Pulse oximeters will not work when there are no arterial pulsations (e.g., on cardiopulmonary bypass), and other techniques must be used, such as reflectance oximetry, which does not depend on arterial pulsations.
B. Ventilation
Ventilation, or the movement of gases between the environment and the alveoli, is another important aspect of a patient’s physiology to monitor during anesthesia (Table 15-1). This can be accomplished by visual inspection of chest rise and fall, condensation of airway water vapor in the endotracheal tube or facemask during expiration, or the cyclic filling and emptying of the reservoir bag or ventilator bellows. The anesthesia machine measures tidal volume and respiratory rate and can alarm if these ventilator parameters fall outside a predetermined range.
During general anesthesia, the best monitor for determining adequacy of ventilation is the measurement of exhaled carbon dioxide (CO2). A small sample of respiratory circuit gas is continually removed from the anesthesia breathing circuit for measurement of CO2 and other gases using an infrared absorption spectrophotometer. The CO2 concentration is continually displayed as a time-dependent waveform, called a capnogram (Fig. 15-1), and is usually reported in millimeters of mercury (mm Hg).
 VIDEO 15-2
VIDEO 15-2
Capnogram and Airway Pressure Tracing
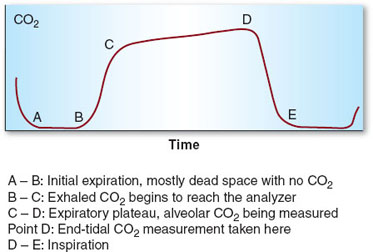
Figure 15-1 Normal capnogram and phases of the respiratory cycle. (From Connor, CE. Commonly used monitoring techniques. In: Barash P, Cullen B, Stoelting R, et al., eds. Clinical Anesthesia. 7th ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins, 2013:263–285, with permission.)
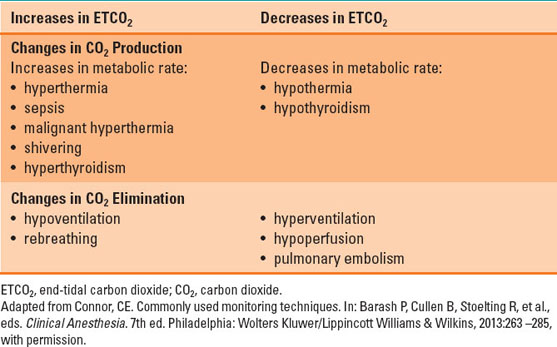
At the beginning of a general anesthetic, a normal-appearing capnogram confirms correct placement of the endotracheal tube in the trachea rather than the esophagus. Both the CO2 value and the shape of the capnogram provide important diagnostic clues about metabolic, respiratory, circulatory, or technical problems with the patient or anesthesia machine (Fig. 15-2 and Table 15-3). For example, a decrease in the end-expiratory or end-tidal CO2 (ETCO2) indicates a potentially serious problem that must be addressed. Although the most common cause of low ETCO2 is hyperventilation or increased dead space ventilation, a sudden and large decrease may be a sign of a misplaced endotracheal tube or a reduction in lung perfusion resulting from pulmonary embolism, anaphylaxis, or cardiac arrest. Capnography is also an important monitor during regional anesthesia or monitored anesthesia care. Although the CO2 value measured from a nasal cannula or facemask will likely underestimate the true ETCO2, owing to dilution with room air, a marked change in the capnogram or loss of the waveform entirely provides a prompt alert that there may be severe hypoventilation, apnea, or obstruction of the airway. Particularly in patients who are breathing supplemental oxygen, the capnogram is an early warning that occurs before a low SpO2 is detected by the pulse oximeter.
 VIDEO 15-3
VIDEO 15-3
Cardiac Arrest

The shape of the capnograph provides important information including the presence of bronchospasm.
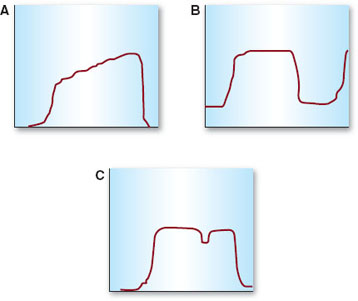
Figure 15-2 Abnormal capnograms. A: Steep, prolonged upslope indicating bronchospasm or expiratory airway obstruction. B: Increase in the baseline due to rebreathing carbon dioxide (CO2), such as with an exhausted CO2 absorbent. C: “Curare cleft,” which may indicate a patient’s attempt at spontaneous ventilation during positive pressure mechanical ventilation.
Table 15-3 Factors that May Change the End-Tidal CO2 Measurement or Waveform during Anesthesia
 VIDEO 15-4
VIDEO 15-4
Hypocarbia Differential Diagnosis
C. Circulation
A patient’s circulation is monitored in multiple different ways during anesthesia. Continuous electrocardiogram (ECG) monitoring is standard of care in anesthesia and provides continuous important information (Table 15-4), including cardiac rate and rhythm. A wide range of rhythm disturbances may occur during anesthesia, and most all can be detected and diagnosed with a simple three-lead ECG system. However, cardiac ischemia is best detected by monitoring a five-lead ECG and displaying both leads II and V5, a technique that can have a sensitivity of up to 80% (3). V5 is often used instead of the potentially more sensitive medial leads (i.e., leads V3 and V4) (Fig. 15-3), because the latter often interfere with the sterile surgical field. ST-segment depression, or subendocardial ischemia (Fig. 15-4), is probably the most common form of perioperative cardiac ischemia, reflecting an oxygen supply–demand mismatch, or demand ischemia. However, transmural cardiac ischemia reflected by ECG ST elevations can also be seen in the perioperative setting (Fig. 15-5).
 VIDEO 15-5
VIDEO 15-5
Electrocardiogram Principles
 VIDEO 15-6
VIDEO 15-6
Heart Electrical Conduction System
It is important to note that the ECG is only a monitor of cardiac electrical activity and it is possible to have a normal-appearing ECG tracing with little or no cardiac output or blood pressure (i.e., pulseless electrical activity or pulseless electrical activity arrest). Therefore, other devices are used in the operating room to further assess a patient’s circulation. As already mentioned, the pulse oximeter plethysmographic waveform can provide an indication of adequate perfusion to an extremity and displays an additional monitor of pulse rate.
Table 15-4 Goals of Intraoperative Electrocardiogram Monitoring
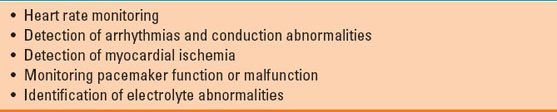
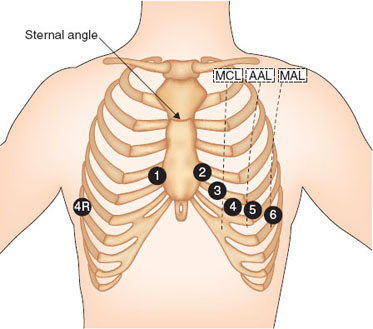
Figure 15-3 Precordial electrocardiogram lead placement. V3 or V4 may be more sensitive for detecting cardiac ischemia, however V5 is often used, as it is more likely to avoid the surgical field. MCL, mid-clavicular line; AAL, anterior axillary line; MAL, mid-axillary line. (From Mark JB. Atlas of Cardiovascular Monitoring. New York: Churchill Livingstone; 1998, with permission.)
Blood pressure should, at the very least, be monitored every 5 minutes via a noninvasive blood pressure cuff. Automatic blood pressure cuffs differ slightly between manufacturers but most commonly use the oscillometric method
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







