Armagan Dagal
I. Preoperative Assessment
Orthopedic spine and extremity surgeries are generally classified as intermediate-risk surgery, although major spine surgery or more limited procedures in patients with pre-existing medical conditions (e.g., hip arthroplasty in the elderly) can significantly increase perioperative risk. The purpose of the preoperative assessment includes the identification and optimization of modifiable risk factors, explanation of the risks, and formulating the best possible anesthetic plan for the patient. In addition to the standard preoperative assessment (see Chapter 16), focused orthopedic evaluation should include:
• Airway and cervical spine assessment (e.g., rheumatoid arthritis, osteoarthritis, and ankylosing spondylitis could result in limited neck motion, atlantoaxial instability, or limited mouth opening due to the involvement of the temporomandibular joint).
• Assessment of respiratory system (e.g., scoliosis-induced restrictive chest defects, impaired diaphragm function due to spinal cord injury).
• Assessment of cardiovascular system. Fitness level is the deciding criteria for the need for further assessment. Spine and orthopedic surgery patients may have limited exercise tolerance due to other reasons (pain) and therefore complicate this assessment.
• Assessment of neurologic status, including existing neurologic deficiencies and active range of motion and strength of extremities.
• Assessment of pain and psychological burden in order to establish realistic postoperative expectations for pain and function.
• Review of past medical, surgical, and anesthetic history, allergies, and current medications with special attention to chronic opioid use and disease modifying drugs such as steroids, methotrexate, and nonsteroidal anti-inflammatory drugs.
• Hematologic profile and anticoagulant or antiplatelet drug use. Management of anemia and modification or discontinuation of the drugs affecting coagulation will likely be required.
• Assessment and improvement of nutritional status (e.g., serum albumin concentration).
• Planning for the postoperative care transition, intensity of care, and eventual discharge destination.

“Incomplete” traumatic spinal cord injuries (i.e., neurologic function below the injury level is partially preserved) are eight times more common than “complete” injuries (i.e., no neurologic function is present below the injury level), highlighting the importance of avoiding secondary neurologic injury during perioperative anesthesia care.
II. Surgery to Spine
A. Spinal Cord Injuries
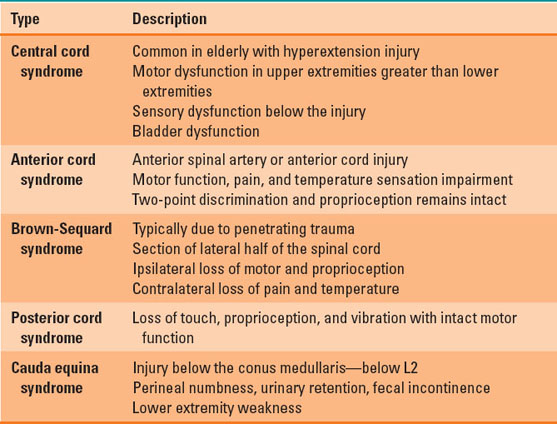
The incidence of traumatic spinal cord injury (TSCI) and its average patient age are increasing, with falls now being the most common overall cause of such injuries. Injury most commonly affects the cervical column (57.4%), followed by thoracic (21.5%) and lumbosacral (13.8%) levels. The initial trauma can result in irreversible neuronal damage (primary injury) that is “complete” (no spinal cord function distal to the injury) or “incomplete” (partial function distal to the injury) and is only modifiable by prevention. Secondary injury starts within minutes and is exacerbated by inflammation and edema, leading to further ischemia and neurologic deterioration. Focused medical care aims to limit its extent with careful coordinated management strategies (1). The American Spinal Injury Association score is used to classify the neurologic injury severity (Table 26-1). Incomplete neurologic injuries are eight times more common than complete injuries and may have a variety of presentations (Table 26-2).
Table 26-1 American Spinal Injury Association (ASIA) Spinal Cord Injury Classification
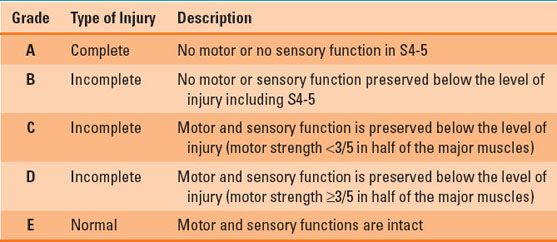
Table 26-2 Incomplete Spinal Cord Injury Syndromes
Hemodynamic Management
Hypotension is common after TSCI and may be associated with intravascular volume depletion, tension pneumothorax, pericardial tamponade, and neurogenic shock. Neurogenic shock is characterized by hypotension with or without bradycardia due to loss of sympathetic tone when the injury occurs at the level of T6 and above. Maintaining mean arterial blood pressure at 85 to 90 mm Hg with the help of intravenous volume expansion, vasopressors, and inotropes is required for the optimization of spinal cord perfusion. Chronotropic agents or cardiac pacing may be required for the treatment of associated bradycardia.
Decompressive Surgery
Decompression of the injured spinal cord and stabilization of the spinal column is generally required after TSCI. It follows the initial resuscitation and surgical management of other immediate life-threatening conditions such as traumatic brain injury or intra-abdominal hemorrhage. When performed within 24 hours of injury, it is shown to improve neurologic recovery sixfold.
B. Scoliosis
Scoliosis is defined as an abnormal lateral curvature of the spinal column in the coronal plane. It is frequently accompanied by a rotation deformity (Table 26-3). Its severity is assessed by the measurement of Cobb’s angle (Fig. 26-1). Despite the application of a brace, progression of the curve to a Cobb’s angle >45 degrees generally requires surgery to stop further deterioration. When untreated, progressive scoliosis may lead to severe back pain, restrictive ventilatory defects, hypoxia, hypercarbia, and pulmonary hypertension.
 VIDEO 26-1
VIDEO 26-1
Scoliosis
Table 26-3 Etiology of Scoliosis
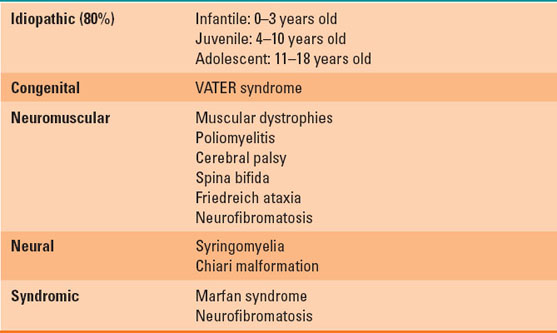
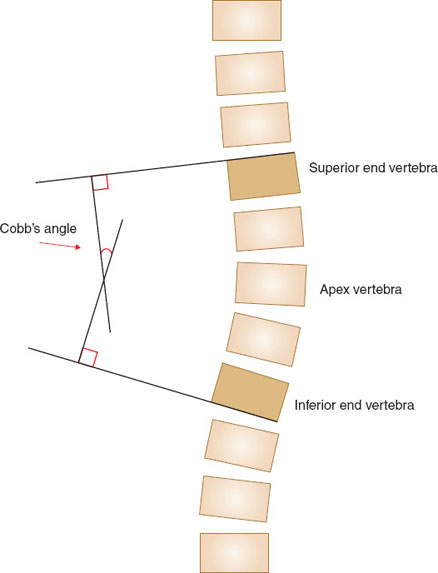
FIGURE 26-1 Cobb’s angle is the angle between the two lines drawn (1) parallel to the superior border of the superior end vertebra and the (2) inferior border of the inferior end vertebra.
C. Degenerative Vertebral Column Disease
Adult degenerative spine disease is a major cause of chronic pain and disability. Spondylolysis refers to a radiculopathy or myelopathy resulting from osteophyte formation and intervertebral disc disease. It is found in about 6% of adults, is twice as common in males, and usually occurs bilaterally near L5. Its etiology is uncertain (>50% due to repetitive spine trauma), and it is generally managed nonoperatively. Spondylolisthesis refers to a loss of vertebral alignment as a result of forward displacement of one vertebra over another and most commonly affects the lumbosacral region. Management is generally conservative (physical therapy, multimodal analgesia, and epidural steroid injections), although progressive myelopathy, neuropathy, or loss of bowel or bladder control are all indications for surgical decompression with or without fusion.
D. Anesthesia for Spine Surgery
Spine surgery is required for the correction of vertebral column deformities and for decompression of nerves and spinal cord due to impingement from diseases of the disc, bone, tumors, and trauma.
Airway
Cervical spine instability requires measures to minimize neck movement during tracheal intubation. All airway instruments and techniques can potentially cause movement in the cervical spine, but these are typically negligible. Thus, when carefully performed, no single technique has been shown superior in terms of neurologic outcomes. TSCI patients who require tracheal intubation in urgent or emergent circumstances and in the absence of other difficult airway issues can generally be safely managed with rapid sequence induction with bimanual cricoid pressure (see Chapters 20 and 32) and manual inline cervical spine stabilization (so that the front of the cervical collar can be temporarily removed to facilitate laryngoscopy). Video laryngoscopy may provide less neck movement and can be used for tracheal intubations in both awake and unconscious patients, particularly those with features predicting difficult laryngoscopy (e.g., large neck circumference, limited mouth opening). Fiberoptic intubation is theoretically associated with minimal cervical spine movement. “Awake” fiberoptic intubation is typically reserved for those with a predicted difficult intubation where maintenance of spontaneous breathing would be advantageous.

In patients with cervical spine instability, no single airway management technique has been shown superior in preventing rare, tracheal intubation-related spinal cord injury.
Positioning
Most spine surgery patients require prone positioning, although certain cervical or thoracic anterior cord lesions may require supine or lateral positioning, respectively. The sitting position is preferred for some high posterior cervical surgeries. All such positioning requires careful attention to details of patient anatomy, vascular access lines, and monitoring equipment. This is facilitated by adequate numbers of personnel and proper equipment training for safety (Figs. 26-2 and 26-3).

FIGURE 26-2 Prone positioning on Wilson frame (left) and Jackson table (right) with foam pillow and Prone View head rest, respectively.

FIGURE 26-3 Correct placement of the arms in prone position. Arms can be positioned either in swimmer position (left) or tucked at the sides (right), with the axillae and ulnar grooves free from direct pressure and the wrists and elbows padded.
The endotracheal tube and all vascular access lines should be secured adequately before turning from the supine to another position. A soft bite block will prevent tongue or endotracheal tube biting. Special spine tables allow the prone abdomen to hang free and reduce intraoperative bleeding by minimizing compression of abdominal contents (and attendant increases in vena cava and epidural venous pressure) as well as facilitating positive pressure ventilation. Slight reverse Trendelenburg tilt also limits the venous back pressure and bleeding. Foam or gel-based face pillows or Mayfield pins are used to provide pressure-free positioning of the face, with the neck in a neutral position to prevent neurologic injury.
Monitoring and Access
In addition to standard American Society of Anesthesiologists monitors, an arterial catheter provides continuous blood pressure monitoring and facilitates blood sampling in selected cases of anticipated hemodynamic instability or large blood loss. At least two peripheral intravenous lines are ideal due to the restricted intraoperative extremity access that occurs with cervical spine procedures with arms tucked at the sides. Central venous catheterization may be helpful for resuscitation and aspiration of intracardiac air if an air embolism occurs.
Anesthetic Technique
General anesthesia is required for most spine procedures. Because volatile anesthetics have variable effects on evoked potential monitoring of spinal cord function, total intravenous anesthesia is usually preferred in such cases, either alone or in combination with a low dose (<1% minimum alveolar concentration) volatile agent (Table 26-4).
Table 26-4 Commonly Used Anesthetic Agents in Spine Surgery
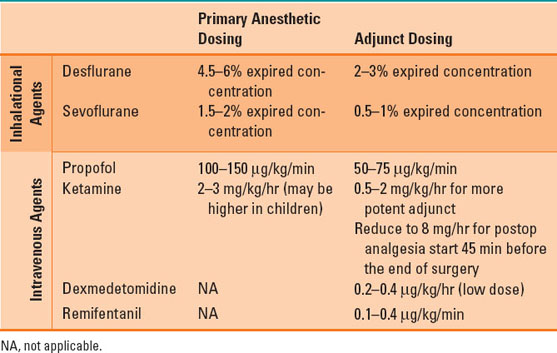
Table 26-5 Intraoperative Neurophysiologic Monitoring Modalities
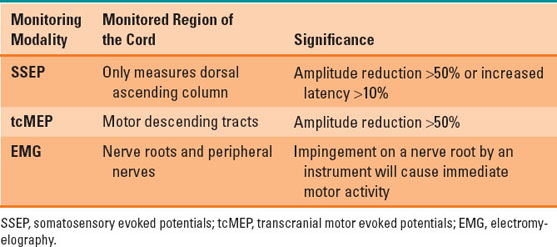
E. Spinal Cord Monitoring
Intraoperative neurophysiologic monitoring of motor or sensory-evoked potentials in the central nervous system is used during spinal surgery to detect unintended spinal cord injury. It is also used to guide surgical and medical interventions to avoid permanent neurologic injury. Multimodal neurophysiologic monitoring (Table 26-5) is sensitive and specific to detect intraoperative neurologic injury, but evidence that it reduces the incidence of new or worsening neurologic deficits is weak (2).

Prior to the advent of modern neurophysiologic monitoring of spinal cord function with motor- or sensory-evoked potentials, intraoperative assessment of spinal cord function was performed by the “wake-up test,” transiently reducing anesthetic depth during the surgical procedure to observe patient extremity movement in response to verbal commands.
Management of Acute Evoked Potential Signal Changes
If an acute change in neurophysiologic monitoring is detected, the following steps should be taken to identify its cause and reverse the abnormality:
• Rule out surgical and equipment-related factors; communicate with the surgeon and neuromonitoring team.
• Reposition the patient (maintain natural alignment of spinal column).
• Correct hypotension, metabolic abnormalities, severe anemia, and hypo- or hyperthermia.
• Raise mean arterial blood pressure >85 mm Hg to increase spinal cord perfusion.
• Turn off inhalation agent and switch to total intravenous anesthesia.
• Consider steroid infusion.
F. Blood Loss Prevention Strategies
Blood loss can be significant during spine surgery, with up to 80% of patients requiring an intraoperative transfusion. Perioperative blood loss and blood transfusion have potential negative consequences. Thus, various techniques have been proposed to minimize blood loss and blood product transfusion in this setting (3).
Preoperative Hemoglobin Optimization
Preoperative hemoglobin levels of 12 g/dL for females and 13 g/dL for males serve as thresholds for anemia that generally require further attention in the preoperative period. Laboratory evaluation, diagnosis, and treatment of existing anemia should occur before elective orthopedic procedures through correction of nutritional deficiencies, use of recombinant human erythropoietin, and oral or intravenous iron supplementation.
Antifibrinolytics
Tranexamic acid is the most common lysin analogue used as an antifibrinolytic to decrease perioperative blood loss and transfusion requirements through the inhibition of clot degradation. Its use is contraindicated in cases of known allergy, history of thromboembolic disease, and pre-existing seizure disorders. Potential adverse effects include thromboembolic events, seizures, and vision changes. The recommended dosing regimen is a 1-g bolus over 10 minutes following by an infusion of 1 g over 8 hours.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








