Joseph Louca
Sofia Maldonado-Villalba
I. General Considerations
The anesthetic management of otolaryngologic (ORL) surgery is complex. Many variables must be considered, including understanding the surgical indications and procedures. Depending on the operation, the anesthesiologist may jointly manage the airway with the surgeon. Additionally, airway anatomy may be distorted by tumor, infection, trauma, congenital abnormalities, radiation exposure, or prior surgery. Age-specific differences in anatomy and physiology, along with existing comorbidities, must also be considered.
Assessing the airway extends beyond the physical examination. Familiarity with airway imaging, particularly computed tomography and magnetic resonance imaging, is critical. Review the digital videos of airway fiberoptic examinations if they are available. If they are not available, the anesthesiologist may consider performing a fiberoptic examination of the airway under topical anesthesia prior to induction.
The selection and dosage of anesthetics and adjuvant medications should be tailored to the procedure being performed. Patients undergoing ORL procedures must also be carefully monitored for blood loss, which can be underestimated due to spillage onto the surgical field, swallowing, and distance of the surgical field from the anesthesiologist.
Topical `–agonists for vasoconstriction can cause hypertension and increased blood flow to the pulmonary circulation. This can be associated with pulmonary edema and death, especially if patients are subsequently treated with β-blockers because of their negative inotropic effects. Given the short duration of action of topical vasoconstrictors, moderate hypertension can be allowed to self-resolve or it can be treated by increasing the depth of anesthesia. Direct vasodilators are the proper treatment for a severe hypertensive response to topical vasoconstrictors.
II. Anesthetic Considerations in the Pediatric Population
A. Anatomy and Physiology
Diseases of the ear in children can be better understood by reviewing the anatomy and physiology of the middle ear and adjacent structures. The eardrum is a thin, well-innervated membrane sitting at the deepest part of the external auditory canal. It borders the middle ear laterally. The middle ear drains into the nasopharynx via the eustachian tube. During infancy, it drains poorly because of its small cross-sectional area, floppy cartilaginous walls, and the low angle it travels toward the nasopharynx. Additionally, its short length increases exposure of the middle ear to the mucous and bacteria of the nasopharynx. These factors increase the risk of otitis media, whose peak incidence occurs at 1 year of age. By age 7, the risk of otitis media is roughly that of adults.

During infancy, the eustachian tube drains poorly due to its small cross-sectional area, floppy cartilaginous walls, and the low angle it travels toward the nasopharynx. This explains why otitis media has a peak incidence in 1-year-old children.
B. Myringotomy and Tube Insertion
Myringotomy and ear tube placement requires general anesthesia (GA) to provide the surgeon with the stillness required for work under a microscope. The short length of the procedure and its noninvasive nature allow use of inhaled anesthetics alone. These procedures are often performed without intravenous (IV) access or securing the airway. Induction using a face mask with a mixture of oxygen, nitrous oxide (N2O), and sevoflurane can be followed by maintenance with sevoflurane. Positioning the head with 30 to 45 degrees of axial rotation allows adequate surgical access.

Myringotomy and ear tube placement, a short-duration procedure, is frequently performed under general anesthesia using a facemask and without intravenous access.
C. Tonsillectomy and Adenoidectomy
Tonsillar hypertrophy may be asymptomatic or lead to obstructive sleep apnea (OSA) and recurrent tonsillitis, which are frequent indications for removal of tonsils or adenoids. The tonsils grow rapidly between the ages of 1 and 3 and are often the largest between ages 3 and 7. Thus, this is the most common age range for this procedure.
 VIDEO 29-1
VIDEO 29-1
Tonsillectomy
The assessment of a child undergoing a tonsillectomy should include evaluating the overall respiratory function. Severe cases of OSA may warrant postoperative intensive care. The worst cases of OSA may also be complicated by pulmonary hypertension with cor pulmonale and may require pharmacologic cardiovascular support prior to induction.
In the setting of a mild or improving upper respiratory infection (URI), proceeding with the operation may increase the risk of respiratory complications. However, a delay often results in the patient returning to the physician until their next URI. Therefore, it may be sensible to proceed in the presence of a mild URI because complete optimization is rarely possible (1).
A variety of regimens exist for postoperative analgesia:
1. Given prior incision, acetaminophen (10 to 40 mg/kg rectally) for analgesia and dexamethasone (0.5 mg IV) for edema, postoperative nausea and vomiting (PONV), may reduce or eliminate the need for IV opioids.
2. If opioids are required, IV fentanyl (0.25 to 1.0 μg/kg) can provide effective relief while reducing the incidence or severity of emergence agitation.
3. Ibuprofen orally, given either pre- or postoperatively, is a safe and effective analgesic, although some surgeons are concerned with postoperative bleeding after its use (2).
D. Posttonsillectomy Hemorrhage
Although rare (<1% to 2% of patients), posttonsillectomy hemorrhage can be life-threatening. Risk factors include chronic tonsillitis, older age (>11 years old), intraoperative blood loss >50 cc, and hypertension. Primary hemorrhage occurs within 24 hours of the surgery. Secondary hemorrhage typically occurs within 5 to 10 days of the surgery, the time period when a fibrin clot sloughs off.
The management of posttonsillectomy hemorrhage includes addressing the airway, circulation, and breathing. Assess cardiovascular stability and obtain IV access. Examine the airway, look for active bleeding or a clot, and obtain the history of any bleeding expeditiously. Keep the patient leaning forward and face down to drain blood away from the laryngopharynx. When minor or recurrent bleeding is present, there is a significant risk (perhaps >40%) for severe hemorrhage due to relaxation of vasospasm or the displacement or lysis of a clot. One must notify the blood bank and prepare for surgery.
In the operating room (OR), a gauze soaked in 1:10,000 epinephrine should be available. Direct pressure can be applied to tonsillar fossae using a Magill forceps wrapped with gauze. Suction and airway equipment should also be available before the patient is placed supine. Children may not tolerate efforts at hemostasis while awake and may need sedation or GA before attempts are made. Ketamine may be an excellent choice. It has a low risk of respiratory compromise and hypotension in hypovolemic patients (3).
E. Emergencies or Stridor
Stridor, a high-pitched or musical breathing caused by obstruction of the larynx, is a medical emergency that must be considered life-threatening. Common causes include foreign body aspiration (FBA), epiglottitis, and croup (Table 29-1).

Stridor, a high-pitched or musical breathing caused by obstruction of the larynx, is a medical emergency and must be considered life-threatening.
FBA is a common problem in children, particularly ages 1 to 5, that can be difficult to diagnose unless the event is witnessed and reported. FBA may present with wheezing and coughing, decreased breath sounds, and stridor. It may also mimic common allergies, asthma, OSA, gastroesophageal reflux disease, bronchiolitis, or airway obstruction due to abscess or congenital anomaly. Although radiography may detect atelectasis and hyperinflation, it cannot rule out FBA when the aspirated body is radiolucent. If there is a high index of suspicion for FBA, rigid bronchoscopy may be the necessary next step (Fig. 29-1).
Table 29-1 Causes of Stridor
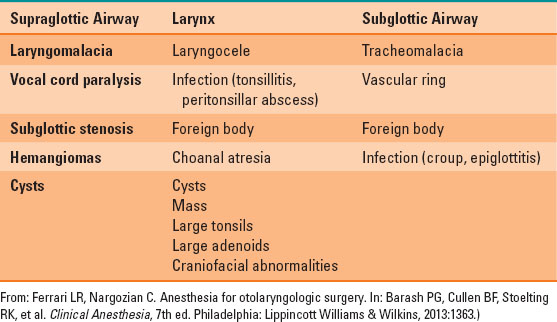
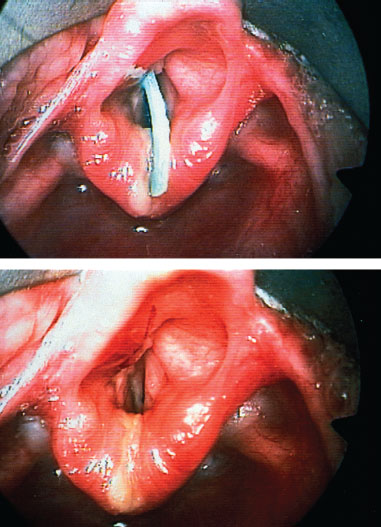
FIGURE 29-1 A radiolucent plastic strip is visible in the glottic inlet (just above the vocal cords) in a child who presented with inspiratory and expiratory stridor. Following foreign body removal, a small endothelial laceration is visible on the posterior surface of the epiglottis.
Epiglottitis, a life-threatening condition typically caused by a bacterial infection, often affects the epiglottis, aryepiglottic folds, arytenoids, and uvula. Its incidence has declined in the pediatric population due to widespread vaccination against Haemophilus influenzae B (Hib). Other bacteria, however, including Streptococcus pneumoniae, may also cause epiglottitis.

A chest x-ray may detect atelectasis and hyperinflation but it cannot rule out FBA if the aspirated body is radiolucent. When there is a high index of suspicion for FBA, rigid bronchoscopy may be necessary to establish a diagnosis.
Epiglottitis presents with stridor, drooling, odynophagia, outright avoidance of food and drink, dysphagia, or high fever. Other signs include malaise and agitation or a history of rapid symptom onset (within hours). An absence of Hib vaccination is of obvious concern. A child growing tired or lethargic suggests imminent respiratory collapse requiring securing the airway. Hypotension, hypoxemia, and bradycardia are also indications for rapid intervention.
Manage patients with suspected epiglottitis swiftly by obtaining radiologic images, monitoring with pulse oximetry, and administering supplemental oxygen. Do not agitate the patient prior to a procedure as it may lead to laryngospasm.
Keep the child upright during transport and proceed directly to the OR for an inhaled anesthetic induction with continuous positive airway pressure ventilation. After induction and IV line placement, weigh the benefit of preventing laryngospasm with a neuromuscular blocking agent against the risk of abolishing spontaneous respiration should tracheal intubation fail. For direct laryngoscopy, a curved Macintosh blade placed gently into the vallecula is likely the best approach. Prevent contact with the epiglottis as this may induce bleeding or swelling. An endotracheal tube 0.5 cm smaller in diameter than would normally be age appropriate should be placed due to the likelihood that edema has reduced patency of the airway. Smaller tubes should also be available.
Have atropine and succinylcholine ready for intramuscular administration to treat cardiac depression or laryngospasm. Alternative airway management plans are essential, and they include having immediate access to rigid bronchoscopy, emergency tracheostomy, or cricothyroidotomy.
Postoperative sedation and mechanical ventilation allow time for airway inflammation to subside. The infection must also be cultured and treated. Extubation should only occur after inspection reveals that the swelling and friability of airway tissues has decreased. A leak test may be helpful in determining readiness.

Laryngotracheobronchitis, also known as croup, may cause stridor; however, it tends to have a milder course than epiglottitis.
Laryngotracheobronchitis, or croup, is another cause of stridor, although it tends to have a milder course than epiglottitis. Croup presents with a barking, high-pitched cough and less severe systemic involvement. Consider croup in a vigorously coughing, alert toddler with a hoarse voice. For croup in an otherwise healthy child, it is unlikely that intubation and mechanical ventilation will be necessary.
III. Anesthesia for Adult Otolaryngologic Surgery
A. Middle Ear and Mastoid
Common procedures for adult middle ear and mastoid issues include stapedectomy, tympanoplasty, mastoidectomy, and myringotomy. Intraoperative considerations for middle ear and mastoid surgery include preservation of the facial nerve, prevention of brachial plexus or cervical injuries, and management of the adverse effects of N2O.
 VIDEO 29-2
VIDEO 29-2
Tympanoplasty and Mastoidectomy
Facial nerve integrity can be monitored and maintained with intraoperative electromyography and avoidance of neuromuscular blocking agents. Preoperative evaluation of cervical spine range of motion is essential to prevent injuries to the brachial plexus and cervical spine. Avoid extreme neck extension or rotation during surgery.
N2O can result in increased middle ear pressure if the eustachian tube is not patent. Sudden discontinuation of this gas leads to rapid absorption of N2O, creating negative pressure that may result in changes to middle ear anatomy, rupture of tympanic membrane, disruption of grafts, and PONV.
B. Nasal and Sinus Surgery
Nasal and sinus surgeries can be performed under local anesthesia with sedation or under GA when there is concern regarding arterial damage or advancing into the intracranial space, the latter being a concern during endoscopic sinus surgery.
Minimize intraoperative bleeding with intranasal vasoconstriction, elevation of the head to facilitate venous drainage, and induced mild hypotension.
C. Maxillofacial Trauma and Orthognathic Surgery
High-speed impact trauma, with or without external evidence of injury, is frequently associated with life-threatening injuries. The anesthetic plan must consider the possibility of cervical spine injuries and skull fractures. Cervical spine stabilization prior to intubation and oral versus nasal intubation (contraindicated in LeFort III fracture) are important considerations. Orthognathic surgery for reconstruction of facial skeletal malformations is often achieved by performing LeFort or mandibular osteotomies, so understanding of these procedures is beneficial.
D. Craniofacial Bone Structure
Knowledge of basic craniofacial bone structure is important. The facial skeleton comprises three parts. The lower third is the mandible. The middle portion includes the zygomatic arch of the temporal bone, zygomaticomaxillary complex, maxilla, nasal bones, and orbits. Lastly, the superior portion comprises the frontal bone.
E. Temporomandibular Joint Arthroscopy
Temporomandibular joint arthroscopy is indicated when there is displacement of the temporomandibular joint cartilage, causing clicking, trismus, fibrosis, or osteoarthritis. Intubation may be oral (if immobility is achieved with GA) or with nasal fiberoptic assistance if the patient is in trismus. Swelling around the surgical site due to irrigation may result in partial or complete airway obstruction.
 VIDEO 29-3
VIDEO 29-3
Temporomadibular Joint Assessment
F. Surgery of the Airway
Suspension Laryngoscopy and Microlaryngoscopy
Suspension laryngoscopy and microlaryngoscopy provide direct access and visualization of the airway, while protecting the trachea and maintaining ventilation and oxygenation.
Jet ventilation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








