Axial sonoanatomy of the paravertebral space.
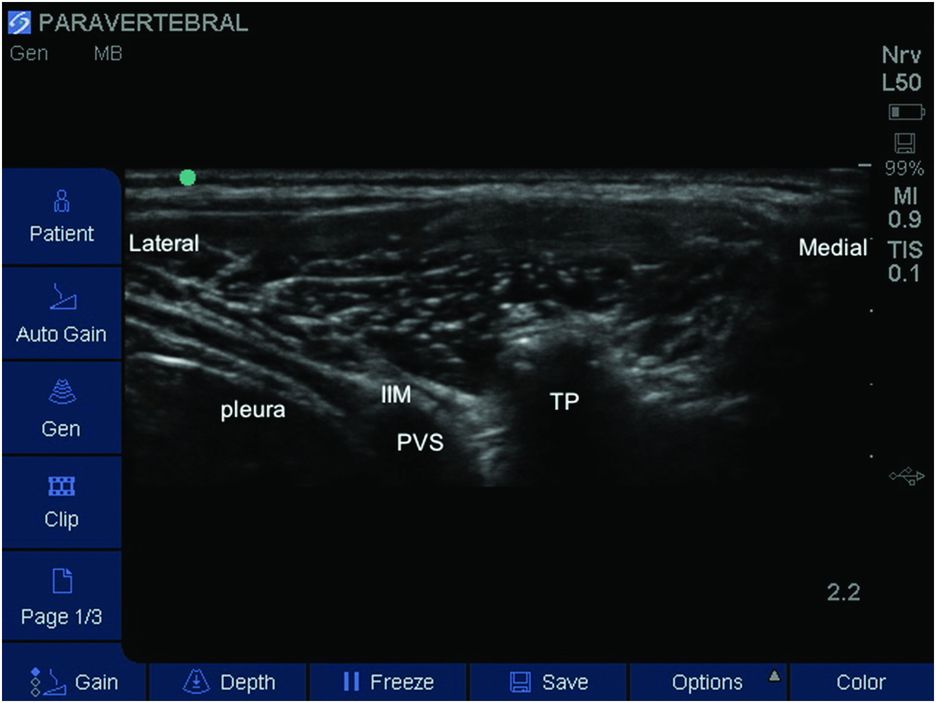
Labeled axial sonoanatomy of the paravertebral space (PVS). IIM, internal intercostal membrane; TP, transverse process.
Landmarks
For unilateral paravertebral block the patient is placed in the lateral position with the operative side uppermost (Figure 17.3). For bilateral blocks the child is positioned either in prone position or in lateral position with the shoulder tilted forward forming a 45 degree angle with the bed to allow easy access to both sides of the back. The bed can be further tilted to optimize block performance (Boretsky et al., 2013). The appropriate vertebral level – T5 for thoracic procedures and T10 for abdominal surgeries – is identified either with the surface landmarks or using ultrasound to give a sagittal view (Figure 17.4), and marked. The ultrasound probe is placed over the marked spinous process in the midline and rotated perpendicular to the spinal column. Then, the probe is moved laterally to obtain an axial or transverse view of the transverse process and the parietal pleura (transverse paramedian view) (Figure 17.3). Probe tilting, rotation, and/or slide may be necessary to obtain a clear view of the important structures.

Lateral patient position and probe placement.
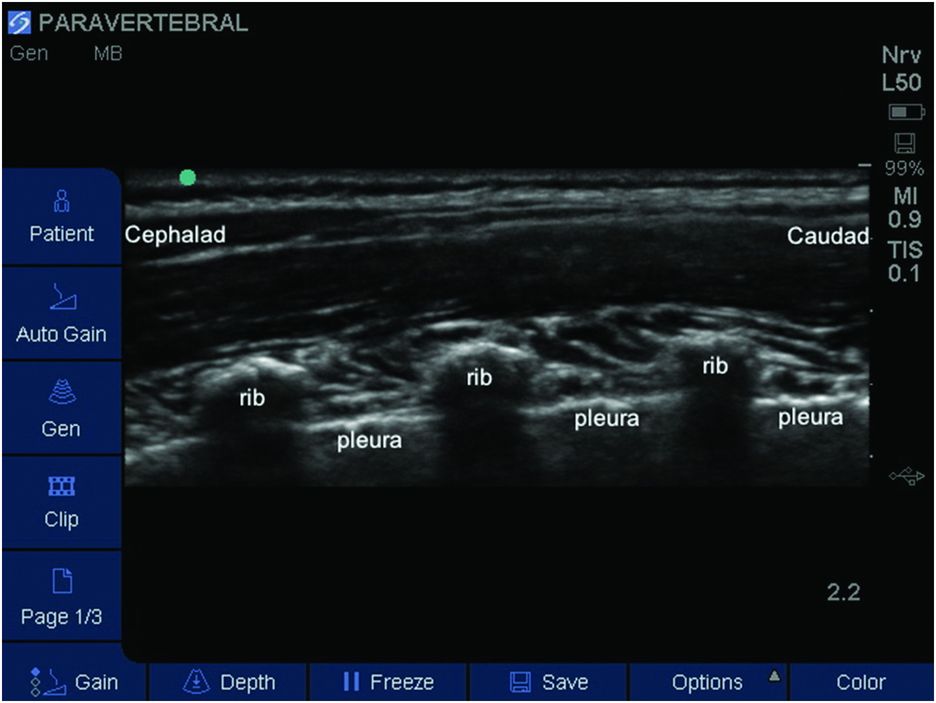
Labeled sagittal sonoanatomy of the paravertebral space. The probe has been moved slightly lateral to the midline to reveal the ribs and the relevant level. The pleural depth can be easily measured.
Block performance
In the pediatric population, a high frequency linear probe (>10 MHz) is appropriate, although some advocate a probe configuration based on age, weight, and body mass index (Boretsky et al., 2013). The ultrasound probe is positioned and manipulated until a clear image of the transverse process, the parietal pleura, and the internal intercostal membrane (lateral continuation of the costotransverse ligament) is obtained. Using an in-plane approach from lateral to medial, an appropriately sized Tuohy needle is introduced 1–2 cm from the lateral edge of the probe. The needle is advanced carefully under constant direct vision until the tip of the needle pierces the internal intercostal membrane and enters the paravertebral space (Figure 17.5). Correct position of the needle tip can be confirmed by resistance-free injection of 1 or 2 ml of normal saline and anterior displacement of the parietal pleura. After negative aspiration the LA can be injected and/or the catheter inserted. When placing a catheter, the bevel of the Tuohy needle should be oriented cranially in order to direct the catheter in the cephalad direction. Catheters should be inserted no more than 2–3 cm beyond the needle tip, and correct catheter position is confirmed with additional anterior displacement of the parietal pleura following normal saline administration. Catheters may be tunneled. Although, the only pediatric study using ultrasound for catheter placement reported no catheter malfunction (Boretsky et al., 2013), adult cadaver studies suggest a high incidence of catheter misplacement into the epidural, mediastinal, or pleural spaces (Luyet et al., 2009, 2011). The optimal volume of LA in a single injection was suggested as 0.5 ml/kg per side (Lönnqvist and Hesser, 1993), which covers at least 5 thoracic paravertebral segments. However, a recent pediatric cadaver study shows that smaller volumes of 0.2 and 0.3 ml/kg are sufficient to cover 5 and 6 segments, respectively (Albokrinov and Fesenko, 2014). When a catheter is placed, an infusion rate of 0.5 mg/kg/h is appropriate. LAs administered are: levobupivacaine 0.25%, bupivacaine 0.25%, or lidocaine 1% – all with added epinephrine 1:200 000 (Coté et al., 2013); ropivacaine 0.5% intraoperatively and 0.1% or 0.2% post-operatively (Boretsky et al., 2013).
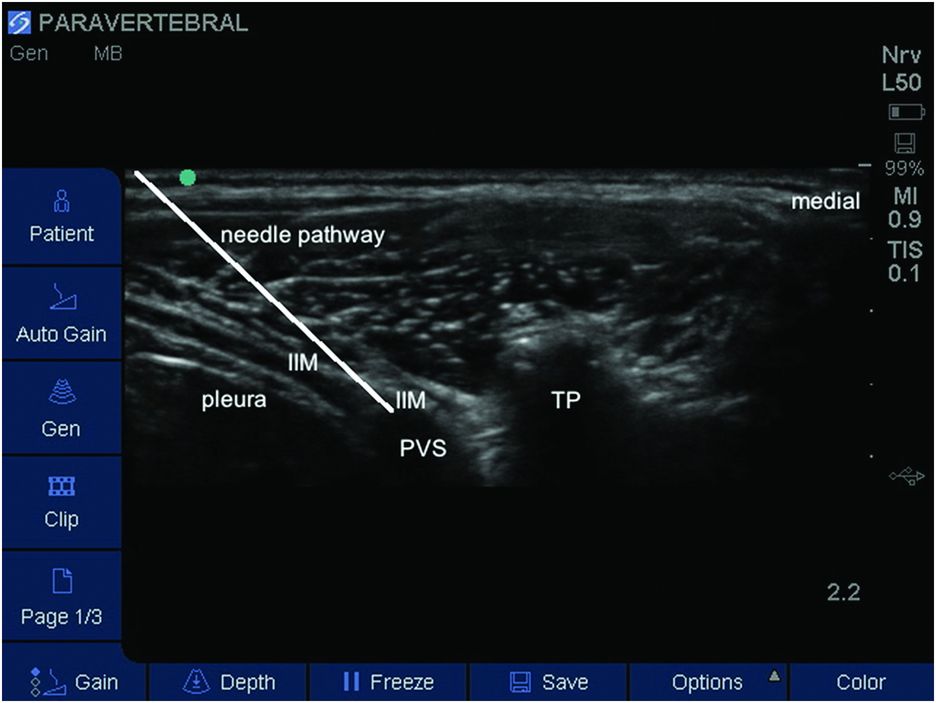
Lateral in-plane needle approach. The needle is advanced carefully under constant direct vision until the tip of the needle pierces the internal intercostal membrane and enters the paravertebral space (PVS). IIM, internal intercostal membrane; TP, transverse process
Post-operative care
Since the effect of a single injection paravertebral block lasts up to 8 hours, oral and/or intravenous analgesics need to be prescribed and the paravertebral block should be considered as part of a multimodal analgesia regimen. When a catheter is placed, the LA infusion is started either in the operating room or in the post-anesthesia care unit (PACU) according to local protocols. Post-operative pain should be assessed regularly using either the FLACC scale (Merkel, 1997) or the numeric rating score (NRS), and managd accordingly. A recent study shows that ambulatory continuous paravertebral nerve block is feasible for pediatric patients (Visoiu et al., 2014).
Use an in-plane approach to visualize needle advancement and needle tip. Connect a fluid-filled tubing and syringe to the needle while advancing the needle. In case of an inadvertent pleural puncture it prevents conversion to pneumothorax.
Thread the catheter no more than 2–3 cm beyond the needle tip.
Suggested reading
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








