Sonoanatomy for supraclavicular block.
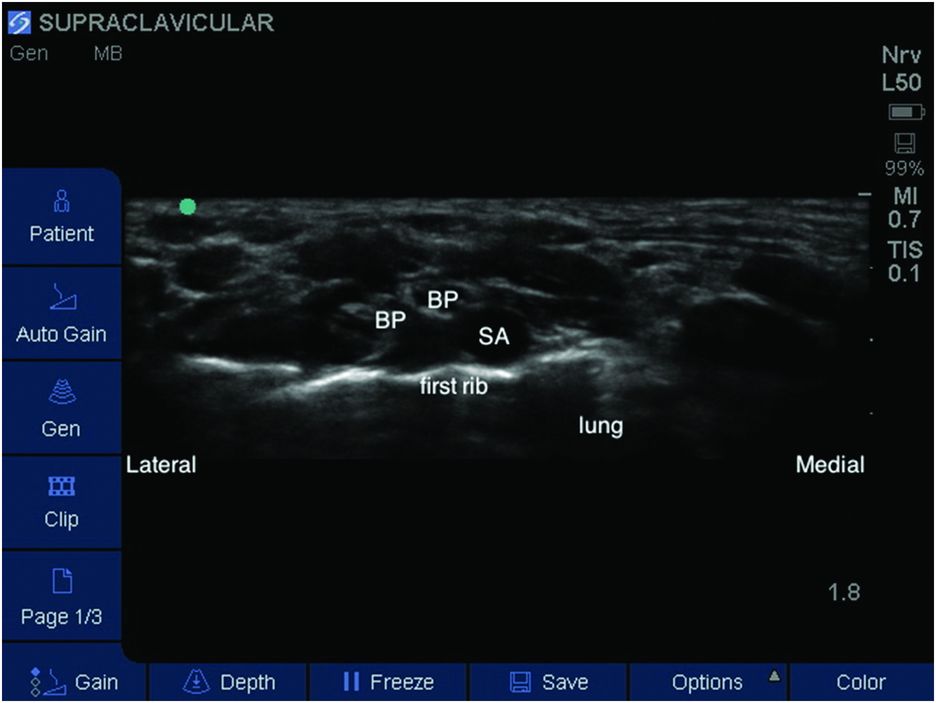
Labeled sonoanatomy for supraclavicular block – brachial plexus divisions (BP), subclavian artery (SA).
Landmarks
The patient should be placed in the supine position with the head turned to the contralateral side. A roll between the scapulae may be necessary in smaller patients. The height of the bed should be set at an ergonomically comfortable level for the anesthesiologist. Placement of the probe is in a coronal-oblique axis along the superior border of the distal clavicle (Figure 8.3). As the probe moves medially, the brachial plexus will come into view lateral to the subclavian artery, above the first rib.

Patient position, probe placement, and in-plane needle technique.
Block performance
A linear, high frequency probe should be placed in the supraclavicular fossa, in the coronal-oblique axis, along the superior border of the distal clavicle. As the probe is guided medially along the clavicle, the hypoechoic subclavian artery should be identified and the brachial plexus will come into view. Color Doppler should be used to scan for vasculature. With the plexus visualized, the probe should be held in place so that the plexus, first rib, and subclavian artery are all in view. A 22-gauge, 50 mm needle is introduced in-plane from the lateral side to approach the brachial plexus (Figure 8.4). Direct visualization of needle movement is necessary to avoid entering nerve bundles, vasculature, or pleural space. Once in close proximity to the plexus, the syringe should be aspirated as a safety measure to protect against intravascular injection. A small amount of LA should be injected incrementally with re-aspiration of the syringe every 1–2 ml. Redirection of the needle, under direct visualization, with deposition of LA around the entire plexus improves block success and decreases latency. Care should be taken to visualize the needle in-plane at all times, avoiding arterial puncture and placement of the needle below the plexus in the area of the pleura.
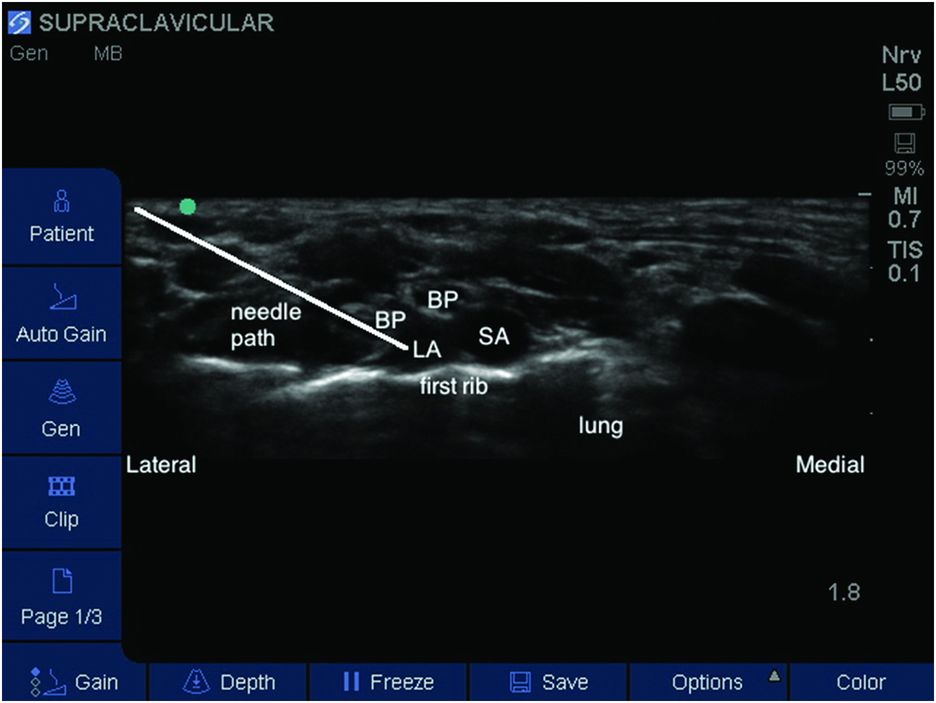
Needle pathway (highlighted) and local anesthetic (LA) deposition – brachial plexus divisions (BP), subclavian artery (SA).
A total of 0.25–0.50 ml/kg of 0.25% bupivacaine, 0.25% levobupivacaine, or 0.2% ropivacaine can be used. In patients under 6 months of age, the dose should be reduced by 50%.
Post-operative care
In a patient who has received a supraclavicular block, the extremity must be protected until full function and sensation have returned to the extremity. This includes padding the extremity while lying in bed, or placing the arm in a sling should the patient ambulate. If a child is to be discharged after a day case with residual block, proper education of the parents as well as written instructions are necessary regarding how to care for and protect a weak and numb upper extremity. The parents must also understand how to safely administer oral analgesics prior to the block wearing off to smoothly transition to an oral pain management regimen.









