Sonoanatomy of the infraclavicular region.
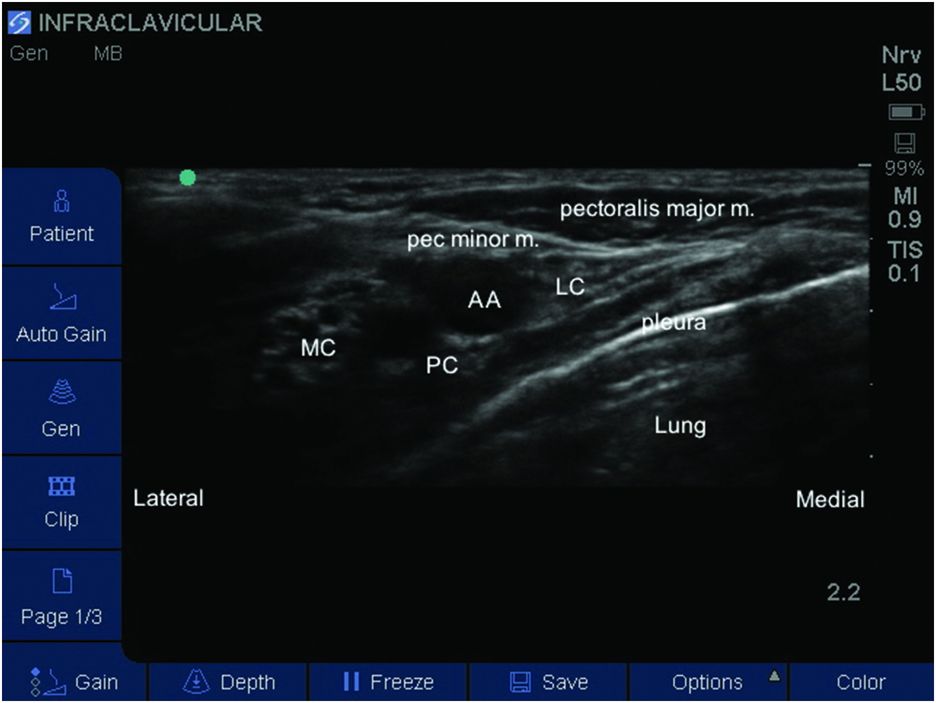
Labeled sonoanatomy of the infraclavicular region. AA, axillary artery; LC, lateral cord; MC, medial cord; PC, posterior cord.
The key anatomic structure to identify is the axillary artery lying posterior to the pectoralis major and minor muscles (Figure 9.2). Although a great deal of anatomic variability exists, the lateral cord is typically located superior to the artery while the posterior and medial cords are located posterior and inferior to the artery respectively.
Landmarks
The patient should be placed in the supine position. The transducer is placed in a parasagittal position below the clavicle on the medial aspect of the coracoid process (Figure 9.3). Depending on the size and body habitus of the child, a probe with a short linear length such as 25 mm may be required. Some adjustment of the probe in multiple planes may be necessary to achieve a satisfactory view of the artery and the surrounding cords. Abduction of the arm to 90 degrees may be helpful by moving the acromioclavicular junction superiorly.

Probe position, which may need to be adjusted to obtain the best view that still permits a lateral to medial needle approach. Abduction of the arm may help by moving the coracoid process superiorly and laterally.
Block performance
In younger or thin children a high frequency linear probe may be sufficient for visualization of the infraclavicular fossa while a lower frequency curved array probe may be necessary in larger children and adolescents to visualize a deeper infraclavicular fossa. Color Doppler may be useful to verify the position of the axillary artery and vein.
The lateral cord is seen as a hyperechoic structure as is the posterior cord, which can be seen posterior to the axillary artery at the 6 o’clock position. The medial cord may be more difficult to visualize but the injection of 1–2 ml of LA anterior to the artery may improve its localization.
For single injection a 22-gauge needle can be used and the length of needle (50–100 mm) can be chosen based on the child’s size and plexus depth. A 25 mm BP needle may be sufficient in infants and small children while a 100 mm BP needle may be required to reach the infraclavicular fossa in adolescents.
The needle is then inserted between the coracoid process and the superior portion of the ultrasound probe. The needle is advanced in-plane through the pectoralis major and minor muscles (Figure 9.4). Because of the steep needle angle required to reach the infraclavicular BP, the needle image may not be very clear so care must be taken to monitor tissue displacement as the needle is advanced in an effort to avoid puncturing the artery. The LA is injected in small 3–5 ml increments around the cords ensuring that there is adequate perivascular spread of the LA, especially medially and laterally around the artery. Current recommended volumes are 0.5 ml/kg of 0.2% ropivacaine or 0.25% bupivacaine, although these volumes may reduce with the increasing experience with ultrasound to guide LA deposition for this block.
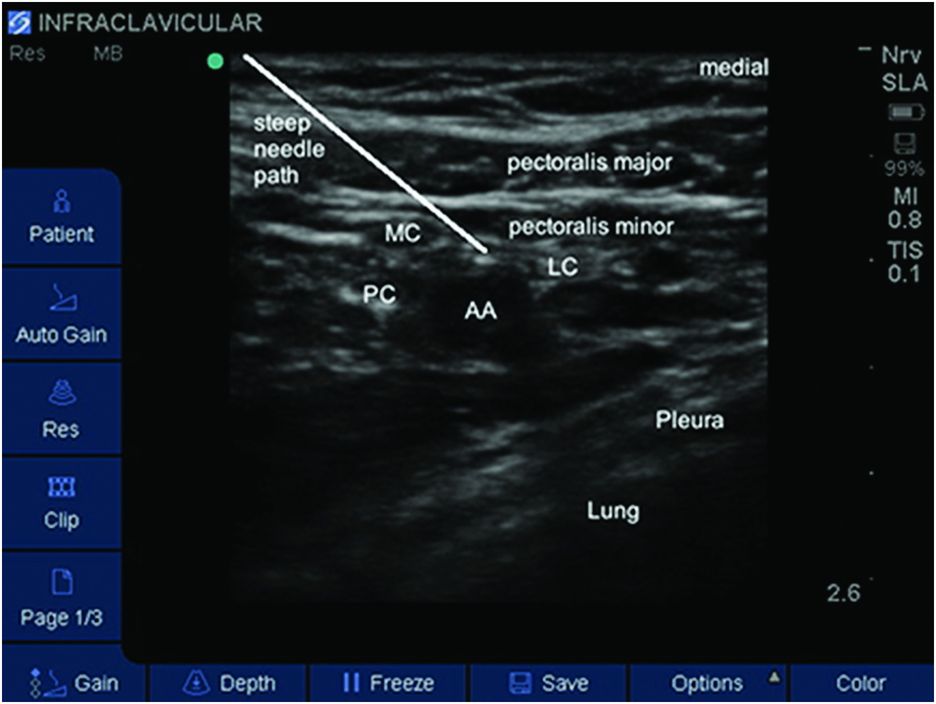
Needle path highlighted. In practice the steep angle required may make needle visualization difficult. AA, axillary artery; LC, lateral cord; MC, medial cord; PC, posterior cord.
If placing a catheter, the use of a short 50 mm Touhy needle in infants and younger children and a 100 mm Touhy needle in young adults would be appropriate. Ideally, the catheter should be placed at the 6 o’clock position adjacent to the posterior cord where the infusate can reach both the medial and lateral cords. Several methods have been described to verify catheter position including the injection of agitated 5% dextrose (Dhir and Ganapathy, 2008) or the injection of a small amount of air (Kan et al., 2013). Once the catheter is in position, LA is injected with ultrasound visualization in 3–5 ml increments following careful aspiration of the catheter. In order to ensure complete BP coverage, medial and lateral extension of the local anesthetic around the axillary artery should be present. The catheter is then carefully secured to the patient. A single drop of dermabond applied to the catheter insertion site helps reduce the possibility of catheter dislodgement and/or pericatheter leakage (Gurnaney et al., 2011). The catheter can then be affixed to the patient using a sterile non-occlusive dressing.
For continuous peripheral nerve blockade an infusion of ropivacaine (0.4 mg/kg/h) or bupivacaine (0.4 mg/kg/h) is commenced with a typical maximum infusion rate of 8–10 ml/h.
Post-operative care
Children and adolescents can be safely discharged home following regional anesthesia (Gurnaney et al., 2014). In the case of single shot peripheral nerve block, it is important to prepare the patient’s parents for the eventual resolution of the block and the potential for increased pain and anxiety in the child. This can be quite alarming to families if not adequately prepared, and a plan for oral analgesics should be available and reviewed with the family prior to discharge. Additionally, it is appropriate to follow up the patient who had a single shot nerve block the following day to confirm resolution of the sensory block and also to monitor for any complications. When a continuous perineural catheter is placed, we recommend daily follow-up phone calls or hospital visits for inpatients to monitor patient response until the catheter has been removed and the block has resolved (Gurnaney et al., 2014). This type of support can relieve parental concerns about managing LA infusions at home and provide a resource for families as they recover from their surgical procedure.









