Thoracolumbar spine.
Spinal cord
The spinal cord lies protected within the vertebral canal, encased in three layers of connective tissue structures known as meninges. The layer closest to the spinal cord is the delicate pia mater, attached directly to the spinal cord. Surrounding this is the arachnoid mater, which does not adhere to the pia mater, creating a space between the two, the subarachnoid space, filled with cerebrospinal fluid. The outermost layer is the dura mater, which lies against the arachnoid mater but has no attachment to it. The dura mater does not touch the bony vertebral canal, but is cushioned by fat and connective tissue, and is accompanied within this epidural space by a venous plexus.
The spinal cord passes through the magnum foramen and extends distally to between L1 and L2 (in the adult), although there can be variation between T12 and L3. During childhood development and growth, the vertebral column and spinal cord do not grow at the same speed, with the vertebral column extending at a faster rate, and, therefore, the distal end of the spinal cord appears to be more proximal in the vertebral canal in the adult compared to neonates where it extends to approximately L3 or L4. The spinal cord stops growing between the ages of 4 and 5 years; therefore, the tip of the spinal cord will appear progressively more proximal with continued skeletal growth until this ceases approximately between 16 and 18 years, at which point the spinal cord tip will approximate the level of L2. The terminal point of the spinal cord is cone-shaped (conus medullaris), and a connective tissue filament (the filum terminale) extends from this to anchor at the coccyx. The spinal cord has two large swellings along its length, corresponding to the areas associated with upper and lower limb spinal nerve emergence. The cervical enlargement corresponds to the regions where C5–T1 spinal nerves emerge, whilst the lumbosacral enlargement corresponds to the regions of L1 to S3 spinal nerve emergence.
Spinal nerves
Thirty-one pairs of spinal nerves arise from the spinal cord and emerge from the vertebral canal via the transverse foramina. There are 8 pairs of cervical nerves, 12 pairs of the thoracic region, 5 pairs of the lumbar region, 5 sacral pairs, and 1 single coccygeal pair. They all arise from the spinal cord as anterior and posterior bundles of rootlets, uniting to form the single spinal nerve before passing through the transverse foramen. The spinal nerves do not always arise at the same level from which they exit the vertebral canal, and distal pairs of spinal nerves (especially those of the lumbar and sacral regions) travel some distance within meningeal membranes inside the vertebral canal before they exit. These “free” spinal nerves at the second to fifth lumbar levels, all sacral levels, and the coccygeal level, form the cauda equina, although the pairs of nerves continue to exit the vertebral canal (Figure 6.2). After this point, each spinal nerve splits into an anterior and posterior branch (anterior and posterior rami). The anterior ramus is the larger branch, and provides innervation of the majority of the body (except the head) whereas the smaller posterior ramus innervates the back.
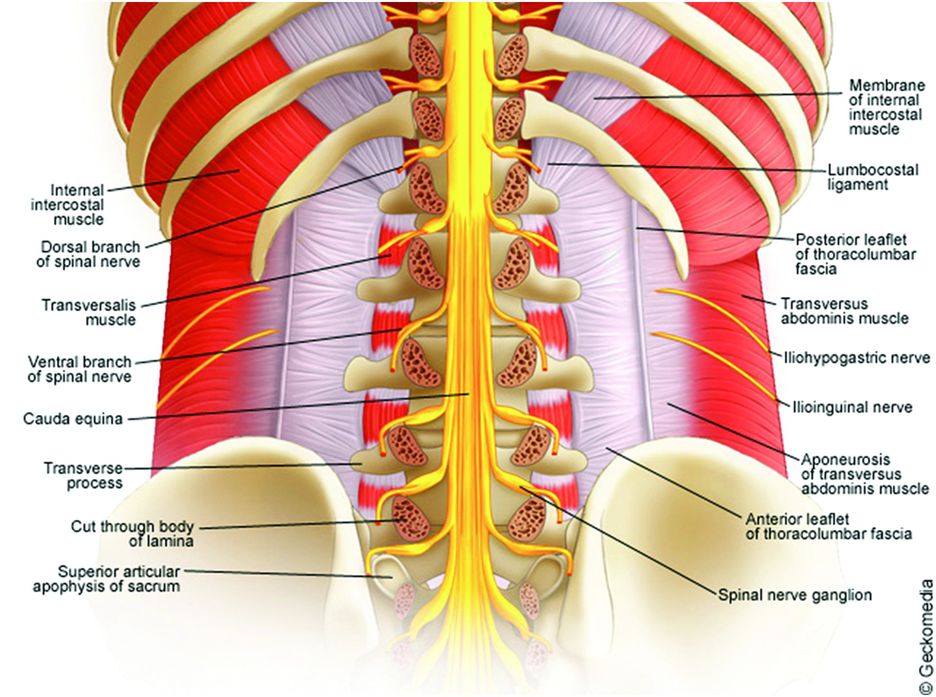
Cauda equine.
Ligaments
Ligaments connect adjacent vertebral bodies at a number of points as well as connecting transverse processes and laminae. The major ligaments are:
Anterior and posterior longitudinal ligaments
Ligamenta flava
Ligamentum nuchae
Supraspinous ligament
Interspinous ligaments.
Anterior and posterior longitudinal ligaments
These ligaments extend vertically along the anterior and posterior borders of the vertebral bodies. The anterior longitudinal ligament runs from the base of the skull to the anterior surface of the sacrum, joining the anterior aspects of the vertebral discs as well as the vertebral bodies. The posterior longitudinal ligament lies within the vertebral canal, attached to the posterior aspect of the vertebral bodies and discs. It begins at C2, where it is known as the tectorial membrane of the atlanto-axial joint, connecting this vertebra to the base of the skull.
Thoracic wall
The thoracic wall consists of thoracic vertebrae, intervertebral discs, ribs, sternum, and all the surrounding and interosseous musculature. The thoracic wall extends from the superior thoracic aperture at the level of the first rib and the upper border of the manubrium, to the inferior thoracic aperture at the border of the twelfth rib, the tip of the eleventh rib, the costal margin, and the distal point of the xiphoid process. At the posterior midline, the bodies of the thoracic vertebrae make up the posterior aspect of the thoracic wall.
Skeletal contribution
Thoracic vertebrae articulate with the 12 pairs of ribs posteriorly, whilst anteriorly the first 7 pairs of ribs articulate with the sternum. The next three pairs of ribs articulate anteriorly with the costal cartilages of the rib directly superior, whilst the final two pairs have no anterior articulation.
Between the ribs are the intercostal spaces in which are sited intercostal muscles as well as vessels and intercostal nerves. These latter structures run along the costal groove on the inferior border of each rib, usually with the vein most superior and closest to the rib, inferior to which is the artery, and inferior to the artery is the nerve, which on occasions is completely out-with the costal groove and, therefore, more at risk of damage. Directly overlying the intercostal spaces are muscles contributing to arm movement (Pectoralis major and minor, Subclavius), and superficial to these are the deep fascia, superficial fascia, and skin. Beneath the intercostal spaces and ribs lies the endothoracic fascia, separating the thoracic wall from the underlying pleura.
Muscular components
The roles of the muscles of the thoracic wall are to change rib and sternal position during breathing to create changes in thoracic volume and, therefore, thoracic pressures. The muscles of the thoracic wall are:
Levatores costarum
Serratus posterior superior and Serratus posterior inferior
Intercostals – external, internal, innermost
Subcostales
Scalenes
Transversus thoracis.
Levatores costarum
There are 12 pairs of these small muscles, arising from the tips of the transverse processes of C7–T11. The muscles pass inferolaterally to insert into the rib directly inferior to the vertebra from which they have arisen. They do not play a role in the inspiratory process but contribute to vertebral movement.
Serratus posterior superior and Serratus posterior inferior
Serratus posterior superior arises collectively from the lower border of ligamentum nuchae, the spinous processes of C7, T1–T3, and the supraspinous ligament. It passes inferolaterally and inserts into the upper borders of the second to fifth ribs. The muscle acts to elevate the second to fifth ribs during inspiration. Serratus posterior inferior arises collectively from the spinous processes of T11–L2 and the supraspinous ligament. It passes superolaterally to insert into the inferior borders of the ninth to twelfth ribs. It functions to pull the lower ribs down and backwards to aid in forced expiration, as well as contribution to trunk movement.
Intercostal muscles
These are made up of three elements within each intercostal space, known as (superficial to deep) external, internal, and innermost intercostals. Together they provide support for the ribs during breathing, as well as contribution to rib movement.
External intercostal muscles ––
there are 11 pairs of these muscles, each arising from the inferior border of ribs 1–11 and extending to the superior border of the rib directly below (ribs 2–12), running obliquely forwards and downwards. They are active during inspiration and elevate the ribs, widening the rib cage, and increase the dimensions of the thoracic cavity.
Internal intercostal muscles ––
the 11 pairs of these muscles arise from the inferolateral edge of the costal grooves of ribs 1–11 and extend to the superior margins of ribs 2–12, deep to the external intercostal muscles. The Internal intercostal muscles also run obliquely, but in the opposite direction to the external layer, i.e. posteroinferiorly, and are active during expiration.
Innermost intercostal muscles ––
these muscles arise from the anterior surfaces of the costal grooves and pass directly to the inner surface of the rib directly inferior, running in the same direction as the Internal intercostals. The neurovascular bundles, which run in the costal grooves, lie between the Internal and Innermost intercostal muscles.
Subcostales
This group of muscles runs in the same direction as the Internal intercostals, passing across multiple ribs. They arise from the internal surfaces of the rib, passing medioinferiorly across the rib immediately below before inserting into the internal surface of the rib directly below that, i.e. they span three ribs. These muscles are thought to work in combination with the Internal intercostals during forced expiration.
Scalenes
The scalene muscle group consists of three pairs of muscles – Scalenus anterior, Scalenus medius, and Scalenus posterior. They arise from the transverse processes of C2–C7, with the anterior and medial pair inserting into the superior surface of the first rib, Scalenus medius inserting posteriorly in relation to Scalenus anterior. Scalenus posterior inserts into the superior surface of the second rib, just anterior to the angle of the rib. The anterior and medial Scalenes lift the first rib (as well as contributing to neck flexion), whilst the posterior Scalene raises the second rib (whilst allowing the neck to laterally flex). In addition, they can act as accessory muscles for inspiration. The Scalenes are important clinically because the subclavian artery and the brachial plexus both pass between the anterior and medial Scalenes (the scalene fissure, scalene hiatus). The subclavian vein and the phrenic nerve pass across the anterior aspect of Scalenus anterior where it inserts into the first rib.
Transversus thoracis
These muscles are found on the innermost surface of the anterior thoracic wall, arising from the posterior aspect of the xiphoid process, the lower third of the body of the sternum, and the costal cartilages of ribs 4–7. They run superolaterally to insert into the inferior edges of the costal cartilages of ribs 3–6, lying in the same plan as the Internal intercostal muscles, although there is variation in this insertion between individuals, as well as on opposite sides of the sternum in the same individual. The internal thoracic vessels lie between the Transversus thoracis muscles and the Internal intercostal muscles.
Vascular supply
The thoracic wall is mainly supplied by the anterior and posterior intercostal arteries, running within the intercostal spaces in the costal grooves of the ribs. The intercostal arteries arise from the aorta and internal thoracic arteries. The internal thoracic arteries (internal mammary arteries) arise from the subclavian artery and run down the lateral borders of the body of the sternum together with the internal thoracic vein between the Internal intercostal and the Transversus thoracis muscle layers. The internal thoracic arteries give off two branches at each rib level, the superior branch running along the inferior surface of the upper rib whilst the lower branch anastomoses with a collateral branch from the posterior intercostal artery. The internal thoracic artery then bifurcates near the sixth intercostal space to form the musculophrenic and superior epigastric arteries.
There are 11 paired posterior intercostal arteries that supply the posterior aspect of the intercostal spaces. The first and second branches arise from the supreme intercostal artery, which itself runs down into the thorax as a branch of the costocervical trunk (a posterior branch of the subclavian artery). The third to ninth branches arise from the posterior aspect of the thoracic aorta, but it should be noted that due to the position of the aorta to the left of the vertebral column the posterior intercostal arteries for the right side of the posterior thoracic wall must pass across the vertebral bodies, posterior to the esophagus, thoracic duct, and the azygos vein. The posterior intercostal arteries then run along the inferior border of the corresponding rib, together with the posterior intercostal vein and the intercostal nerve relative to that intercostal space. Further branches arise from the posterior intercostal arteries which anastomose with branches of the anterior intercostal arteries.
The venous system mirrors the arterial supply, with the intercostal veins draining into internal thoracic veins, in turn draining into brachiocephalic veins.
Innervation
Intercostal nerves provide innervation for the thoracic wall, and these are formed from the anterior rami of spinal nerves T1–T11. Spinal nerves exit the dural sleeve at the intervertebral foramen and travel through the paravertebral space to enter the intercostal space becoming intercostal nerves. The intercostal nerves run together with the artery and vein along the lower border of the ribs. The first two intercostal nerves (from T1 and T2) innervate the upper limb in addition to the thoracic wall, the nerves from T3–T6 innervate the thoracic wall only, whilst those from T7–T11 innervate both the thoracic and abdominal walls. The xiphoid process indicates the termination of the seventh intercostal nerve, whilst the umbilicus indicates the termination of the tenth intercostal nerve. The nerve from T12 innervates the abdominal wall and groin.
Abdominal wall
The margins of the abdominal wall are the xiphoid process and costal margins superiorly, the vertebral column posteriorly, and the upper borders of the pelvis inferiorly. There are multiple layers to the abdominal wall consisting of fascia, muscles, peritoneum, and skin.
Superficial fascia
The superficial fascia consists mainly of fatty connective tissue continuous with the superficial fascia of the rest of the body, although anteriorly it forms two layers in the lower region below the umbilicus, referred to as the deeper membranous layer and the superficial fatty layer. The superficial fatty layer, as the name suggests, contains a high proportion of fat and may vary considerably in thickness. It runs over the inguinal ligament and is continuous with the superficial fascia of the thigh. In the male the superficial layer also continues over the penis, and fuses with the deeper layer of superficial fascia over the scrotum, forming the dartos fascia, a specialized layer, which contains smooth muscle, but has low levels of fatty tissue. In females the levels of fatty tissue remain, and this layer contributes to the labia majora.
The deeper membranous layer is much thinner with lower levels of fat. Inferior to the inguinal ligament it fuses with the fascia lata in the thigh, whilst in the midline of the abdomen it blends with the linea alba and the symphysis pubis. Inferiorly it runs into the perineum and attaches to the inferior pubic ramus (ischiopubic ramus) and the posterior aspect of the perineal membrane, sometimes referred to as Colles’ fascia. In the male the deep and superficial fascial layers blend to form the superficial fascia of the penis, subsequently contributing to the dartos fascia. Extensions of the deeper layer also attach to the pubic symphysis of the male to form the fundiform ligament of the penis. In females the deeper layer extends into the labia majora and the anterior aspect of the perineum.
Muscles
The five muscles of the abdominal wall are sited antero-laterally and are described as either flat or vertical:
Flat – External oblique, Internal oblique, Transversus abdominis
Vertical – Rectus abdominis, Pyramidalis.
The flat muscles arise posterolaterally and run forwards towards the midline, gradually being replaced by aponeurosis at the midline, whereas the vertical muscles run within the aponeurosis arising from the flat muscles, and are situated para-laterally to the midline. Together these muscles work synergistically as a support mechanism for the abdominal organs to maintain them within the abdominal cavity, and also to maintain posture.
Transversus abdominis ––
this is the deepest of the three flat muscles, lying under the internal oblique muscle. It blends with the linea alba at the midline.
Internal oblique ––
this is the intermediate muscle of the flat muscle group. It is a relatively small and thin structure when compared to the External oblique muscle. This muscle also blends at the midline with the linea alba, and its fibers run superomedially.
External oblique ––
this is the most superficial of this muscle group, and lies immediately below the superficial fascia. Its fibers run inferomedially, and as it blends with the other muscles in the group it contributes a large aponeurotic component to the anterior aspect of the wall. From the inferior border of the aponeurosis of the External oblique muscle the inguinal ligament arises, running from the anterior superior iliac spine anteroinferiorly to attach to the pubic tubercle. The inguinal ligament also forms part of the inguinal canal. At the anterior end of the inguinal ligament there are a number of other ligaments formed: the lacunar ligament arises as a crescent-shaped structure, which runs backwards to insert into the pecten pubis on the iliopubic ramus, and further elements arise from the lacunar ligament at this point to form the pectineal ligament (Cooper’s ligament).
All three flat muscles are each surrounded by a layer of deep fascia, the layer specifically related to the Transversus abdominis muscle being known as the transversalis fascia. This layer is continuous with the lining of the abdominal and pelvic cavities, as well as the fascial layer on the inferior aspect of the diaphragm, and the deep fascia of the muscles on the posterior abdominal wall and the thoracolumbar fascia.
Rectus abdominis ––
this is a flat, paired muscle separated by the linea alba in the midline. It runs from the costal margin to the pubic symphysis, being wider and thinner superiorly. In those with well-developed Rectus muscles it is possible to see transverse fibrous banding at intervals along the length of the muscle.
Pyramidalis ––
as the name would suggest, Pyramidalis is triangular in shape, and may not be present in all individuals. The base of the triangle arises from the pubis with the apex inserting into the linea alba, the muscle belly lying anterior to Rectus abdominis.
Both vertical muscles are also enclosed in a structure known as the rectus sheath consisting of the aponeuroses of the Internal and External obliques, and the Transversus abdominis muscles. The lower quarter posterior surface of the Rectus abdominis muscle is not covered by the rectus sheath, and, therefore, is in immediate contact with the transversalis fascia at this point.
Extraperitoneal fascia
Deep to the transversalis fascia is the extraperitoneal fascia, separating it from the peritoneum. The extraperitoneal fascia lines the abdominal cavity and is continuous with the lining of the peritoneal cavity. The fascia is thicker and fattier on the posterior aspect of the abdominal wall (forming the pararenal fascia around the kidneys), but becoming thinner and more fibrous towards the linea alba. Beneath the extraperitoneal fascia lies the peritoneum, which is a thin, serous membrane providing the innermost layer of the abdominal wall (parietal peritoneum). In some areas this reflects onto the abdominal organs to provide either a partial or complete covering (visceral peritoneum). In females, the parietal peritoneum forms a sac with small openings allowing the uterine tubes to pass through. In males this sac is closed, but in both cases this sac forms the peritoneal cavity.
Vascular supply
The arterial supply (mirrored by venous drainage) of the abdominal wall can be considered in superficial and deep layers.
Superficial layer ––
superiorly, it is supplied by branches of the musculophrenic artery (arising from the internal thoracic artery), whilst the inferior aspect of the wall is supplied laterally by the superficial circumflex iliac artery, and medially by the superficial epigastric artery, both of which arise from the femoral artery.
Deep layer ––
the superior aspect of the deep supply is from the superior epigastric artery (a terminal branch of the internal thoracic artery), whilst the deep lateral aspect arises from the tenth and eleventh intercostal arteries together with the subcostal artery. Inferiorly the supply is from the inferior epigastric artery and deep circumflex iliac artery, both of which arise from the external iliac artery. Both the inferior and superior epigastric arteries run posterior to Rectus abdominis, eventually anastomosing with each other.
Innervation
The spinal nerves of T7–T12 and L1 provide innervation to the anterolateral parietal peritoneum, muscles, and skin, passing from posterior to anterior and giving off smaller lateral cutaneous branches (Figure 6.3). The intercostal nerves of T7–T11 run deep to the costal cartilage and run forward to the anterolateral wall between Transversus abdominis and the Internal oblique muscle. They pass posteriorly to the lateral border of the rectus sheath and give off an anterior cutaneous branch, which passes through Rectus abdominis to the skin. Eventually all these nerves provide cutaneous supply, with T7–T9 innervating the skin from the xiphoid process to the umbilicus; T10 supplying the skin of the umbilicus; T11, T12, and L1 innervating the area inferior to the umbilicus to the pubic region. L1 also provides a branch known as the ilio-inguinal nerve, which innervates the anterior surface of the labia majora/scrotum, with a small cutaneous branch running to the thigh.
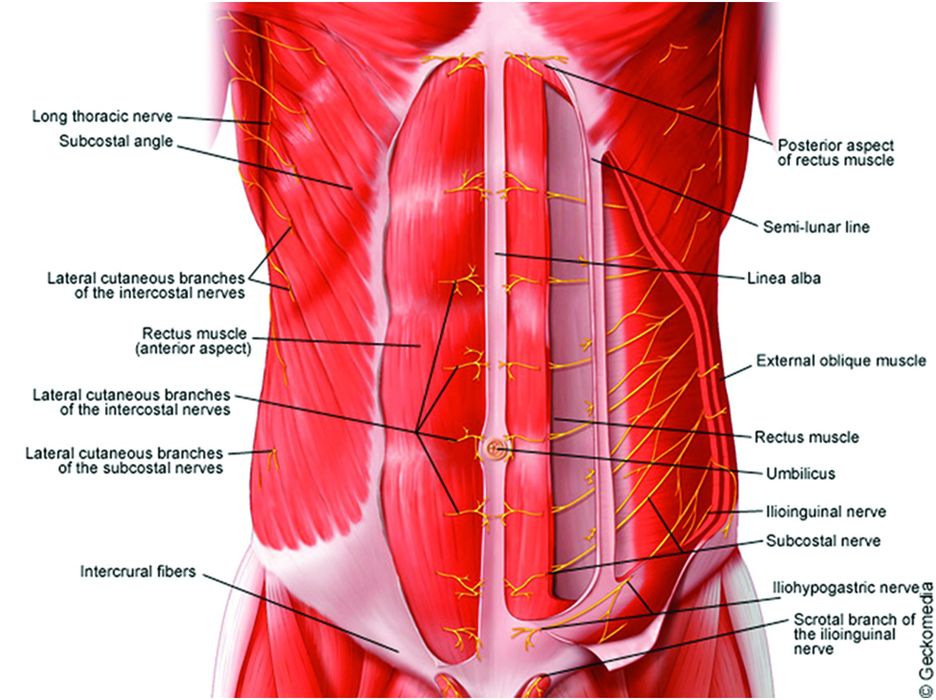
Anterior abdominal wall.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








