Sonoanatomy for the ilioinguinal/iliohypogastric block (ILIHB).
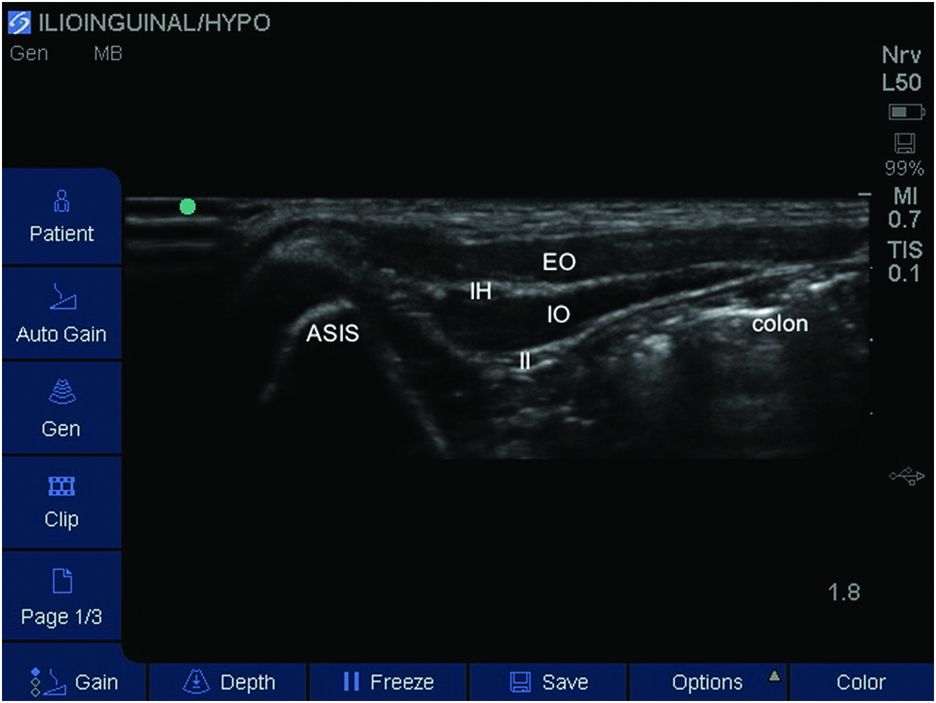
Labeled sonoanatomy for the ilioinguinal/iliohypogastric block (ILIHB). ASIS, anterior superior iliac spine; EO, external oblique; IH, iliohypogastric nerve; II, ilioinguinal nerve; IO, internal oblique.
Landmarks
The child should be placed supine with the lower abdomen, iliac crest, and groin exposed. In order to identify the nerves, the probe is placed on the iliac crest along a line joining the anterior superior iliac spine (ASIS) with the umbilicus (Figure 14.3).

Patient position and probe placement. A lateral needle approach is performed.
Identify all three muscle layers and the ilioinguinal/iliohypogastric nerves between the internal oblique and the transversus abdominis. Color Doppler will confirm the presence of any vascular structures in the same plane as the nerves.
Block performance
The block can be performed using an in-plane or out-of-plane approach using a 5–8 cm 22-gauge insulated needle. The in-plane approach confers the advantage of continuous assessment of needle position, which is important given the close proximity of the desired plane and the bowel (Weintraud at al., 2008). High-frequency linear ultrasound probes (5–10 MHz) can provide excellent definition as the nerves remain very superficial in the pediatric population, at a depth of approximately 1–3 cm. Bupivacaine 0.25% or levobupivacaine 0.25% are the most commonly used LA agents with a dose range of 0.1–0.2 ml/kg with a maximum volume of 10 ml. Doses as low as 0.075 ml/kg have previously been described with high success rates (Willschke at al., 2006).
Using an in-plane approach, the needle can be inserted either medially or laterally to the probe (Figure 14.4). The needle insertion point should be placed a short distance from the probe to allow visualization of the needle throughout the procedure.
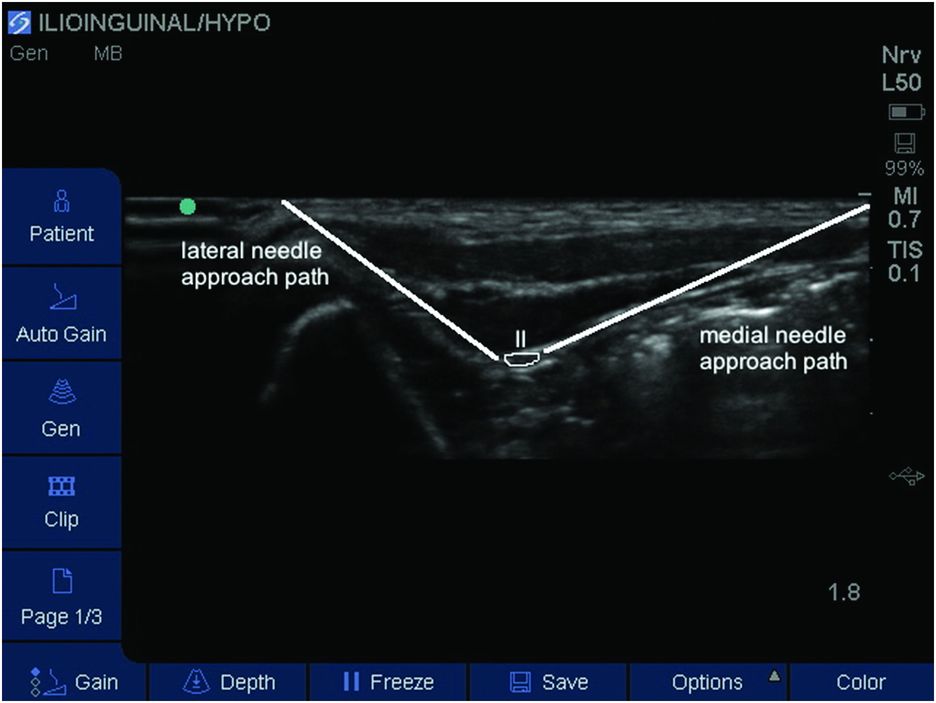
Needle pathway(s) and site of local anesthetic (LA) injection (outline) for block of ilioinguinal nerve (II).
Depending on the neural anatomy, two separate needle pathways may be required to deposit LA between the two oblique muscles or the internal oblique and transversus abdominis muscles only. Once the needle can be viewed in close proximity to the nerve (s) between the two muscle layers, careful aspiration is performed and a small volume of LA deposited. Once separation of the correct fascial layer is observed, the remaining LA can be injected. There are three principles of the correct injection technique. The first is to locate the correct depth. This is achieved through needle visualization on ultrasound in conjunction with a “pop” or “fascial click” as the fascial layer is penetrated. The second principle states that minimal resistance should be encountered when injecting around the nerve, and the third principle is to never inject against resistance. The presence of resistance increases the likelihood that the needle tip is in muscle (Broen, 2012).
Alternatively an out-of-plane approach can be used. The needle is inserted at 90 degrees to the skin in the middle of the ultrasound screen. Progress of the needle causes tissue displacement, which allows assessment of needle tip position.
As no definitive method exists to identify LA toxicity, it is imperative that small doses are injected incrementally during the block. In addition, an observation period of up to 90 seconds after each dose has been suggested in order to detect any changes (Mosseti and Ivani, 2012).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








