Robert S. Holzman
In dealing with those who are undergoing great suffering, if you feel “burnout” setting in, if you feel demoralized and exhausted, it is best, for the sake of everyone, to withdraw and restore yourself. The point is to have a long-term perspective.
—Dalai Lama
I. Wellness and the Anesthesiologist
Wellness is personal; therefore, a single definition is elusive. Of diverse cultural and spiritual backgrounds, anesthesiologists operate in a high-stress environment physically, mentally, and emotionally. They work alongside one another while experiencing vastly different life stages, thereby “wellness” means something entirely different to each member of the team. Compare the 29-year-old residency graduate in her second year of marriage, starting a family, and paying down medical school debt while learning how to become an autonomous physician and teacher, with the 63-year-old seasoned practitioner celebrating her first grandchild while contemplating retirement, her own health, and the illness or death of a parent. Here the commonality of wellness is defined as the collective thought processes, behaviors, values, and attitudes that lead to increased resilience, decreased burnout, an enhanced sense of well-being, and improved job and life satisfaction. Given that wellness is a multivariate, complex, and personal endeavor, it is not the purpose of this chapter to provide a personal guide to wellness. Rather, this chapter will provide a summary of wellness issues specific to the anesthesiologist, the practice of anesthesiology, and to leaders within anesthesiology-related organizations.
 VIDEO 44-1
VIDEO 44-1
Wellness Principles

Wellness is a complex and personal endeavor, defined by the collective thought processes, values, and attitudes that lead to increased resilience, decreased burnout, and an enhanced sense of well-being, including job and life satisfaction.
Several organizations have incorporated wellness as a group of competencies to be achieved during training. For example, the Royal College of Physicians and Surgeons of Canada lists: “Demonstrate a commitment to physician health and sustainable practice” as the third competency of professionalism in their 2005 framework (1). More recently, as part of the Milestones project, well-being has been addressed as a training requirement: “Professionalism: Responsibility to maintain personal emotional, physical, and mental health.”
Although the concept of wellness remains somewhat nebulous, the concept of burnout is well established. The “burnout syndrome” gained attention in the 1970s and 1980s, when Maslach et al. (2) developed and marketed the “Maslach Burnout Inventory” (MBI). They defined burnout as “a syndrome of emotional exhaustion and cynicism that occurs frequently among individuals who do ‘people work’ of some kind.” The MBI characterizes burnout based on three major psychological characteristics: emotional exhaustion, depersonalization, and a low sense of personal accomplishment. The MBI has since become the gold standard in quantifying burnout.
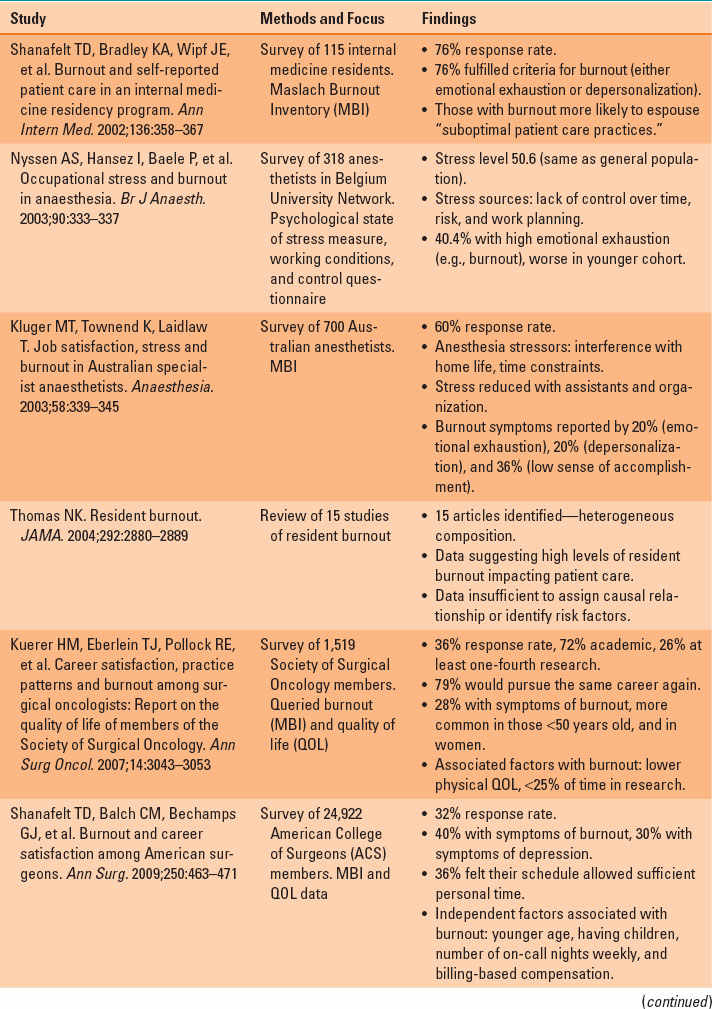
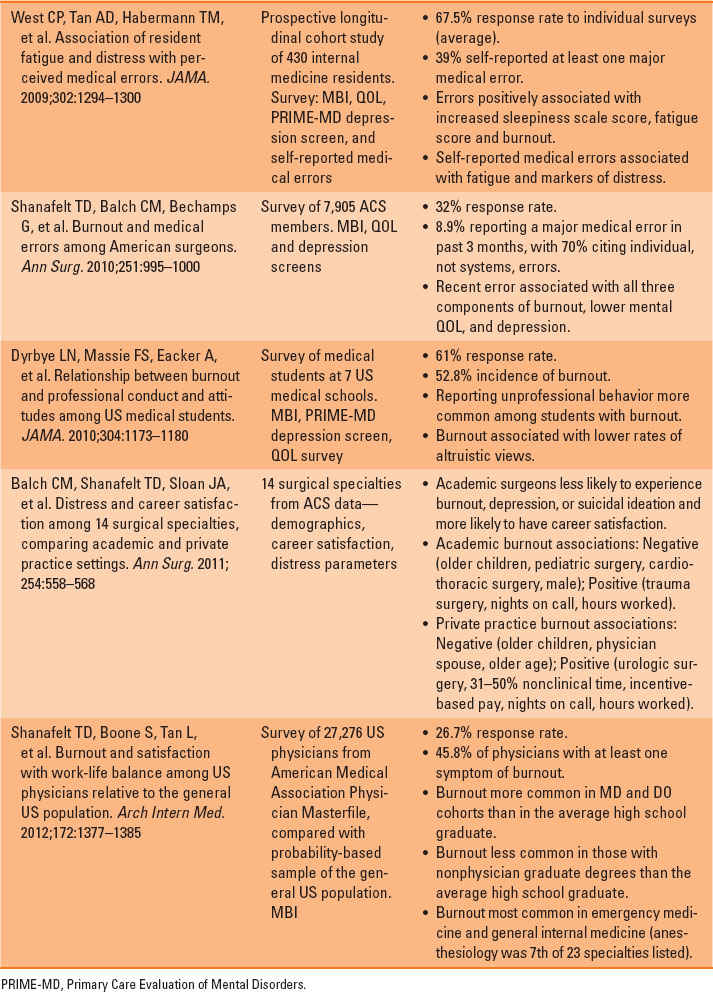
In 1999, in response to a growing body of literature concerning higher rates of suicide, substance abuse, and depression among anesthesiologists, Jackson (3) contemplated the role of stress, closely examining aspects such as personality type, physical implications of stress, life-cycle changes, sex stress differences, self-esteem, and workplace stress abatement. He defined stress as the “nonspecific adaptive response of the body to any change, demand, pressure, challenge, threat or trauma” and related this to the particular stressors encountered within the practice of anesthesiology. Jackson offered that a humanistic approach to medical education, coupled with the teaching of stress management techniques, could improve the overall professional and personal lives of anesthesiologists. Following this, a body of literature has amassed exploring the epidemiology and impact of burnout in the larger community of physicians (Table 44-1).

In one large national study, physicians reported higher burnout rates than the average high school graduate, whereas those with nonmedical graduate degrees reported lower burnout rates than the average high school graduate.
Shanafelt et al. (4) surveyed over 27,000 US physicians, with 46% of them reporting at least one burnout symptom (emotional exhaustion, depersonalization, or low sense of personal accomplishment). Physicians and osteopaths reported higher rates of burnout than the average high school graduate. However, a comparison group holding nonmedical graduate degrees had lower rates of burnout than the average high school graduate. Anesthesiologists ranked 7 of 23 medical specialties in burnout among physicians. Of all respondents, 38% screened positive for depression and 6% reported suicidal ideations within the past 12 months.
II. Special Circumstances
Some stressors are so vital they require intervention to continue practice. This has resulted in various legislative efforts, as described in the sections that follow.
A. Americans with Disabilities Act
The Americans with Disabilities Act (ADA) is “An Act to establish a clear and comprehensive prohibition of discrimination on the basis of disability” that was signed into law by George H. W. Bush in 1990. This was followed in 2008 by the ADA Amendments Act (ADAAA), which broadened the protections offered in the original bill. In order to be protected by the ADA, a person must demonstrate a disability to qualify for protection and then request reasonable accommodation. A major focus of the ADAAA was to clarify the meaning of disability and broaden its definition to include any impairment that “substantially limits” a “major life activity.” Although patients’ safety must take primary focus, there will occasionally be physicians who have physical or mental limitations, including visual and auditory impairments. Often, reasonable accommodations can be made to enable the anesthesiologist to perform in an acceptable manner. When this is possible, the patient is protected by the ADA. Controversy is introduced, however, when there is a question of whether the proposed accommodations are reasonable or when patient safety appears to be compromised. Further questions—and controversies—arise at the local level with regard to credentialing and privileges and at the indemnification level with liability insurance underwriting. These cases are rare and are generally dealt with on a case-by-case basis.
Table 44-1 Physician Burnout: Causes, Consequences, and Epidemiology
B. Family and Medical Leave Act
The Family and Medical Leave Act of 1993 was signed into law by President Bill Clinton and was a federal attempt at protecting work–life balance by ensuring covered employees job-protected, albeit unpaid, leave during times of family need, such as an illness in the family, military leave, personal illness or recovery, pregnancy, or adoption. Certain stipulations (e.g., who is considered a covered employee, including employment of 12 months prior to leave) are made, but most employed physicians and trainees fall within this category. Many employers also provide paid leave for various periods of time and circumstances. Controversies persist regarding the relatively higher use by women for maternity leave, although the use of paternity leave does appear to be increasing.
III.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








