Valvular Heart Disease
Jay A. Mazel MD
The cardiac valves are designed to maximize the work performed by the heart. If the valves malfunction, a hemodynamic strain is placed on the heart. This strain is initially tolerated because the heart compensates by increasing in size or dimension. Over time, however, the hemodynamic burden leads to cardiac muscle dysfunction and congestive heart failure, and sometimes sudden death.
In the management of every case of valvular heart disease, the primary care provider must answer two major questions: Is the valvular disease severe enough to warrant mechanical intervention over medical therapy? If so, what is the best time to refer the patient for surgical intervention? This chapter will review these questions for the four major acquired left-sided valvular lesions: aortic stenosis, mitral stenosis, nonischemic mitral regurgitation, and aortic regurgitation.
ANATOMY, PHYSIOLOGY, AND PATHOLOGY
The compensatory mechanisms of the cardiovascular system depend on the type of hemodynamic strain imposed on the heart by the dysfunctional valve. If the valve is stenotic, the reduced valve area obstructs blood flow. To maintain an adequate cardiac output, more pressure must be generated to propel blood across the valve. Therefore, in stenosis, the heart undergoes hypertrophy to reduce the increasing wall tension. In contrast, if the valve is incompetent, forward stroke volume is reduced in proportion to the degree of regurgitation. To maintain the cardiac output, more volume must be generated to maintain forward flow. The heart dilates to accommodate the increasing volume. The hypertrophied or dilated heart decompensates when the pressure or volume creates excessive wall tension and overwhelms the ability of the heart to contract, resulting in a reduced cardiac output.
In valvular stenosis, the increased pressure and wall tension generated are dispersed proximal to the obstruction. In aortic stenosis, patients remain symptom-free for years because of the marked ability of the left ventricle to hypertrophy. Twice the baseline mass (105 to 275 g/m2) is typical; however, even 10 times baseline mass has been reported (Passik et al, 1987). In contrast, in mitral stenosis the left atrium is in direct communication with the pulmonary vasculature and cannot adapt as easily. Thus, in mitral stenosis, increased atrial tension and pulmonary wall tension occur in the disease, manifested as dyspnea, orthopnea, and atrial arrhythmias.
Left ventricular dilatation occurs in both chronic aortic regurgitation and chronic mitral regurgitation. In aortic regurgitation, the increased volume is entirely ejected into the aorta. In contrast, in mitral regurgitation the regurgitant volume enters the left atrium. This is an important distinction because the increased stroke volume of aortic regurgitation increases pulse pressure, causing systolic hypertension. This imposes a significant increase in afterload on the left ventricle, as high as levels seen in aortic stenosis.
EPIDEMIOLOGY
Aortic Stenosis
Acquired aortic stenosis is usually an idiopathic disease resulting from degeneration and calcification of the aortic leaflets. When the disease is acquired in previously normal tricuspid aortic valves, stenosis develops in the sixth, seventh, and eighth decades. In persons born with a bicuspid aortic valve, stenosis is more likely to occur than in those with normal tricuspid valves. In these patients, stenosis typically develops earlier, in the fourth and fifth decades of life. It is unknown why aortic stenosis occurs in some people and not in others. Aortic stenosis does, however, share some of the same risk factors associated with coronary atherosclerosis, such as hypertension, hypercholesterolemia, calcification related to renal disease, and even infection with Chlamydia pneumoniae (Otto et al, 1994; Juvonen et al, 1997).
Mitral Stenosis
Mitral stenosis is usually a consequence of rheumatic heart disease, which primarily affects women. Although mitral valve involvement occurs in 40% of acute rheumatic fever cases, patients rarely recall having had rheumatic carditis. A history of rheumatic fever, therefore, is not helpful in establishing the presence or absence of mitral stenosis. In rheumatic heart disease, isolated mitral stenosis is the most common, followed by combined mitral stenosis and aortic stenosis. Isolated mitral regurgitation rarely occurs. The steady decline in the incidence of rheumatic fever has reduced the incidence of mitral stenosis in developed countries. In developing nations, however, both rheumatic fever and mitral stenosis remain common.
Regardless of the etiology, if aortic or mitral stenosis was not present at birth, the disease develops later in life from damage to the valve cusps. This causes abnormal flow patterns and predisposes the valve to fibrosis and calcification later in life. Because turbulent blood flow tends to persist, the stenosis can usually be expected to progress.
Mitral Regurgitation
Aortic Regurgitation
Aortic regurgitation results from disease of either the aortic leaflets or the aortic root that prevents coaptation of the leaflets. Leaflet abnormalities that result in aortic regurgitation can be secondary to infective endocarditis and rheumatic fever. Aortic root causes of aortic regurgitation include Marfan syndrome, aortic dissection, collagen vascular disease, syphilis, and annuloaortic ectasia.
HISTORY AND PHYSICAL EXAMINATION
Aortic Stenosis
The classic symptoms of aortic stenosis are angina, syncope, and the symptoms of congestive heart failure. Angina develops in aortic stenosis because of reduced coronary flow reserve and increased myocardial oxygen demand caused by high afterload. Exertional syncope results from either a vasodepressor response or an exercise-induced drop in total peripheral resistance that is uncompensated because the cardiac output is restricted by the stenotic valve. Heart failure in aortic stenosis results from diastolic dysfunction, systolic dysfunction, or both. Diastolic dysfunction results from increased left ventricular wall thickness and increased collagen content. Systolic dysfunction results from excess afterload, decreased contractility, or a combination of these factors.
A systolic ejection murmur radiating to the neck is the most common sign of aortic stenosis. It is usually heard best in the aortic area. It disappears over the sternum and then reappears in the apical area, mimicking mitral regurgitation (Gallivardin’s phenomenon). In mild aortic stenosis, the murmur usually peaks early in systole. As the severity of stenosis increases, the murmur peaks progressively later in systole and may become softer as the cardiac output diminishes. The carotid upstrokes classically become diminished in amplitude and delayed in time (parvus et tardus). S2 may become paradoxically split because of the delay in left ventricular emptying, or the second heart sound may become single because the aortic closing component is lost.
Mitral Stenosis
Patients with mitral stenosis usually have symptoms typical of left-sided heart failure: dyspnea on exertion, orthopnea, and paroxysmal nocturnal dyspnea. The increases in pulmonary vascular pressure can cause hemoptysis, hoarseness, and symptoms of right-sided heart failure. These symptoms are somewhat more specific for mitral stenosis but occur less frequently. Typically, patients first present with dyspnea or orthopnea when a cardiac stress such as pregnancy or atrial fibrillation occurs. The symptoms of mitral stenosis stem from increased left atrial pressure and reduced cardiac output, primarily caused by mechanical obstruction during filling of the left ventricle. Although the symptoms are those of left ventricular failure, the left ventricular function is usually normal in mitral stenosis. In some cases, however, the left ventricular ejection fraction is reduced because of excessive afterload secondary to a reflexive increase in systemic vascular resistance. Because it is the right ventricle that ultimately propels blood through the mitral valve, right ventricular function is compromised, first by the afterload imposed on it by high left atrial pressure and then by the development of secondary pulmonary vasoconstriction.
During physical examination, mitral stenosis is suspected because of the presence of the classic diastolic rumble that follows an opening snap. S1 is characteristically loud because the mitral valve is held open by the transmitral gradient until the force of ventricular systole closes the valve. A loud P2, right ventricular lift, elevated neck veins, ascites, and edema indicate that pulmonary hypertension with right ventricular overload has developed. This is an ominous sign in the progression of the disease because pulmonary hypertension increases the risk associated with surgery.
Mitral Regurgitation
Chronic mitral regurgitation is compensated by the development of eccentric cardiac hypertrophy. Cardiac enlargement should therefore be manifest on physical examination. A holosystolic apical murmur heard on physical examination alerts the examiner that mitral regurgitation is present. An S4 suggests that the disease is severe. An S3 heard in mitral regurgitation, however, does not necessarily indicate the presence of congestive heart failure, because in this situation rapid filling of the left ventricle causes the sound by the large volume of blood stored in the left atrium in diastole.
Aortic Regurgitation
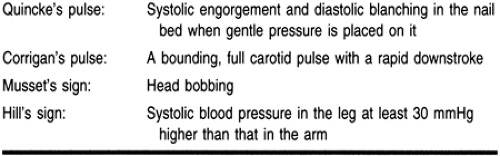
The large total stroke volume in aortic regurgitation increases pulse pressure, which produces a host of clinical signs. Although the typical diastolic blowing murmur heard along the left sternal border is the usual sign of aortic regurgitation, the peripheral signs of a hyperdynamic circulation indicate when the disease is severe. Table 14-1 is a partial list of these signs.
In addition to the typical murmur of aortic insufficiency, a diastolic rumble (Austin Flint murmur) may also be heard over the cardiac apex. Although its origin is debatable, the Austin Flint murmur is probably produced as the aortic jet impinges on the mitral valve, causing it to vibrate. Simultaneous diastolic filling of the left ventricle from the left atrium and aorta tends to close the mitral valve in diastole, producing physiologic stenosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree