Low Back Pain
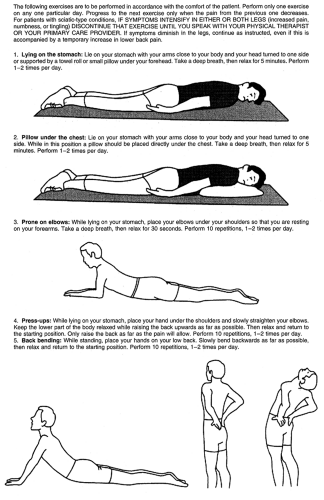
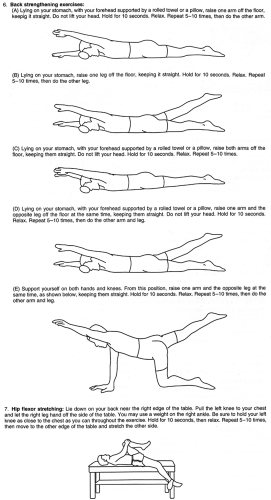
Steve Weintraub DO
Low back pain (LBP) remains one of the leading reasons for primary care visits. It usually resolves with nonspecific treatment within 6 weeks in 75% to 90% of cases, but there is a high likelihood of recurrence. LBP continues to be a costly condition in terms of both actual health care dollars spent and time lost from work.
Pain is subjective, and there may be few if any objective findings. In fact, a precise pathognomonic diagnosis can be given in only 10% to 20% of patients with LBP (Margo, 1994; Brady, 1996). Because back pain may spontaneously resolve on its own, the back pain sufferers who seek health care attention are those for whom the pain is severe or disabling or lasts beyond a reasonable time, or for those seeking secondary gain. In most cases, LBP is labeled as lumbar strain because the physical exam reveals no gross abnormalities and recovery is often quick.
This chapter discusses the etiologies of LBP and the evaluation and treatment of patients. Primary care providers must have a good understanding of the anatomic, biomechanical, and physiologic factors of back pain, for this will aid in the evaluation and treatment of patients with LBP.
ANATOMY, PHYSIOLOGY, AND PATHOLOGY
Anatomy of the Spine
The spine is divided into four sections: there are 7 cervical, 12 thoracic, and 5 lumbar vertebral sections and the fused sacrum (Hainline, 1995) (Fig. 46-1). The bony vertebral bodies and intervertebral discs provide weight bearing and shock absorption. The posterior elements—vertebral arches, transverse and spinous processes, and facet joints—protect the spinal cord and nerve roots. The facets, ligaments, and paraspinal muscles provide stability and balance (Wipf & Deyo, 1995; Brady, 1996). Pain may arise from any of these structures. The combined anterior and posterior elements are referred to as a functional unit.
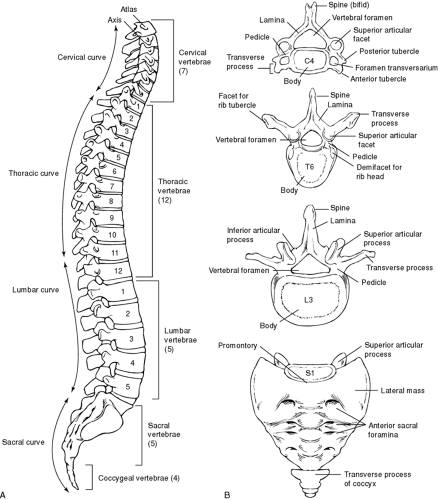 FIGURE 46-1 (A) Lateral view of vertebral column. (B) General features of different kinds of vertebrae. ( Snell, R. (1992). Clinical anatomy for medical students, 4/e. Boston: Little, Brown. ) |
The lumbar vertebra is a static structure that is made up of the anterior vertebral body and posterior elements (spinous process, articular facets, and transverse process). There is a strong potential for pain at the vertebral body and facet articular cartilage secondary to increased pain sensitivity. The most common etiologies are degenerative joint disease and fracture of any part of the vertebra (body, compression fraction secondary to osteoporosis, pars interarticularis stress fractures).
The intervertebral disc plays a major role in LBP. It is composed of the outer annulus fibrosis, made up of multiple layers of collagen fibers, and the inner nucleus pulposus, made up of a colloidal gel of proteoglycans and collagen. It is 80% fluid (Hainline, 1995; Cyriax, 1991; Al-Magdassy, 1996). Its functions are absorbing shock, providing resistance to compression, and allowing flexibility of the vertebral column (Hainline, 1995). A compromised disc lends itself to abnormal motion and disc herniation, with potential radiculopathy and pain. The neurologic components of spinal anatomy are discussed below.
Degenerative disc disease is usually secondary to an annular tear, with subsequent leakage of nuclear material and dehydration of the disc (Hainline, 1995). Large annular tears may lead to prolapse or herniation of the nuclear material and subsequent nerve root compression. With aging, the percentage of water decreases and the disc becomes less able to function normally, decreasing the risk of disc herniation in the older population.
The superior and inferior posterior lumbar facets are synovial articulations situated between each vertebral body (Margo, 1994; Wipf & Deyo, 1995; Hainline, 1995; Cyriax, 1991). They play a potential role, along with the intervertebral discs, which play a major role, in lower back dysfunction and pain.
Ligaments play a major role in stability and restriction of motion in the lumbar spine. The key ligamentous structures include the anterior and posterior longitudinal ligaments, which help reinforce the annulus. As the ligament descends toward the sacrum, it narrows, increasing the risk of a herniated nucleus pulposus. The ligamentum flavum and the interspinous and supraspinous ligaments all provide further support to spinal movement (Hainline, 1995; Al-Magdassy, 1996).
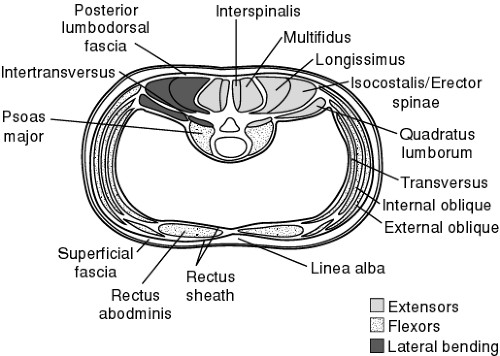
Muscles can be divided into anterior and posterior muscle groups. Most posterior is the erector spinae, which is made up of the lateral iliocostals, the intermediate longissimus, and the medial spinalis. The middle layer is the thick multifidus, and the deep posterior muscles include the rotators, interspinalis, and intertransversarii (Fig. 46-2). The anterior muscle group includes the abdominal muscles, which play a major role in lumbar stabilization. They include the psoas (which is a primary hip flexor), the outer external obliques, the intermediate internal obliques, and the inner transversus abdominis. The remaining anterior muscles include the midline rectus abdominis and the lateral quadratus lumborum, which functions as a lateral trunk flexor (see Fig. 46-2). All these muscles play a role in trunk motion and stabilization.
The anatomy of LBP is a combination of fact and theory. Studies have shown that pain can be reproduced by injecting hypertonic saline into the ligamentum flavum in facet joint capsules. Supra- and infraspinous ligaments are innervated by afferent branches of the posterior primary rami, and muscle spasms are thought to be a motor reflex to pain. The role of muscle injury as it relates to back pain has not been fully elucidated. Strains and sprains, however, remain the leading diagnosis.
Sciatic pain requires both mechanical and inflammatory stimuli. The sciatic nerve arises from L4–S3 nerve roots (common peroneal and fibial nerves), passes over the lower edge of the sciatic notch, and lies just beneath the piriformis muscle and just above the obturator internus muscle (see Fig. 46-2). The nerve innervates the gluteus medius and minimus as well
as the tensor fasciae latae before passing beneath the piriformis muscle. After passing through the main branch of the sciatic nerve, it innervates the hamstring and the muscles of the lower leg, and provides sensory innervation of the leg and foot (Borenstein et al, 1995).
as the tensor fasciae latae before passing beneath the piriformis muscle. After passing through the main branch of the sciatic nerve, it innervates the hamstring and the muscles of the lower leg, and provides sensory innervation of the leg and foot (Borenstein et al, 1995).
EPIDEMIOLOGY
Approximately 75% to 85% of the U.S. population will experience LBP at some point in their lives (Wheeler, 1995; Margo, 1994; Wipf & Deyo, 1995; Hainline, 1995). The prevalence of back pain ranges from 60% to 90%, with an annual incidence of 5% (Beattie, 1996; Daltroy & Iverson, 1997). The prevalence of LBP in both men and women 25 to 74 years of age is 16%, with an increase in prevalence in persons ages 45 to 64. There is a greater incidence in whites (16.5%) than African Americans (13.2%) or other racial groups (11.3%). Men and women are equally affected (Daltroy & Iverson, 1997), but women complain of back pain more often after the age of 60.
The prevalence of back pain alone and back pain with sciatica (defined as pain radiating along the course of the sciatic nerve to below the knee in one or both legs) is summarized in Table 46-1. Back pain, especially back pain with features of sciatica,
usually does not last longer than 2 weeks. As a result of back pain, there are 7 million people missing work at any one time in the United States alone.
usually does not last longer than 2 weeks. As a result of back pain, there are 7 million people missing work at any one time in the United States alone.
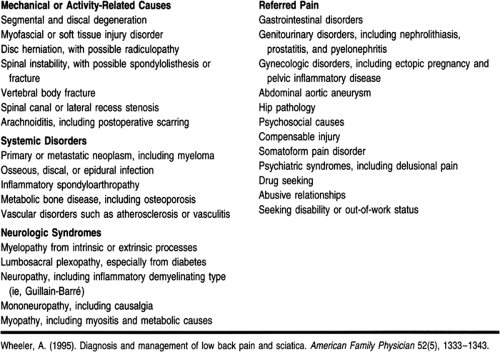
LBP has numerous etiologies. Fewer than 3% of cases are secondary to a serious medical disease. Most cases of LBP are mechanical in origin. Mechanical conditions of the spine, including disc disease, spondylosis, spinal stenosis, and fractures, account for up to 98% of cases of LBP, with the remaining cases the result of systemic and visceral disease (Wheeler, 1995; Margo, 1994). There are many opinions as to the actual neurogenic etiology of LBP, and only 10% to 20% of cases can actually be attributed to an anatomically defined lesion.
Epidemiologic studies also reveal distinct characteristics in the occupational and psychological profiles of people disabled by LBP. Many of these patients view their jobs as boring and dissatisfying (Daltroy & Iverson, 1997). They present with depression, anxiety, hypochondriasis, and hysteria. There also appear to be increased rates of alcoholism, divorce, headaches, and ulcers in this population (Turner & Denny, 1993). When working with patients with LBP, providers must keep in mind the possibility of secondary gain—either financial gain (through a lawsuit for a motor vehicle accident or other liability) or the desire to remain off work and collect disability. These issues must be carefully and sensitively discussed if the provider has evidence that this is the nature of the patient’s LBP disability.
There are equal numbers of reports of LBP in heavy laborers compared to those in sedentary occupations. The loss of productivity, however, and time lost from work are greater in heavy laborers. The risk factors in both settings may be biomechanical (twisting and other repetitive motions that occur on the job). In sedentary occupations, there is an increased risk secondary to muscular deconditioning or the chronic mechanical stress from sitting positions (Beattie, 1996). Other risk factors include obesity, cigarette smoking, lower socioeconomic status, and lower educational attainment.
Osteoporosis increases the risk of spinal compression fractures. Genetics may play a role in osteoporosis as well as congenital isthmic spondylolisthesis, spinal osteochondrosis (Scheurmann’s disease), and spinal stenosis associated with achondroplasia. Also, certain athletic activities, such as gymnastics and football, may increase the risk of spondylolysis and isthmic spondylolisthesis because they involve repetitive hyperextension.
DIAGNOSTIC CRITERIA
Differential Diagnosis
Although there are no true diagnostic criteria for LBP, Table 46-1 shows the multitude of LBP syndromes. This section focuses on the more common etiologies, or specific diagnoses of secondary back pain. The provider must be able to differentiate between benign causes, such as lumbar strain and disc disease, and the more ominous and life-threatening disorders that need quick referral, such as cauda equina syndrome, malignancy, and vertebral fracture with neurologic compromise. A thorough history and a detailed physical exam, including a neurologic exam, are warranted.
LBP can be divided into three clinical courses: acute, subacute, and chronic. It is useful to differentiate these three categories when approaching treatment protocols. The definitions are as follows:
Acute: 0 to 6 weeks
Subacute: 6 to 12 weeks
Chronic: More than 12 weeks.
It is also important to categorize back pain along with its etiology for correct treatment and accurate referral.
Mechanical or Activity-Related Causes
DEGENERATIVE DISC DISEASE
There appears to be a correlation between annular tears of the disc and degenerative disc disease. As previously stated, there is also a correlation with herniated nucleus pulposus. A slow leak over time of the nuclear material will lead to desiccation of the disc. How does this lead to back pain? One explanation is an inflammatory pathway involving chemical factors. This pathway may explain why pain is relieved when a corticosteroid or nonsteroidal anti-inflammatory agent is administered (Saal, 1995). The other theory is an immunologic phenomenon, described by in vitro studies. It is theorized that the nuclear material, previously sheltered from the immune system, generates an autoimmune response once it is exposed.
Degenerative disc disease may present with isolated LBP or with radicular symptoms. The diagnosis can be made with plain radiographs, noting diminished disc space between the vertebral bodies, or by magnetic resonance imaging (MRI), which notes changes on T2-weighted images.
LUMBAR SOFT-TISSUE INJURY/STRAIN, SPRAIN
Most cases of LBP fall into this category, known as nonspecific back pain. This pain usually resolves spontaneously in 2 to 6 weeks. If the pain persists longer than this, a secondary cause must be considered (ie, disc versus facet). In this type of pain, the most common etiologic factors are poor conditioning, excess weight, and sudden overuse or overload activities.
HERNIATED LUMBAR INTERVERTEBRAL DISC
Herniated disc is diagnosed in a small percentage of patients with LBP. Lumbar disc herniation is most common in persons ages 30 to 40; it is less common in adolescents and young adults and rare in the older population (Lazara & Quinet, 1994; Rothman & Simeone, 1992; Beattie, 1996). Acute herniation of the nucleus pulposus may result from sudden overload of the intervertebral disc or from repetitive microtraumatic loading (Hainline, 1995). For most patients with a herniated disc, back pain precedes the onset of sciatica. The back pain may or may not linger as the pain and paresthesias begin to radiate down the leg (Beattie, 1996).
The onset of sciatic pain may be gradual or sudden. Pain and radicular symptoms may be worsened by sitting for a long period, rising from a sitting or supine position, or coughing or sneezing.
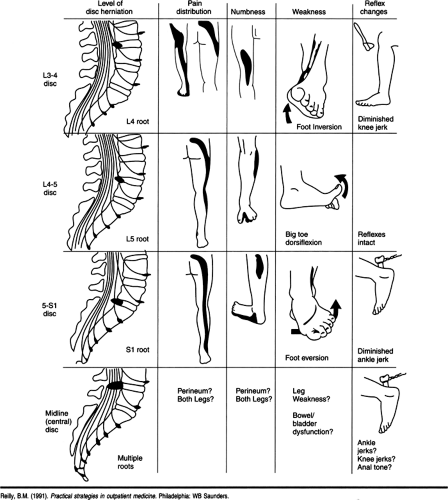
Herniated discs occur at the L4-5 or L5–S1 level in 95% of cases (Wipf & Deyo, 1995; Beattie, 1996). The neurologic examination should focus on the L5 and S1 nerve roots. A herniated disc at the L5 nerve root may cause pain and numbness radiating from the back to the anterior thigh, anterolateral leg, medial foot, and great toe. There are no reflex changes, and the motor exam reveals weakness in the great toe extensor as well as the dorsiflexors of the foot (Table 46-2).
Patients with an L5–S1 disc herniation (sacroiliac root) have pain and numbness of the posterior thigh and leg, posterior-lateral foot, and lateral toes; a diminished ankle reflex; and weakness of the plantar flexors of the foot, which can be seen with difficulty on toe walking (see Table 46-2). It is rare to see clinical herniations above the level of L4.
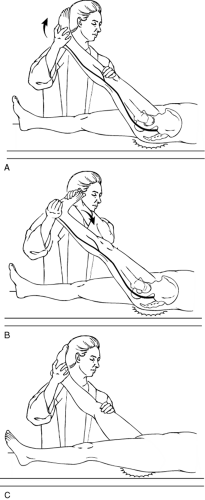
A positive straight leg raise (SLR) test helps confirm nerve root irritation. This test has a sensitivity of 95% with proven disc herniation, and its absence can actually rule out disc herniation. A crossover test or crossed SLR is less sensitive but more specific for disc herniation (Fig. 46-3). Electromyography may aid in the diagnosis of a particular radiculopathy, but it is better used to discriminate radicular pain from peripheral neuropathy.
Plain x-rays are not helpful in diagnosing a herniated disc, but they should be used to rule out tumor, infection, fracture, and spondylolisthesis. A herniated disc is usually confirmed when an imaging study such as myelography, computed tomography (CT), or MRI shows an abnormality corresponding to the clinical exam. However, these sophisticated and expensive studies should not be ordered too early in the course of a workup for LBP, especially if the patient is not considered a surgical candidate. These tests should be ordered in patients who have a long protracted course, or early in the case of cauda equina syndrome, a progressive neurologic deficit, or the suspicion of tumor or infection (Beattie, 1996).
SPINAL STENOSIS
Spinal stenosis (narrowing of the spinal canal) may be secondary to hypertrophy of the facet joints (osteoarthritis), hypertrophy of the ligamentum flavum, or spondylosis of the intervertebral disc, which is often superimposed on a congenitally narrow canal (Wipf & Deyo, 1995; Lazara & Quinet, 1994).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree