Lymphoma
Candis Morrison Ph.D., C.R.N.P.
Hodgkin’s and non-Hodgkin’s lymphoma are neoplasms of lymphocytes that affect the lymph nodes, the spleen, and the hematopoietic system. These cancers may spread to other tissues and structures, including the gastrointestinal tract, bone marrow, and liver. They are often referred to as immunologic cancers because of the immunologic function of the lymphocyte (Carson, 1996).
Although the clinical presentation and diagnostic evaluation of these two diseases are similar, the pathologic identification of marker cells distinguishes the two types of lymphoma. The diagnostic category determines both treatment and prognosis, despite the fact that the staging systems overlap.
The development of less toxic therapies and growth factors have lessened the complication of severe cytopenia, enabling many patients with lymphoma to be treated as outpatients. Primary providers participating in the care of these patients must understand the disease entities, the treatment modalities and their side effects, and complications. A multidisciplinary team approach is optimal to help decrease the morbidity and mortality rates associated with these hematologic malignancies.
ANATOMY, PHYSIOLOGY, AND PATHOLOGY
The intricate interrelation between the hematologic and the immunologic systems protects the body from foreign invaders, such as pathogens and toxins. There are three primary components of the immune system. The first is phagocytosis, in which invading substances are ingested and destroyed by individual immune cells. Mononuclear phagocytes recognize invaders, engulf foreign particles, and activate specific immunity. The second component is inflammation, in which cells and proteins defend the body against infection and repair tissue damage. The third component is cellular and humoral immunity. In cellular immunity, T lymphocytes initiate the response; in humoral immunity, the trigger is serum antibodies. Phagocytosis and inflammation are predominantly nonspecific immune responses, whereas humoral and cellular responses are characteristic of specific immunity (Post-White, 1996).
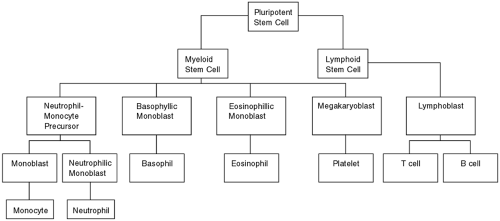
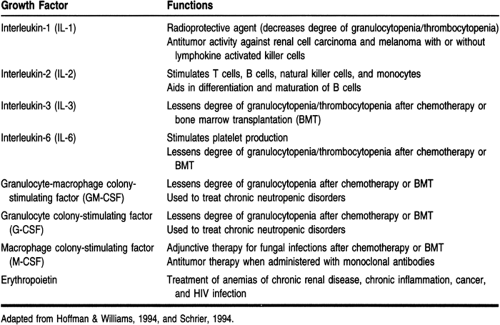
The primary cells of the immune system are lymphocytes and mononuclear phagocytes. Lymphocytes are formed from pluripotent stem cells, found primarily in the bone marrow. These cells differentiate into all of the recognized mature cell lines produced by the various hematopoietic cytokines, or growth factors (Lowry, 1996). Figure 38-1 illustrates normal hematopoiesis, and Table 38-1 describes the clinically relevant cytokines (Hoffman & Williams, 1994).
More than 1 billion lymphocytes are produced in the marrow daily. There are two functional classes of lymphocytes—the T lymphocytes, which regulate antibody synthesis and cellular immune processes, and the B lymphocytes, which contribute to the humoral response of antigen sensitization. The lymphoid stem cell is programmed by the bone marrow to develop into either a T-cell or a B-cell precursor. B-cell maturation occurs in the follicles of the lymph nodes after exposure to an antigen (Paradiso, 1995).
Lymphocytes are the only immunocompetent cells able to recognize antigens. T cells are produced in the marrow, mature in the thymus, and then are released to secondary lymphoid organs, such as the lymph nodes, the spleen, the tonsils, and Peyer’s patches in the ileum, as well as throughout all the connective and epithelial tissues of the body. Lymphocytes continuously circulate through the lymphatic network and vascular channels throughout the body and within nodes, which are densely clustered in the neck, axillae, abdomen, and pelvis (David, 1994).
Surface markers and receptors, which are macromolecules with a binding affinity for a specific antigen, appear on the immune cell during maturation. They signal each other to recognize, bind, and kill antigens. Surface markers differentiate between lymphocyte subsets and are recognized by monoclonal antibodies. These groups of lymphocytes, surface markers, and monoclonal antibodies are called “clusters of differentiation” (CD). The most commonly known surface markers are CD4 and CD8. CD4 defines the helper function of T cells, CD8 the suppressor or cytotoxic function (Post-White, 1996).
When B lymphocytes are activated by a signal from T lymphocytes, they differentiate into one of the five classes of immunoglobulins (Ig); IgM, IgG, IgD, IgE, and IgA. In the primary immune response, there is a latent period in which B cells make contact with the antigen, proliferate, differentiate, and secrete antibody. Because resting B cells express only IgM and IgD, and IgD is rarely secreted, IgM is the dominant antibody secreted in the primary immune response. Other isotypes, including IgG, IgA, and IgE, appear with second exposure to the same antigen. The secondary antibody response is more rapid than the primary because of the added ability of memory. This complicated host response is distorted by malfunctions in hematopoiesis, especially the proliferation of abnormal cells.
Hodgkin’s Disease
Hodgkin’s disease (HD) is a unifocal disease that usually spreads in a contiguous manner. Early in the course of the disease, only the lymph nodes are affected, making diagnosis difficult until multiple nodes are involved. The disease spreads predictably from the original site to lymph nodes in adjacent areas. This orderly pattern of contiguous spread is most evident in nodular sclerosing HD.
Some lesions that originate in the mediastinum spread to nodes in the lower neck and then to the upper retroperitoneal area. Other histologic types may skip the mediastinum and
spread to the retroperitoneal nodes without ever causing intrathoracic disease. Disease spreads to extranodal areas by direct extension and then invades the vasculature, resulting in hematologic dissemination. The spleen is the final lymph node area of involvement before hematologous dissemination occurs.
spread to the retroperitoneal nodes without ever causing intrathoracic disease. Disease spreads to extranodal areas by direct extension and then invades the vasculature, resulting in hematologic dissemination. The spleen is the final lymph node area of involvement before hematologous dissemination occurs.
CLINICAL PEARL
The absence of splenic disease is a positive prognostic indicator for HD.
Non-Hodgkin’s Lymphoma
Normally, the early lymphocyte matures in a predictable manner into a mature immunocompetent cell. However, in non-Hodgkin’s lymphoma (NHL), an abnormal proliferation of monoclonal cells occurs. Instead of progressing to the next developmental phase, the cells fix at one phase of development and continue to proliferate.
The neoplastic cell population is cloned from a single neoplastic hematopoietic stem cell and ultimately proliferates into
lymphoma. Surface markers and immunoglobulins are formed after the proliferation of neoplastic cells and designate the cell type of lymphoma. This progression of events has important implications for the prognosis and treatment of this disease.
lymphoma. Surface markers and immunoglobulins are formed after the proliferation of neoplastic cells and designate the cell type of lymphoma. This progression of events has important implications for the prognosis and treatment of this disease.
Seventy percent of lymphomas are B cell. B cells can be divided into four cytologic types: small cleaved, large cleaved, small noncleaved, and large noncleaved. It is possible to predict some of the clinical manifestations of NHL based on the characteristics of the predominant cell type. Neoplastic cells often retain the surface of their cells of origin, so it is also possible to group them according to the phenotypic properties of their surface markers.
The two major classes of NHL are indolent and aggressive. Indolent NHL is a generalized disease usually diagnosed late (stage III or IV in 70% to 90% of cases). Indolent NHL spreads noncontiguously, and bone marrow involvement is evident most of the time. Spread to the central nervous system is rare, and systemic symptoms are present in only 15% to 20% of cases. Aggressive NHL is often diagnosed early (stage I or II in 30% to 40% of cases). Mediastinal involvement is rare; the bone marrow is affected only 10% to 30% of the time. Ten percent to 15% of patients have central nervous system disease, and 20% to 30% have systemic symptoms (Sunderland & Coltman, 1993).
EPIDEMIOLOGY
With an incidence in excess of 61,000 cases a year, the malignant lymphomas collectively represent the sixth most common cause of cancer in the United States (ACS, 1998). Approximately 85% of patients with malignant lymphomas have NHL, and the remaining 15% have HD.
Hodgkin’s Disease
There are 7000 to 8000 cases of HD diagnosed in the United States each year. The incidence follows a bimodal curve. The first peak occurs between ages 20 and 25, followed by a plateau lasting until age 55. There is a second peak in the seventh decade (Klitz et al, 1994). HD is uncommon in children, with only 10% to 15% of cases occurring in patients younger than 16 (Weinstein & Tarbell, 1997). HD is more common in males than in females for all age groups, and half as common among African Americans as whites.
The etiology of HD is unknown. Evidence suggests that impaired growth factor genes, viruses, genetic alterations, and immune defects all contribute to tumorigenesis in HD (Durkop et al, 1992). Certain HLA phenotypes are associated with increased susceptibility, and there are several examples of multiple family occurrences. Siblings of patients with HD have a five- to ninefold increased risk of developing the disease, and that risk may be even higher in same-sex siblings (Sunderland & Coltman, 1993). It occurs more frequently in first-born children and in those from small families.
Patients with a higher standard of living or who are better educated are also at increased risk. One hypothesis suggests that exposure to common environmental pathogens is protective against HD, and this exposure is reduced in wealthier young people. In older patients, social class characteristics play a less significant role (Sunderland & Coltman, 1993).
An association between Epstein-Barr virus infection and HD has been postulated as a result of an increased incidence of HD in persons with a history of infectious mononucleosis. Prospective studies have also shown elevated Epstein-Barr virus titers in patients before the diagnosis of HD.
Non-Hodgkin’s Lymphoma
More than 53,600 cases of NHL are diagnosed each year. It is the sixth most common cause of cancer-related death in the United States, accounting for more than 23,800 deaths yearly (ACS, 1998). This is approximately three times the number of HD cases (Carson, 1996). Males outnumber females by 10:7. Because of the young average age of lymphoma patients (42 years) and the resulting number of years of life lost to these diseases, NHLs rank fourth in economic impact among cancers in the United States (Shipp et al, 1997).
There has been a 50% increase in the incidence of NHL in the past 15 years, one of the largest increases for any cancer group. Certain highly aggressive NHLs occur in the setting of AIDS, accounting for the biggest increase in overall incidence. Indolent lymphomas have also significantly increased in recent years (Shipp et al, 1997).
In the United States, the incidence of NHL shows a steady age-dependent increase from childhood through the eighth decade of life. Certain subcategories are more likely to occur in specific age groups. Diffuse large B-cell, lymphoblastic, and Burkitt’s lymphoma are the most common lymphomas in children. Aggressive lymphomas are the most common lymphoid neoplasms in young adults. Indolent lymphomas affect adults averaging age 56 years. Because the incidence of both indolent and aggressive lymphomas increases with age, they are the most common lymphoid malignancies in patients over 60 years of age (Shipp et al, 1997).
NHLs are more common in males than females and in whites than African Americans. Although NHLs are reported worldwide, specific subtypes occur more frequently in particular locales. Follicular lymphomas are rare in Latin America. Burkitt’s lymphoma occurs more frequently in tropical Africa, and adult T-cell lymphoma is more common in southwest Japan and the Caribbean (Shipp et al, 1997).
Some lymphomas have been associated with chromosome translocations and rearrangement of proto-oncogenes such as bcl-2 and c-myc. These changes may be important to the etiology and progression of the disease. Genetic abnormalities of chromosome 14 are recognized in many follicular lymphomas as well as in Burkitt’s lymphoma (Carson, 1996).
Some research suggests that exposure to certain herbicides, industrial solvents, or vinyl chloride may increase a person’s risk. Other possible risk factors include exposure to excessive amounts of radiation or treatment with high-dose chemotherapy for cancer, or with immunosuppressive agents such as those used after solid organ transplant (ACS, 1998). NHL is 45 to 100 times more likely among renal transplant patients receiving immunosuppressive therapy, with lymphomas accounting for 29% of cancers in these patients. Other patients predisposed to NHL are those with autoimmune diseases such as rheumatoid arthritis and systemic lupus erythematosus.
Certain viral etiologies have been implicated in NHL, including Epstein-Barr (particularly in the immunocompromised host), Helicobacter pylori, HTLV-1, and Kaposi Sarcoma herpesvirus. Burkitt’s lymphoma is associated with the presence of
the Epstein-Barr virus. The HTLV-1 virus has been implicated in some adult T-cell lymphomas, especially in those occurring in the Caribbean, parts of South Africa, and southwestern Japan. The HTLV-1 infection has also been detected in AIDS patients who develop lymphomas.
the Epstein-Barr virus. The HTLV-1 virus has been implicated in some adult T-cell lymphomas, especially in those occurring in the Caribbean, parts of South Africa, and southwestern Japan. The HTLV-1 infection has also been detected in AIDS patients who develop lymphomas.
DIAGNOSTIC CRITERIA
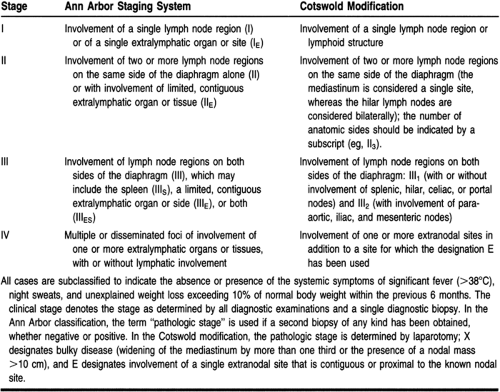
Lymphomas are diagnosed and categorized by the histologic exam of an excised lymph node. Both HD and NHL are staged via the Ann Arbor system (Table 38-2). This classification does not account for changes in histology, bulky disease, or extranodal involvement, all of which are important prognostic indicators in NHL. The Cotswold additions, which address bulk and site of disease, make this system much more useful for staging NHL.
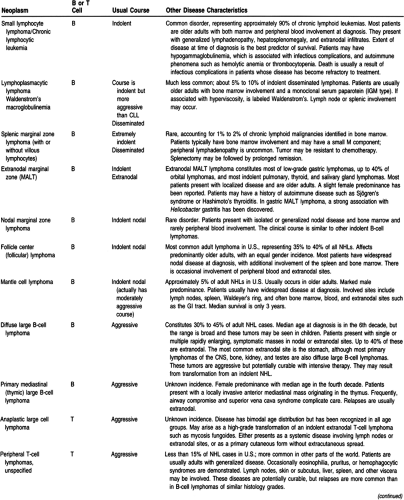
Lymphomas are classified by cell type. NHL classifications are presented in Table 38-3. This new system includes lymphomas that have been reclassified or newly recognized. There is currently a version of lymphoma classification under development.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree