Cumulative Trauma Disorder
Nancy S. Morris PhD, RN, CS, ANP
Cumulative trauma disorder (CTD) is a collective term for a range of soft-tissue injuries and conditions that primarily involve tendons, tendon sheaths, muscles, or nerves and are characterized by discomfort, paresthesia, numbness, weakness, impairment, or persistent pain in the joints, muscles, tendons, and other soft tissues, with or without physical manifestations. Although they have been described in the literature since the 1700s, CTDs have received increased attention over the last 10 to 15 years because of changes in occupational and recreational activities, as well as advances in the field of ergonomics. The legal profession and issues of workers compensation have also been driving factors in this resurgence. This chapter focuses on the common CTDs of the upper extremity that a primary care provider is likely to encounter.
Many common daily activities at home, at work, and in the community require functional upper extremities. The upper extremities are used to perform basic activities such as dressing and eating, to communicate with others through gesturing and writing, to operate machinery and recreational equipment, and to meet the many demands inherent in a tactile world. When the upper extremity cannot function as desired because of pain, weakness, numbness, or paresthesias, problems can occur. Concerns may arise regarding ability to meet demands at home, at work, and in social or recreational situations. Given the impact that upper extremity dysfunction can have, thorough evaluation, proper diagnosis, and adequate treatment are essential.
ANATOMY, PHYSIOLOGY, AND PATHOLOGY
Anatomy and Physiology
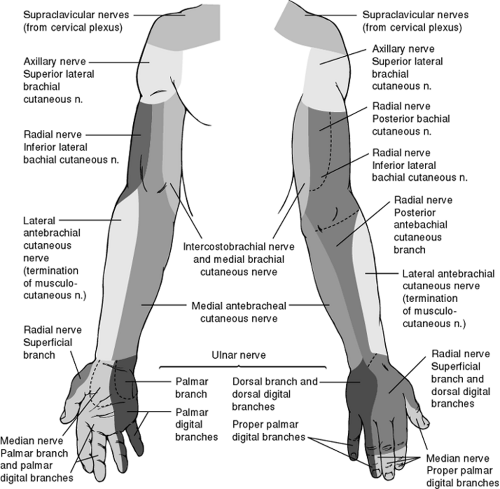
The provider needs a working knowledge of the bones, muscles, tendons, nerves, and vessels of the upper extremity, neck, and back (Figures 44-1, 44-2, 44-3, and 44-4). The hand is innervated by the median, ulnar, and radial nerves. Each nerve passes through a muscle in the forearm, and each passes through potential points of entrapment. These nerves are involved in the control of the wrist, fingers, and thumbs. The sensory branches of the nerves are depicted in Figure 44-5.
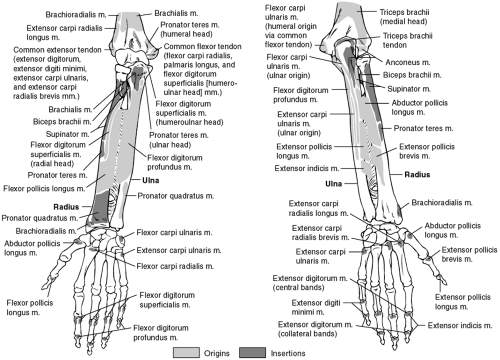 FIGURE 44-1 Muscles of forearm. (Adapted from the Ciba Collection of Medical Illustrations by Frank Netter, MD ) |
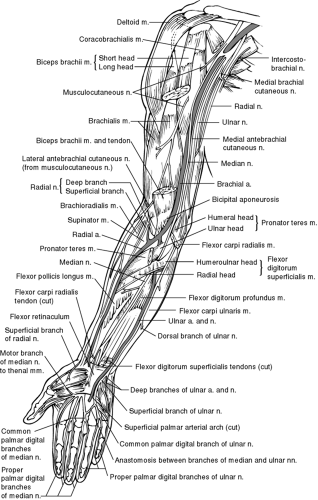 FIGURE 44-2 Arteries and nerves of upper limb (anterior view). (Adapted from the Ciba Collection of Medical Illustrations by Frank Netter, MD ) |
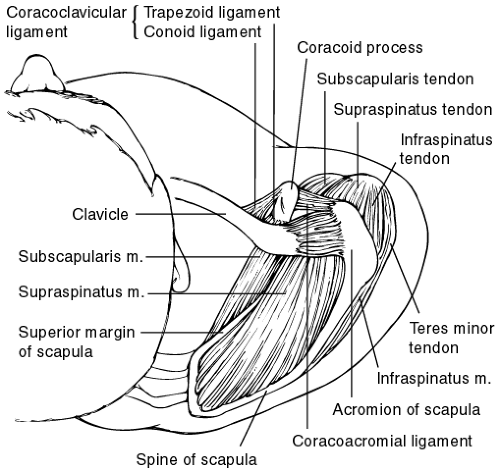 FIGURE 44-3 Shoulder and acromioclavicular joints. (Adapted from the Ciba Collection of Medical Illustrations by Frank Netter, MD ) |
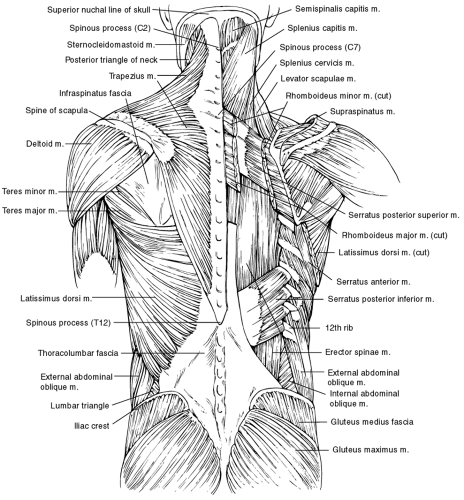 FIGURE 44-4 Musculature of back. (Adapted from the Ciba Collection of Medical Illustrations by Frank Netter, MD ) |
Pathology
Although the etiology of CTDs remains controversial, there are two distinct views emerging. One perspective is that CTDs are the result of a musculotendinous injury caused by force, repetition, abnormal postures, and vibrations over time. The second perspective is that psychosocial and political factors account for conditions identified as CTDs. A single explanation for the diversity of disorders and the multiplicity of symptoms is lacking, but there is consensus that these disorders develop gradually and are not the result of a single episode of trauma (Armstrong et al, 1987a; Higgs et al, 1993; Mackinnon & Novak, 1994; Putz-Anderson, 1988).
PHYSIOLOGIC PERSPECTIVE
Three hypothesis support the perspective that CTDs are a result of a musculotendinous injury (Mackinnon & Novak, 1994). The first hypothesis purports that muscle and tendon overuse is the primary etiology of CTDs. The second hypothesis maintains that there is a neurogenic origin to CTDs. The third hypothesis is based on an integration of neuropathic compression, myofascial pain, and muscle imbalance. A summary of each is provided below.
Muscle and Tendon Overuse
The premise behind the first hypothesis is that pain results directly from an overused muscle or as a result of pathologic changes that occur in the muscle fibers of overused muscles. With repetitive motion, there is reduced relaxation and increased tension in these tissues, reducing essential blood supply. This can lead to a rapid rate of wear and tear, with a greatly reduced ability to repair. Over time, a cumulative overload results in inflammation, edema, compression, ischemia, tearing, and fibrosis of affected tissues.
When muscles hold their contraction at more than about 15% to 20% of their maximal capability, they pull on their tendons and compress their joints, which decreases the blood supply to the tissues (Hebert, 1993). This can result in tissue ischemia and delayed dissipation of metabolites, causing irritation and inflammation. Additionally, overstrain of the muscles can cause microtears at the tendinous insertions; this leads to less diffusion, which causes a relative ischemia and subsequent inflammation at the tendon insertion. This results in mechanical attrition, a thickening of the tendon with irregular surfaces, and further abrasions and tearing (Childre & Winzeler, 1995). When there is insufficient time between episodes of heavy usage for a tissue to recover or repair itself, CTD can occur (Frederick, 1992; Hebert, 1993).
When a muscle or tendon unit is repeatedly tensed, the end result can be tendinitis. Tendons have both a biomechanical and a physiologic response to stressors. Tendons function as mechanical links that transmit forces, stabilize movements, and move the kinematic chains of the extremities. Consequently, tendons are subjected to tensile stresses by the muscle and to compressive and shearing stresses from adjacent bones and ligaments. Tendons respond mechanically to these stresses; if the stresses exceed a certain point, the tendons can become deformed.
Normal tendon structure can be disrupted in response to three stressors: tension, compression, and abrasion secondary to friction (Gross, 1992). Mechanisms of injury may involve stressors that are too high in magnitude, too frequent in repetition, or both. Local mechanical stresses can also irritate tendons via excessive force or high frequency of physical contact between soft tissues and an object or tool in the work environment.
Tendons also respond physiologically to stressors. Physiologic responses include metabolic, circulatory, and adaptive changes in the accessory tissues, synovial and mesenteric membranes, and adjacent ligaments. The changes are likely to be related to the occlusion of blood flow and the subsequent deprivation of nutrients that can occur with compression of a tendon against adjacent surfaces, thickening of tendon sheaths, or increased diffusion distances because of thickened sheaths (Manske et al, 1985). The amount of deprivation is a result of the intensity, duration, and frequency of exertion, or the forcefulness and repetitiveness of the activity (Armstrong et al, 1987a).
Many of the tendons in the upper extremity are surrounded by a sheath that contains synovial fluid. This allows easy gliding of the tendon within its sheath. If there is insufficient fluid in the sheath, overuse may lead to friction between the tendon and sheath, initiating the protective response of inflammation. The tendon area will swell and feel warm, tender, and painful. Movement is limited as a result of increased muscle tension and muscle spasm. If this occurs repeatedly, the frequent episodes of acute inflammation may prompt the formation of extraneous fibrous tissue, which is largely responsible for establishing a permanent or chronic condition. Chronic overuse often results in a thickened tendon sheath that impedes tendon movement, particularly in tight areas such as the wrist and fingers.
Compression Neuropathy
A second hypothesis points to a neurogenic origin for cumulative trauma disorders, targeting multilevel compression neuropathy as the primary etiology. The mechanism by which acute compression affects the peripheral nerve is not completely understood but is thought to involve both ischemic and mechanical factors. Nerve entrapment syndromes result from repeated or sustained compression of a peripheral nerve between ligaments or constricted anatomic structures. In addition to external compression, nerve entrapment may also be caused, aggravated, or precipitated by posture (Mackinnon & Novak, 1994).
It is proposed that the hypoxia from compression of the blood supply by muscles and tendons leads to problems with the nerves (Mackinnon & Novak, 1994; Ranney, 1993). With compression of a nerve, there is obstruction of venous return.
The increased venous pressure results in slowed circulation in the nerve complex and dilatation of the small vessels and capillaries within the nerve segment. There is edema, proliferation of fibroblasts, and scarring in the nerve segment, which compresses the nerve (Childre & Winzeler, 1995).
The increased venous pressure results in slowed circulation in the nerve complex and dilatation of the small vessels and capillaries within the nerve segment. There is edema, proliferation of fibroblasts, and scarring in the nerve segment, which compresses the nerve (Childre & Winzeler, 1995).
Critics of this hypothesis raise concerns regarding lack of an explanation for the etiology of the muscular component seen with CTDs.
Neuropathic Compression, Myofascial Pain, and Muscle Imbalance
The third hypothesis is an integration of the existing hypotheses relating to neuropathic compression and myofascial pain, with the addition of muscle imbalance (Higgs & Mackinnon, 1995; Mackinnon & Novak, 1994). The basic tenet of this hypothesis is that prolonged and frequent assumption of abnormal postures, positions, or movements of the head, neck, and upper extremity has two major influences on the body. First, specific
extremity positions cause increased pressure around certain nerves and, if encountered frequently and for long periods, will eventually result in chronic nerve compression. Both chronic tension and direct mechanical compression decrease blood flow to the nerve, producing fibrosis in and around the nerve; this in turn inhibits full excursion during normal extremity movement. In addition, placing the nerve on stretch will cause increased tension within the nerve, provoking symptoms from both sensory and motor fibers. Nerve compression at one point along the nerve may cause both distal and proximal sites to be less tolerant to the effects of compression. Chronic nerve compression is thought to be progressive unless specific interventions are initiated.
extremity positions cause increased pressure around certain nerves and, if encountered frequently and for long periods, will eventually result in chronic nerve compression. Both chronic tension and direct mechanical compression decrease blood flow to the nerve, producing fibrosis in and around the nerve; this in turn inhibits full excursion during normal extremity movement. In addition, placing the nerve on stretch will cause increased tension within the nerve, provoking symptoms from both sensory and motor fibers. Nerve compression at one point along the nerve may cause both distal and proximal sites to be less tolerant to the effects of compression. Chronic nerve compression is thought to be progressive unless specific interventions are initiated.
Second, abnormal postures can result in a set of muscles being maintained and used in shortened positions, which can lead to muscle imbalance. Underuse of some muscles subsequently leads to a weak set of muscles; this ultimately results in a compensatory overuse of a second set of muscles, and a cycle of muscle imbalance will be established. The muscles maintained and used in shortened positions become tight and painful, especially when stretched. Some muscles secondarily compress neurovascular structures when in a tightened position. It is this self-perpetuating cycle of tight muscles becoming tighter and weak muscles becoming weaker that explains why rest alone will not relieve all the symptoms of CTDs (Mackinnon & Novak, 1994).
NONPHYSIOLOGIC PERSPECTIVE
The second perspective on CTDs is denial of their very existence. Proponents of this explanation (Ferguson, 1987; Hadler, 1990; Ireland, 1995; Lam, 1995; Ranney, 1993; Weiland, 1996) believe that CTDs are not primarily physiologic in nature but rather are based on psychosocial and sociopolitical factors. As such, they suggest that CTDs are a reflection of modern society without clearly identifiable pathology. The difficulty in the objective determination of the work-relatedness of CTDs and the frequently associated financial compensation factor add to the difficulty of accepting CTD as a diagnosis. For the most part, supporters of this perspective recommend that syndromic titles such as CTD be abandoned in favor of clearly definable and diagnosable entities with a known histologic appearance and etiology.
Although there are different perspectives on the causative factors of CTDs, all but the psychosocial theory accept that both biomechanical and physiologic factors are involved. Most would agree that repeated or sustained exertion, in combination with certain postures, causes, precipitates, or aggravates chronic upper extremity tendon and nerve disorders. Additional contributing factors may include the force used in performing movements, increased muscle tension associated with mental stress, and factors external to the person (eg, faulty work station, equipment, task design, and maintenance of equipment).
EPIDEMIOLOGY
The overall incidence and prevalence of CTDs, as well as the distribution and determinants, are difficult to ascertain. No definition of CTD has been agreed on. Use of such a broad term does not specify the exact anatomic or pathologic involvement. This creates difficulty when the provider is pressed to determine an etiology and recommend a treatment plan. To complicate matters, there are several terms used synonymously with CTD, including repetitive strain injuries, overuse syndromes, and repetitive motion injuries. For clarity, the term CTD is used throughout this chapter.
In addition to variations in diagnostic terminology and criteria, differences in attitudes of health care providers about reporting CTDs contribute to the inadequacies of the epidemiologic data. Many of the published data involve occupation-related CTDs, but occurrence can also be related to intrinsic factors of the person and recreational activities. The epidemiologic literature also separates clinically well-defined disorders such as tendinitis and carpal tunnel syndrome from the more nonspecific diagnoses referred to as CTDs (Hales & Bernard, 1996).
The Bureau of Labor Statistics (U.S. Department of Labor, 1995) reports that the incidence rates for CTDs increased from 5.1 to 39 cases per 10,000 full-time workers from 1984 to 1994. This change is attributed to increased awareness among employees, employers, and health care providers that these disorders may be work-related, thereby resulting in more complete recording and an actual increase in the number of cases (Hales & Bernard, 1996). Given the inconsistencies in reporting and the occurrence of CTDs that are not work-related, these data are most useful for interpreting trends and identifying high-risk industries.
The prevalence of upper extremity CTDs depends on the occupation studied, the risk factors present, and the specific body part studied. The recent increase in prevalence may be related to ergonomic factors. Nearly two thirds of all occupational illnesses reported to the Bureau of Labor Statistics in 1994 were caused by exposure to repeated trauma to the upper body (wrist, elbow, or shoulder) (U.S. Department of Labor, 1996). The following five industries have had the highest rank of CTDs during the last 10 years: meat packing, knit underwear manufacturing, automobile manufacturing, poultry processing, and house slipper manufacturing (U.S. Department of Labor,
1995). However, the reporting of CTDs is inconsistent, and there may be other industries with a high occurrence.
1995). However, the reporting of CTDs is inconsistent, and there may be other industries with a high occurrence.
Many factors, both occupational and nonoccupational, have been reported to cause, precipitate, or aggravate conditions categorized as CTDs. The specific contribution of occupational and nonoccupational factors has not been determined. Occupational factors include repetitive motion, forceful exertions, mechanical insult, sustained and awkward postures, and frequent exposure to low-frequency vibrations and cold temperatures, as well as lack of training and experience, poor work station design, and inappropriate tools. The association of job demand and workplace psychosocial factors should also be considered. Factors that have the most consistent association include high workloads, perceived time pressure, work pressure, high workload variability, poor work content, and monotonous work (Hales & Bernard, 1996). Examples of nonoccupational factors thought to contribute to CTDs include congenital defects, use of birth-control pills, pregnancy, chronic disease, and recreational factors (Armstrong et al, 1987a; Hebert, 1993; Kroemer, 1992; Putz-Anderson, 1988). There are few epidemiologic data available to determine how age relates to CTDs; the influence of age and gender on the susceptibility to CTDs is controversial.
DIAGNOSTIC CRITERIA
CTDs include a variety of familiar clinical entities, such as tenosynovitis, tendinitis, epicondylitis, trigger finger, and carpal tunnel syndrome, as well as vague complaints of pain. Assessment and management of these familiar conditions are better
understood in contrast to the more challenging and often perplexing disorders associated with compressive neuropathies and nonspecific complaints of pain. The major problem in assessing and managing CTDs occurs when paresthesias are accompanied by ambiguous complaints, such as pain in the entire upper extremity, neck, back, subscapular area, and shoulder (Higgs & Mackinnon, 1995).
understood in contrast to the more challenging and often perplexing disorders associated with compressive neuropathies and nonspecific complaints of pain. The major problem in assessing and managing CTDs occurs when paresthesias are accompanied by ambiguous complaints, such as pain in the entire upper extremity, neck, back, subscapular area, and shoulder (Higgs & Mackinnon, 1995).
Diagnosis is based on a careful history, physical exam, and the exclusion of other well-described entities. There are no specific pathologic or radiologic features to support a diagnosis of CTD, and definitive diagnostic criteria have not been established. There is, however, a distinct history that is suggestive of CTD:
Symptoms come on gradually.
Symptoms worsen over weeks, months, or even years.
Initially the symptoms may subside with rest, but as time goes on, symptoms worsen and are no longer relieved with rest (Armstrong et al, 1987a; Higgs et al, 1993; Mackinnon & Novak, 1994; Putz-Anderson, 1988).
Subjective and objective signs and symptoms consistent with the diagnosis of CTD include:
Soft-tissue swelling and muscle atrophy
Pain and tenderness
Decreased range of motion
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree