high compared with the rest of the body. The temperature in this compartment can be evaluated in the pulmonary artery, distal esophagus, tympanic membrane, or nasopharynx. Even during rapid thermal perturbations (e.g., cardiopulmonary bypass), these temperature monitoring sites remain reliable, although the rectal site also provides a reliable estimation of Tc during regional anesthesia.1
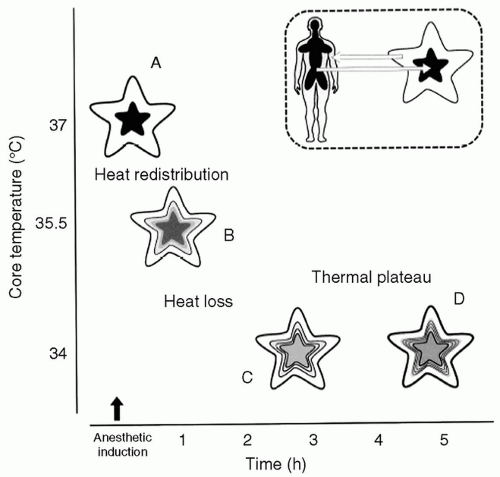 FIGURE 45.1 Schematic presentation of the three phases of intraoperative hypothermia, based on data from Matsukawa et al.4 and Kurz et al.3 The human body, as shown in the inset, is denoted by a 5-limb star with a dense black core representing the high-heat central thermal compartment and a low-heat surrounding gray area indicating the peripheral tissues. A: The typical preoperative patient is vasoconstricted with a large core-to-peripheral tissue temperature gradient and a clear distinction between the two thermal compartments. B: After anesthesia-induced peripheral vasodilation, heat driven by the temperature gradient flows toward the periphery of the body. Therefore, core temperature decreases, and the two body compartments become more homogeneous (redistribution hypothermia, A→B). C: Radiation- and convection-mediated losses have the higher impact on systemic heat balance during the linear phase in the core temperature decrease (B→C). At this point, hypothermia activates thermoregulatory vasoconstriction in an effort to constrain heat in the body core and restore the normal core-to-periphery temperature gradient. D: During thermal plateau (C→D), core temperature becomes stable or even increases slightly. However, the total heat content of the body continues to decline, largely at the expense of the peripheral thermal compartment. (Data from: Matsukawa T, Sessler DI, Sessler AM, et al. Heat flow and distribution during induction of general anesthesia. Anesthesiology. 1995;82:662 and Kurz A, Sessler DI, Christensen R, et al. Heat balance and distribution during the core-temperature plateau in anesthetized humans. Anesthesiology. 1995;83:491.) |
surfaces through the kinetic energy of molecules being transferred to adjacent molecules. The constant flow of air surrounding the patient in the operating room facilitates conduction and results in the convection current, which carries heat away from the body.2,7
TABLE 45.1 Major Clinical Consequences of Mild Perioperative Hypothermiaa | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








