Safety and Hazards Associated with Tracheal Intubation and Use of Supralaryngeal Airways
David Ferson
Linda Chi
Sonal Zambare
Wendy Botnick
CASE SUMMARY
A 42-year-old male patient was scheduled for an arthroscopic knee surgery under general anesthesia. The patient’s medical history was unremarkable except for mild seasonal asthma. Height and weight were 180 cm and 80 kg, respectively. In the operating room, general anesthesia was induced with midazolam, fentanyl, and propofol. A supraglottic airway device was inserted easily on the first attempt. The cuff was inflated with air to the maximum volume recommended by the manufacturer. Intracuff pressure was neither measured nor monitored during the course of surgery. Anesthesia was maintained with desflurane. At the conclusion of surgery, which lasted for 130 minutes, the patient was awakened, and the supraglottic airway was removed without incident. The patient was then transferred to the recovery room. Shortly after arrival, he complained of dysphagia. A specialist in head and neck surgery was consulted and, after performing a flexible nasal fiberoptic laryngoscopy, bilateral hypoglossal nerve palsy was diagnosed. A swallowing study demonstrated an uncoordinated swallowing reflex. Because of the risk for aspiration, a nasogastric tube was placed for enteric feeding. The patient’s symptoms improved gradually and on the 16th postoperative day, another swallowing study demonstrated near normal function. The nasogastric tube was removed. Despite enteric feeding, the patient lost 15 lb over 2 weeks. After 21 days, the symptoms of hypoglossal nerve palsy resolved completely.
▪ INTRODUCTION
One of the most critically important perioperative functions of the anesthesiologist is establishing and maintaining a patent airway. To achieve this goal, the anesthesiologist usually inserts an airway device to facilitate spontaneous, assisted, or controlled ventilation. There are two distinctly different categories of airway devices—supralaryngeal and tracheal. Supralaryngeal airways (SLAs) do not descend below the vocal cords, whereas tracheal tubes are always positioned below the vocal cords, within the lumen of the trachea. Additionally, currently available SLAs can only be inserted orally, but tracheal tubes can be inserted through oral or nasal routes.
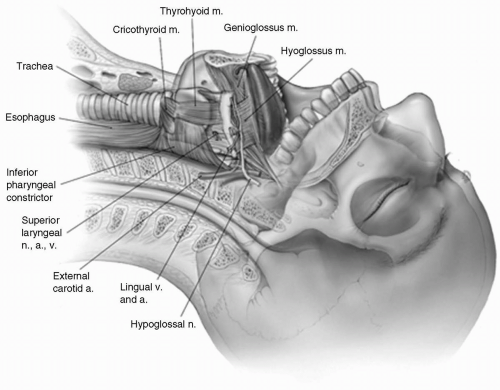
Complications can occur with the insertion of both types of airway devices, and short- and long-term adverse effects have been described in the literature (see Fig. 7.1). This chapter will focus on the major hazards associated with tracheal intubation and SLA use, how to diminish the risk of complications, and, most important, how to manage complications if they occur.
▪ HAZARDS ASSOCIATED WITH TRACHEAL INTUBATION
MacEwen first described tracheal intubation for mandibular surgery in 1878; however, the current techniques of tracheal intubation were not developed, refined, and popularized until the 1920 and 1930s.1,2,3,4 Subsequently, the development of different laryngoscopic blades has corresponded with major improvements in tracheal tube technology. Currently, tracheal intubation is the most widely used method of airway management; therefore, it stands to reason that its complications have been described numerous times in the literature. These can be grouped into the following categories following a procedural timeline: (i) Complications that result from direct laryngoscopy and intubation, (ii) complications that result from the pressure of the tracheal tube or cuff on airway structures, and (iii) complications following extubation.
How Can Complications Be Induced through Direct Laryngoscopy and Intubation?
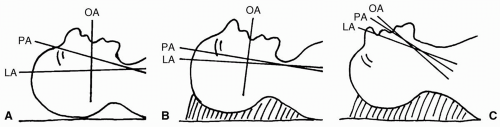
Tracheal intubation under direct observation requires visualization of the glottic opening and is usually achieved
with a rigid laryngoscope. Although several types of laryngoscopic blades have been introduced over the years, they all have similar features designed to displace soft tissues of the neck to create a line of sight from the mouth to the larynx (see Fig. 7.2). In an attempt to optimize visualization and minimize the angle between the oral, pharyngeal, and laryngeal axes, the laryngoscopist must flex the patient’s neck and extend the head. Complications related to such head and neck manipulations during rigid laryngoscopy have been described in patients with unrecognized cervical spine injury and in patients with degenerative disease of the cervical spine.5,6,7 Also, rigid laryngoscopy elicits an autonomic response in patients, and complications related to hemodynamic responses to rigid laryngoscopy and tracheal intubation are well documented.8,9 One of the relatively infrequent complications of tracheal intubation is failure to place the tracheal tube inside the trachea, which occurs in patients with unexpected or unrecognized difficult-to-manage airways. Although this complication is rare, it carries a serious risk because failure to ventilate and oxygenate the patient can result in brain damage or death. In addition, rigid laryngoscopy and tracheal intubation can cause trauma to the pharynx, larynx, or esophagus, even when the laryngoscopy and intubation are perceived as not difficult.
with a rigid laryngoscope. Although several types of laryngoscopic blades have been introduced over the years, they all have similar features designed to displace soft tissues of the neck to create a line of sight from the mouth to the larynx (see Fig. 7.2). In an attempt to optimize visualization and minimize the angle between the oral, pharyngeal, and laryngeal axes, the laryngoscopist must flex the patient’s neck and extend the head. Complications related to such head and neck manipulations during rigid laryngoscopy have been described in patients with unrecognized cervical spine injury and in patients with degenerative disease of the cervical spine.5,6,7 Also, rigid laryngoscopy elicits an autonomic response in patients, and complications related to hemodynamic responses to rigid laryngoscopy and tracheal intubation are well documented.8,9 One of the relatively infrequent complications of tracheal intubation is failure to place the tracheal tube inside the trachea, which occurs in patients with unexpected or unrecognized difficult-to-manage airways. Although this complication is rare, it carries a serious risk because failure to ventilate and oxygenate the patient can result in brain damage or death. In addition, rigid laryngoscopy and tracheal intubation can cause trauma to the pharynx, larynx, or esophagus, even when the laryngoscopy and intubation are perceived as not difficult.
Why Should Patients Be Evaluated Anatomically before Intubation?
Patients with unrecognized cervical spine injury and patients with degenerative disease of the cervical spine are at risk for neurological complications, which can range from minor and transient sensory and motor deficits to severe neurological impairments resulting from spinal cord trauma.10,11,12 Therefore, it is imperative, before intubation, to evaluate the integrity of the cervical spine in all trauma victims. Helical computed tomography (CT), a recently developed imaging technique, is particularly useful in evaluating the integrity of the cervical spine and detecting even small fractures that can be easily missed by conventional radiography.13 The information acquired from a helical CT is volumetric, compared with a single slice in conventional CT; therefore, the entire anatomical region of interest can be scanned during a single breathhold. The volumetric information obtained by the helical CT scan also increases the chances of detecting small lesions and allows for better three-dimensional reformatting, which enables clinicians to view the anatomy in a
manner that is more applicable to their level of training (see Fig. 7.3). Furthermore, because of the higher speed of data acquisition possible with helical CT, misregistration and image degradation caused by patient motion is less of an issue. This is especially important when scanning uncooperative patients and trauma victims. In emergency cases, however, when there is no time to perform radiological studies, it is important to minimize head and neck movement by having a skilled assistant apply in-line stabilization to the head and neck throughout the intubation. This maneuver, when properly performed, minimizes the flexion-extension movement and also decreases the rotation of the cervical spine.14
manner that is more applicable to their level of training (see Fig. 7.3). Furthermore, because of the higher speed of data acquisition possible with helical CT, misregistration and image degradation caused by patient motion is less of an issue. This is especially important when scanning uncooperative patients and trauma victims. In emergency cases, however, when there is no time to perform radiological studies, it is important to minimize head and neck movement by having a skilled assistant apply in-line stabilization to the head and neck throughout the intubation. This maneuver, when properly performed, minimizes the flexion-extension movement and also decreases the rotation of the cervical spine.14
Laryngoscopy can also be particularly challenging in patients with degenerative disease of the cervical spine. This is because, in these patients, the movement of the cervical spine is restricted or impossible, and therefore, the optimal intubating position cannot be obtained. The most common diseases in this group of patients are ankylosing spondylitis, diffuse idiopathic skeletal hyperostosis, and osteoarthritis. Also, the presence of cervical osteophytes can make visualization of the cords and passage of the tube very difficult. In patients with restricted mobility of the cervical spine, intubation is perhaps best achieved with the use of specialized equipment that is, a fiberoptic bronchoscope, video laryngoscope, or fiberoptically equipped intubating laryngeal mask airway (C-Trach LMA; LMA NA, San Diego, CA).
What Type of Adverse Hemodynamic Responses Can Be Elicited by Laryngoscopy and Intubation?
Typically, direct laryngoscopy requires little force to displace the soft tissues and visualize the glottic entry. However, when intubation is difficult, excessive force is usually required. Hemodynamic response to even routine laryngoscopy and intubation can vary significantly among patients.15 Most patients are reported to have transient tachycardia and hypertension during laryngoscopy. These conditions are usually short-lived in nature and are not associated with any significant morbidity. However, in a patient with known cardiovascular disease, even a short duration of tachycardia and hypertension can lead to myocardial ischemia, arrhythmias, or even myocardial infarction.16 Various drugs have been used to abate this detrimental cardiovascular response.17 Short-acting β-blockers such as esmolol and calcium channel blockers such as intravenous nicardipine have been shown to be very effective in reducing tachycardia and hypertension caused by laryngoscopy and intubation.18,19 However, these agents, while attenuating the hemodynamic responses, may result in excessive negative ionotropic and chronotropic action that precipitates cardiac failure in susceptible patients. Various other techniques, such as injecting lidocaine through an intratracheal or intravenous route immediately before intubation, have been described, but none has been proved to be completely reliable and effective.20,21 Therefore, it is essential to use a combination of anesthetic and adjuvant agents to ensure that the patient is adequately anesthetized before instrumenting the airway. This is particularly important in patients with increased intracranial or intraocular pressure, in whom the exaggerated hemodynamic responses can lead to catastrophic consequences.22,23,24,25
What Complications Are Related to Difficult or Failed Intubation?
Several anatomical characteristics and clinical syndromes associated with difficult intubation are described
extensively in a separate chapter of this textbook. Therefore, in this chapter we will not discuss the evaluation and management of these patients. However, it is important to remember that excessive force during direct laryngoscopy in patients with difficult-to-manage airways frequently results in tooth damage and trauma to the soft tissues and cartilaginous and bony structures of the larynx. Because it is difficult to predict, in any patient, how much force applied during laryngoscopy will result in trauma to the pharyngeal and laryngeal structures, it seems logical that if visualization of the larynx is difficult, one should switch to a different laryngoscopic blade or consider an alternative technique for intubation instead of increasing the amount of force while continuing to use a technique that has already failed.26 In 1993, the American Society of Anesthesiologists (ASA) established guidelines for taking care of patients with difficult-to-manage airways and published a difficult airway algorithm. The ASA guidelines and the difficult airway algorithm provide an excellent framework for developing an organized approach to patients with difficult-to-manage airways that can be easily integrated into clinical practice during elective and emergency airway-related situations.27 In 2003, the guidelines and the algorithm were revised and updated. Specifically, the new algorithm has expanded the uses of the laryngeal mask airway (LMA Classic; LMA North America, San Diego, CA) in patients with difficult-to-manage airways.28
extensively in a separate chapter of this textbook. Therefore, in this chapter we will not discuss the evaluation and management of these patients. However, it is important to remember that excessive force during direct laryngoscopy in patients with difficult-to-manage airways frequently results in tooth damage and trauma to the soft tissues and cartilaginous and bony structures of the larynx. Because it is difficult to predict, in any patient, how much force applied during laryngoscopy will result in trauma to the pharyngeal and laryngeal structures, it seems logical that if visualization of the larynx is difficult, one should switch to a different laryngoscopic blade or consider an alternative technique for intubation instead of increasing the amount of force while continuing to use a technique that has already failed.26 In 1993, the American Society of Anesthesiologists (ASA) established guidelines for taking care of patients with difficult-to-manage airways and published a difficult airway algorithm. The ASA guidelines and the difficult airway algorithm provide an excellent framework for developing an organized approach to patients with difficult-to-manage airways that can be easily integrated into clinical practice during elective and emergency airway-related situations.27 In 2003, the guidelines and the algorithm were revised and updated. Specifically, the new algorithm has expanded the uses of the laryngeal mask airway (LMA Classic; LMA North America, San Diego, CA) in patients with difficult-to-manage airways.28
▪ TOOTH DAMAGE
If tooth damage occurs during laryngoscopy, one should obtain a dental consultation in the postoperative period. More important, if a tooth is dislodged into the patient’s airway during laryngoscopy, it is imperative to retrieve it from the pharynx before inserting an endotracheal tube to avoid pushing the tooth into the trachea or bronchi. If the tooth does become wedged into the bronchus, one needs to perform fiberoptic bronchoscopy immediately, using
a large diameter bronchoscope, and retrieve the tooth using a special forceps, which can be passed through the working channel of the bronchoscope. Undetected aspiration of a tooth into a mainstem bronchus can lead to lung collapse, hypoxemia, and formation of a lung abscess.29,30,31
a large diameter bronchoscope, and retrieve the tooth using a special forceps, which can be passed through the working channel of the bronchoscope. Undetected aspiration of a tooth into a mainstem bronchus can lead to lung collapse, hypoxemia, and formation of a lung abscess.29,30,31
▪ TRAUMA TO SOFT TISSUES
Trauma to the soft tissues of the pharynx and larynx during intubation is very common and is usually the result of excessive force used during laryngoscopy and/or poor intubation technique.32 In the postoperative period, patients who have had soft tissue trauma may complain of prolonged sore throat and difficulty in swallowing. Also, there may be bleeding associated with soft tissue trauma. In more severe cases, when the integrity of the pharyngeal wall has been compromised, a pharyngeal abscess may form.33 If trauma causes an esophageal rupture, this may lead to mediastinitis, which carries a high mortality risk in the postoperative period.34
▪ TRAUMA TO THE CRICOARYTENOID JOINT
Although trauma to the cricoarytenoid joint occurs in only 0.023% of patients, it represents a serious complication.35 Subluxation of the arytenoid cartilage may occur during both difficult and uncomplicated intubation. Forces on the arytenoid cartilage exerted by the laryngoscope blade or by the distal part of the endotracheal tube may cause anterior and inferior displacement of the arytenoid cartilage. The left arytenoid cartilage is affected most frequently during conventional rigid laryngoscopy. In contrast, posterolateral subluxation results from the pressure exerted on the posterior glottis by the convex part of the shaft of the tracheal tube.36 Systemic diseases such as chronic renal insufficiency, Crohn’s disease, and acromegaly may cause degeneration of the cricoarytenoid ligaments, thereby making the cricoarytenoid joint more susceptible to traumatic dislocation. Persistent voice changes, sore throat, and pain on swallowing may allude to the diagnosis of arytenoid dislocation. However, stridor and shortness of breath have also been observed. If pharyngolaryngeal complaints persist, however, evaluation by a laryngologist is mandatory. In addition to indirect and direct laryngoscopy, helical CT and electromyography of the larynx play an important role in differentiating arytenoid dislocation from true vocal cord paralysis due to nerve damage. There are several types of treatment for arytenoid cartilage dislocation, such as voice therapy, chemical splinting, and closed reduction. Early operative treatment results in a fair prognosis, whereas delayed diagnosis may lead to ankylosis of the cricoarytenoid joint with permanent impairment of the voice and possible compromised airway protection.
What Types of Problems Are Related to the Tracheal Tube and Its Cuff?
The presence of the tracheal tube itself can cause a number of complications, which include, but are not limited to, the esophageal or bronchial misplacement of the tracheal tube, pressure exerted by the tube and its cuff on the pharyngeal, laryngeal, and tracheal structures, and nosocomial infections.
▪ MISPLACEMENT OF THE TRACHEAL TUBE AND PRESSURE EXERTED BY THE CUFF
Esophageal or bronchial misplacement of the tracheal tube is not uncommon. Failure to recognize esophageal intubation can have a catastrophic outcome because it can lead to hypoxemia, gastric distension, regurgitation, and aspiration of acidic contents into the trachea leading to aspiration pneumonitis. Placing the tracheal tube too far into the mainstem bronchus can lead to hypoxemia and a decreased depth of anesthesia, because the uptake of inhaled anesthetic agents is impaired. In patients with severe lung disease, bronchial intubation can also lead to pneumothorax. Clinical vigilance, ballotment of the endotracheal tube cuff at the sternal notch, careful auscultation of both lung fields, and the use of pulse oximetry and capnography should help recognize tracheal tube misplacement and avoid further complications. However, only fiberoptic bronchoscopy can confirm optimal placement of the endotracheal tube.
▪ ASPIRATION
The aspiration of gastric contents into the respiratory tract is a serious complication of endotracheal intubations, and every effort should be made to prevent it. The use of prokinetic drugs and antacid, even in fasting patients, should prove helpful because they reduce the volume and pH of the gastric contents.
▪ PRESSURE
The presence of the tracheal tube and its cuff creates pressure on the tracheal mucosa. Although this problem has been addressed by developing low-pressure, high-volume cuffs, recent research has shown that this kind of cuff after inflation may form vertical channels, which may increase the chances of aspiration of gastric contents into the tracheobronchial structures.37,38 Special technology that uses a low-volume, low-pressure tracheal tube cuff
will hopefully solve the problems associated with mucosal pressure and also reduce the incidence of pulmonary aspiration.39
will hopefully solve the problems associated with mucosal pressure and also reduce the incidence of pulmonary aspiration.39
▪ NERVE INJURIES
There are also reports of nerve injuries caused by the inflated cuff.40 The nerves commonly affected are the recurrent laryngeal branch of the vagus nerve, the lingual nerve, and the hypoglossal nerve. These nerve injuries are usually temporary, and a complete recovery is possible, in most cases, within a couple of days. However, if symptoms persist, an otolaryngology consultation may be required to assess the function of the vocal cords and the coordination of the structures associated with swallowing. The clinical presentation of recurrent laryngeal nerve palsy can be identical to that of arytenoid subluxation or arytenoid dislocation caused by forceful laryngoscopy. Only special studies can distinguish between these two clinical complications. Whereas hypoglossal or recurrent nerve palsy can be diagnosed by nerve conduction studies, arytenoid displacement requires specialized CT scanning to establish the correct diagnosis. Cuff herniation used to be a common problem before the current standards for manufacturing endotracheal tubes were established. Currently, the cuff is firmly attached to the tube, and this complication is no longer seen.
What Hazards Are Inherent with Extubation?
Extubation carries a separate set of hazards and requires the same level of vigilance as does intubation. The main complications related to extubation include hypoxemia, airway obstruction, and aspiration. Several factors have been identified that lead to complications after extubation. Some are related to patient comorbidities, whereas others can be linked to the residual effects of anesthetic agents in the immediate postoperative period.41,42 Patients, who are at increased risk for complications after extubation include those with significant cardiopulmonary disease, those who have undergone major abdominal or thoracic surgery, and the morbidly obese. Therefore, the anesthetic plan should be tailored to each individual patient, taking into consideration all the factors that can significantly influence the immediate postoperative course in the recovery room.
Hypoxemia after extubation is usually multifactorial. The diagnosis should be established in a systematic manner and appropriate treatment implemented accordingly. The most common causes include a low inspired oxygen concentration, hypoventilation, alveolar ventilation-perfusion mismatch, increased shunt, and diffusion abnormalities. Also, the risk of hypoxemia is increased with the intraoperative use of long-acting anesthetic agents. Residual muscle relaxation plays an important role in postoperative hypoxemia. As demonstrated by several investigators, the incidence of residual muscle relaxation in the recovery room can be as high as 50%.43
What is most concerning is that despite the availability of modern neuromuscular blocking agents with short or intermediate durations of action, the incidence of residual neuromuscular blockade remains very high.44,45 Therefore, it is imperative that all patients satisfy extubation criteria (i.e., sustained head lift for more than 5 seconds or a strong handgrip) before removal of the tracheal tube. It has been found, however, that even after fulfilling the criteria for extubation, some patients may still have residual neuromuscular paralysis.46,47 This can have serious consequences, because the respiratory muscles and pharyngeal protective reflexes may not be functioning at optimal levels. Therefore, in patients who are at high risk for developing hypoxemia or upper airway obstruction and who have diminished respiratory reserve, residual muscle paralysis is especially dangerous and can lead to respiratory failure shortly after extubation.
Also, muscle weakness, hypoxemia, upper airway obstruction, and diminished pharyngeal reflexes increase the chances for aspiration in the immediate postoperative period.48 In addition to patient-related factors, prolonged neuromuscular blockade can be caused or aggravated by an acid-base imbalance, electrolyte abnormalities, the use of magnesium, renal or hepatic disease, and the administration of aminoglycosides, β-blockers, and calcium channel blockers.
▪ PULMONARY EDEMA
Another serious complication that occurs after extubation is acute pulmonary edema.49 This complication develops when the patient is trying to breathe while the upper airway is obstructed.50,51 Acute pulmonary edema is usually seen in younger patients who can generate high negative intrapleural pressure, which increases the pulmonary transcapillary hydrostatic pressure gradient. Movement of the fluid from the pulmonary vessels to the interstitial space exceeds the lymphatic drainage capacity. This, in combination with a compromised alveolar epithelial barrier, causes the alveolar flooding. Laryngeal spasm during emergence from general anesthesia accounts for most cases of acute postextubation, “negative-pressure” pulmonary edema. Primary clinical management considerations are the establishment of a patent airway and the maintenance of adequate arterial oxygenation using supplemental oxygen. Also, continuous positive airway pressure (CPAP) using a face mask or tracheal tube is necessary during the initial treatment phase of pulmonary edema. Tracheal reintubation is necessary to sustain the airway in more than 85% of adults and children. In most patients, short-term ventilatory support with supplemental oxygen is all that is required for treatment. However, when significant coex-isting cardiac comorbidities are present or when fluid overload occurs, diuretics and vasoactive agents may be indicated.
▪ HAZARDS ASSOCIATED WITH THE USE OF SUPRALARYNGEAL AIRWAYS
How Do Supralaryngeal Airways Differ from Other Airway Devices?
SLAs represent a class of medical devices designed to provide spontaneous, assisted, or controlled ventilation. SLAs differ from other airway devices, such as oropharyngeal airways and tracheal tubes, in that they do not require a facial seal or tracheal insertion for ventilation. The laryngeal mask airway (LMA Classic; LMA North America, San Diego, CA) was introduced into clinical practice in 1988 and became the first commercially successful SLA. Indeed, the LMA Classic has demonstrated that, for many patients in select clinical situations, the supraglottic airway approach is not only feasible, but also less invasive and more beneficial than endotracheal intubation.52 As a result of the clinical and commercial success of the LMA Classic, the following SLAs have been introduced into clinical practice: the cuffed oropharyngeal airway (COPA) (Mallinckrodt Medical; St Louis, MO), the pharyngeal airway express (PAEXPRESS) (Vital Signs, Inc., Totowa, NJ), the laryngeal tube (LT) (King System Corporation, Noblesville, IN), the Portex soft seal laryngeal mask (Portex-Soft Seal) (Portex Inc., Keene, NH), the perilaryngeal airway (COBRA) (Engineered Medical Systems, Indianapolis, IN), the Ambu laryngeal mask (AMBU-LM) (Ambu Inc., Linthicum, MD), and the streamlined liner of the pharynx airway (SLIPA) (SLIPAmed SA Pty Ltd, Cape Town, South Africa). Predictably, some of the new supraglottic airways are close replicas of the LMA Classic, whereas others differ significantly in their functional design. These design differences include the location and type of cuff, which serves as a sealing mechanism, the location of the ventilatory portion of the device, and whether there is an attempt to seal off the entrance to the esophagus. On the basis of an anatomical comparative analysis of currently available SLAs, they can be grouped into the categories as shown in Table 7.1.53 (Also see Figs. 7.4 to 7.10.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree