Sonoanatomy for interscalene block (ISB).
Landmarks
The patient is positioned supine with the head slightly rotated to the contralateral side on a pillow (Figure 10.2). The cricoid cartilage can be used as a landmark to identify the C5/6 vertebral level.
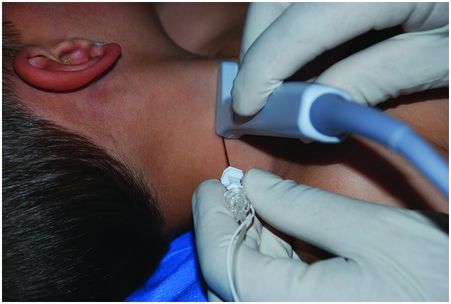
Patient position, probe placement, and in-plane needle approach.
Block performance
A high frequency probe should be used with the depth set to 2–3 cm, as the nerve roots are located superficially. The probe is placed about 2 cm cephalad and parallel to the clavicle. A slight caudal or cephalad tilting of the ultrasound probe may help improve visualization of the brachial plexus in the interscalene groove. A 25 mm needle is recommended for most children as the plexus is very superficial. A tangential caudal oriented needle approach from lateral to medial direction to the plexus is recommended to reduce the risk of needle injury to the spinal cord (Figure 10.2). The needle can be inserted in-plane or out-of-plane. The in-plane approach is described here. Firstly, the anterior and middle scalene muscles and the cervical nerve roots are visualized in the short axis (Figure 10.3). The needle is then advanced in a lateral to medial direction until the needle tip is located in the interscalene groove just lateral to the superficial brachial plexus nerve roots (Figure 10.4). Once the needle tip is in the correct position up to 0.5 ml/kg of 0.2% ropivacaine is injected under ultrasound guidance (maximum of 20 ml).
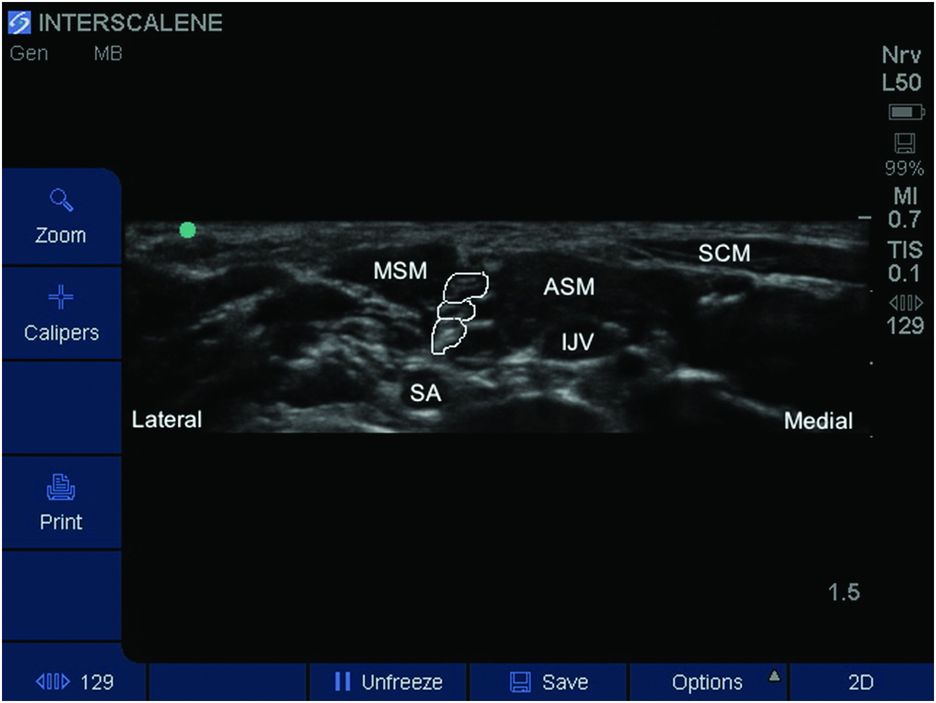
Labeled sonoanatomy for interscalene block (ISB). The roots of the brachial plexus are outlined. ASM, anterior scalene muscle; IJV, internal jugular vein; MSM, middle scalene muscle; SA, subclavian artery; SCM, sternocleidomastoid muscle.
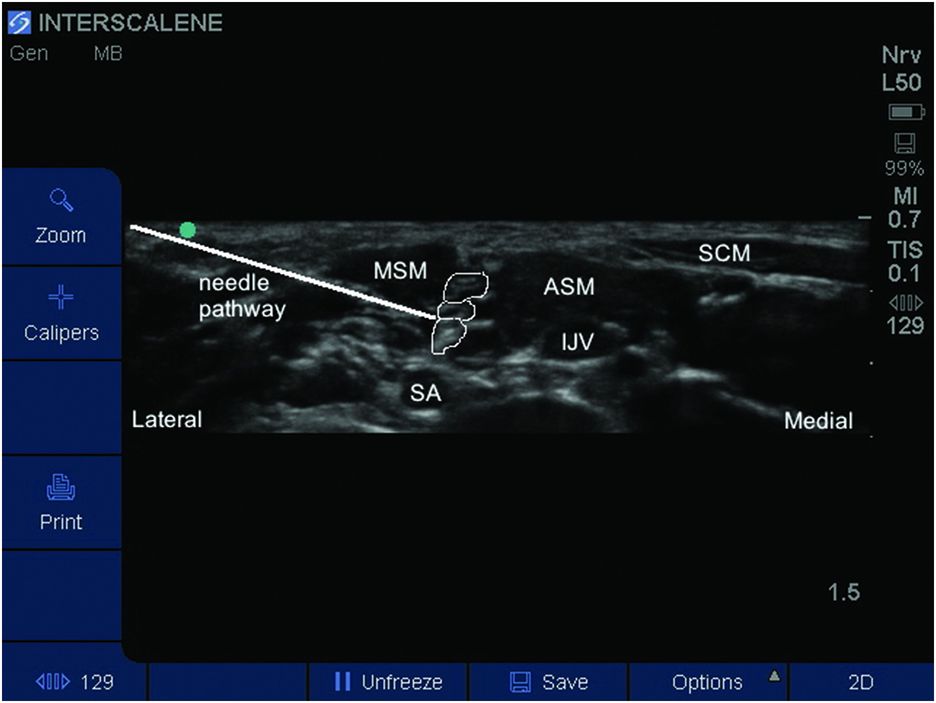
Needle pathway for in-plane interscalene block (ISB). ASM, anterior scalene muscle; IJV, internal jugular vein; MSM, middle scalene muscle; SA, subclavian artery; SCM, sternocleidomastoid muscle.
Continuous catheter technique
The modified lateral approach is the common technique for placement of a continuous ISB catheter (Borgeat et al., 2003). The patient position and probe orientation are similar to that of a single injection technique. Once the needle is positioned in the interscalene groove the needle tip location can be confirmed with nerve stimulation or by injecting a small amount of dextrose 5% through the needle (Fredrickson et al., 2009). This will help confirm that the needle tip is in the interscalene groove and also ease the advancement of the catheter into the interscalene space. The next part of the procedure is to maintain the needle position while inserting a catheter through the needle. If continuous ultrasound visualization is sought a second operator is needed to help pass the catheter. Once the catheter is inserted the catheter tip position is confirmed by visualizing an injection of a small amount of LA through the catheter. Following this confirmation the intended dose of LA is administered through the catheter. As these catheters are relatively superficial it is important to secure the catheter well to avoid accidental dislodgement. Catheters may be tunneled to decrease the risk of dislodgement. A drop of dermabond at the catheter insertion site can help reduce pericatheter leakage and help secure the catheter (Gurnaney et al., 2011). The catheter is secured using an adhesive skin preparation followed by a clear dressing to allow inspection of the catheter insertion site.
Post-operative care
The parents and child should be warned preoperatively about the potential for Horner’s syndrome with this block. In addition the risk of ipsilateral phrenic nerve block can lead to ventilatory compromise in children with a history of moderate to severe lung disease. A single injection block is expected to last 12–18 hours, and an analgesia plan should be in place for when the block resolves. The parents and child should be warned about the risk of temporary paresthesias and dysesthesias after an ISB as the risk is higher for the ISB (2–3%) compared to other brachial plexus blocks.
Continuous infusion for an interscalene catheter is initiated after the bolus intraoperatively or in the recovery room. Dilute bupivacaine, levobupivacaine or ropivacaine are used for the infusion. An infusion rate of 0.10–0.15 ml/kg with a maximum rate of 10 ml/h is recommended for the continuous infusion. Addition of adjuvants has not been beneficial for continuous nerve blocks.









