Substance Abuse and Addiction
Arnold J. Berry
Jerry S. Matsumura
CASE SUMMARY
A 36-year-old anesthesiologist was well liked by his anesthesiologist colleagues and was popular with patients. He arrived early to work and always seemed to be around the operating room in the evenings. He frequently signed up for extra call and requested to be assigned to cardiac and more complex cases.
A postanesthetic care unit (PACU) nurse mentioned that a few of his patients seemed to be having pain out of proportion to the amount of narcotics that were charted on the anesthesia record. Subsequently, the anesthesiologist was seen staggering in the operating room and was described as speaking very slowly. In accordance with departmental policy, a urine drug screen was obtained. The results of the urine drug screen were negative.
Later that month while on call, the anesthesiologist did not respond to his pager for an hour. When he did arrive to the operating room, he appeared sluggish. After discussion with the hospital’s Physician Health Committee and the practice group’s Management Committee, the anesthesiologist’s wasted narcotic syringes were analyzed. The results were consistent with dilution of narcotics with normal saline. The spouse was consulted, and she reported finding blood-tinged alcohol swabs and syringes around the house but stated that he always had reasonable explanations.
The Physicians’ Health Committee, based on the accumulated evidence, ordered the anesthesiologist to undergo a medical evaluation for addiction. He was then accompanied to a multidisciplinary, referral center specializing in health care professionals with addictive disease.
Subsequently, the anesthesiologist was diagnosed with an intravenous opioid addiction. He completed a 4-month treatment program and was counseled not to return to the practice of anesthesiology in the operating room for another 8 months. He received intensive outpatient treatment and monitoring. He registered with the state Physicians’ Diversion program and consented to a 5-year monitoring agreement, including naltrexone therapy. He was able to return to anesthesia practice a year later because of his success in accepting his disease, good family support, and compliance with his monitoring agreement.
What Baseline Knowledge Is Relevant?
This chapter addresses a complication that is very different from most of those in this text. Addiction is a disease that impacts us and is one of the only occupationally related complications that results in the deaths of several residents and anesthesiologists each year. In a practice consisting of 10 or more anesthesiologists, it is likely that one will become addicted at some point in their career. Although this chapter will provide the basic information on addiction among anesthesiologists and will discuss intervention and treatment, an expert in addiction medicine, with experience in treating physicians, should be consulted when a colleague shows signs of the disease.
▪ DEFINITION OF TERMS RELATING TO ADDICTION
In 1990, the American Society of Addiction Medicine (ASAM) formed a Committee on Nomenclature to define high-priority terms for use in scientific publications. The American Psychiatric Association decided on slightly different terminology in 1995, which was published in its Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV). For consistency, ASAM terminology will be used in this chapter.1
Addiction is “a primary, chronic, neurobiologic disease with genetic, psychosocial, and environmental factors that influence its development and manifestations.”1 It is characterized by behaviors that include one or more of the “4 C’s”: impaired control over drug use, compulsivity, continued use of drugs despite adverse consequences, and craving. (The DSM-IV equivalent is the term, substance dependence.)
According to the ASAM terminology, dependence is “used in three different ways, (a) physical dependence, a physiological state of adaptation to a specific psychoactive substance characterized by the emergence of a withdrawal syndrome during abstinence, which may be relieved in total or in part by readministration of the substance; (b) psychological dependence, a subjective sense of need for a specific psychoactive substance, either for its positive effects or to avoid negative effects associated with its abstinence; and (c) one category of psychoactive substance use disorder.”1 According to DSM-IV criteria, substance abuse represents a maladaptive pattern of regular use of a psychoactive drug. ASAM recognizes that “abuse” is part of diagnostic terminology, but because of lack of specificity and the pessimistic implication, it favors other terminology. Chemical dependency is a generic expression describing psychologic or physical dependency, or both, on one or more psychoactive substances.
According to the ASAM terminology, dependence is “used in three different ways, (a) physical dependence, a physiological state of adaptation to a specific psychoactive substance characterized by the emergence of a withdrawal syndrome during abstinence, which may be relieved in total or in part by readministration of the substance; (b) psychological dependence, a subjective sense of need for a specific psychoactive substance, either for its positive effects or to avoid negative effects associated with its abstinence; and (c) one category of psychoactive substance use disorder.”1 According to DSM-IV criteria, substance abuse represents a maladaptive pattern of regular use of a psychoactive drug. ASAM recognizes that “abuse” is part of diagnostic terminology, but because of lack of specificity and the pessimistic implication, it favors other terminology. Chemical dependency is a generic expression describing psychologic or physical dependency, or both, on one or more psychoactive substances.
Recovery is the process of overcoming both physical and psychologic dependence on a psychoactive substance with a commitment to sobriety. Addicts in recovery are referred to as recovering, rather than recovered, because addiction, like other chronic medical diseases, has no cure.1
What Are the Genetic, Neurophysiologic, and Biochemical Implications of Addiction as a Chronic Disease?
Although the concept of whether addiction should be classified as a disease has been debated, current research indicates that addiction has characteristics very similar to other diseases: it has distinguishing signs and symptoms; it is linked to genetic factors; it results in acute and chronic physiologic changes in the brain; it has behavioral and environmental components; and it has a progressive course that, if left untreated, results in disability and death. The model of addiction as a disease is important because it permits an understanding of the risk factors in susceptible individuals and an appreciation of the chronic changes that occur in neural pathways and signaling, all of which provide a rational basis for effective treatment strategies.
▪ GENETIC LINK
Studies in families have found a genetic link to chemical dependency.2 Early work documented that children of alcoholic parents were more likely to suffer from alcoholism. Although there are environmental factors that contribute to addiction, these studies demonstrated that in separated, adopted twins, the risk of alcoholism was more closely linked to drug dependence in the biologic parents than to drug use in the adoptive parents. Familial studies in siblings of addicts found an increased risk of cocaine abuse and other addictive drug use.
Molecular genetic research has identified specific genes that code for receptors and proteins in the endogenous opioid and monoaminergic systems in the brain.3 Changes in these receptors or in the characteristics or amount of the proteins they produce affect an individual’s response to addictive drugs. Addiction is associated with specific polymorphisms or variant genes responsible for the amounts and types of proteins and receptors in the regions of the brain affected by opiates and other addicting drugs.
▪ PATHWAYS AND MECHANISMS
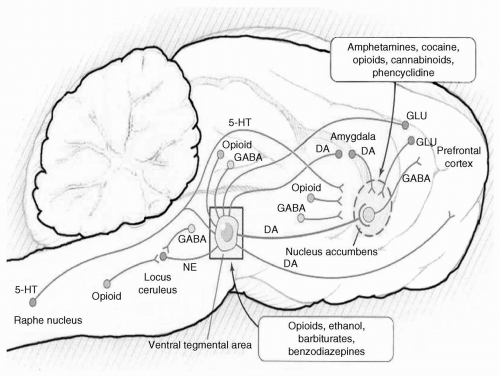
Highly addictive substances all produce their effects through a common neural pathway, the mesocorticolimbic system, which extends from the ventral tegmental area (VTA) of the midbrain to the nucleus accumbens (NAc), projecting to the limbic system, amygdala, and orbitofrontal cortex4 (see Fig. 69.1). This is the major central nervous system (CNS) pathway involved in processing reward, punishment, and reinforcement of the basic physiologic drives required for survival, that is, reproduction and eating. Components of the neural pathways contribute to the patterns of behavior. The amygdala assesses whether an experience is pleasurable; the limbic system saves the memories; and the frontal cortex synthesizes the information and executes the final action to take.
Although they work through specific receptors, all addictive drugs produce their effects through a common mechanism: increasing the neurotransmitter, dopamine, in the VTA and subsequently in the NAc.4 Opioids are agonists at the µ-receptors of the endogenous opiate pathways and produce increased dopamine in the VTA and NAc, whereas cocaine inhibits dopamine transporters, thereby increasing its concentration in the NAc. If the experience is pleasurable, the activation of these centers produces euphoria and reinforces the drive to repeat it. In contrast, declining levels of dopamine in the NAc prompts the addicted individual to seek drugs to prevent dysphoria and the unpleasant physical symptoms of withdrawal that are produced by noradrenergic outpouring from the neurons in the locus ceruleus.
Acute opioid administration activates µ-opioid receptors, inhibiting adenyl cyclase and reducing cyclic adenosine monophosphate (cAMP) levels. Continued use and chronic activation of µ-receptors has the opposite effect of upregulating cAMP-signaling pathways but also increases the phosphorylation of gene transcription factors, cAMP-responsive, element-binding protein (CREB), and ΔFosB. Tolerance, defined as an increase in the dose and the frequency of drug administration required to achieve the desired effects, is associated with decreases in the number and responsiveness of opioid receptors produced by CREB. Animal models have demonstrated remodeling of neurons in the NAc after chronic drug administration,
possibly related to increased levels of ΔFosB. Positron emission tomography brain scans in addicts confirm increased neuronal activity in the NAc and demonstrate changes consistent with animal models. Alterations in the CNS generated by substance use may persist for years after abstinence from highly addictive drugs. Treatment for chemical dependency must, therefore, continue well beyond the acute recovery phase to prevent relapse from the sensitization and craving that persists because of CNS remodeling. It is hoped that, as we gain more knowledge of the CNS, we will be able to treat addiction more effectively with specific therapies that target the neural pathways and receptors affected by the disease.
possibly related to increased levels of ΔFosB. Positron emission tomography brain scans in addicts confirm increased neuronal activity in the NAc and demonstrate changes consistent with animal models. Alterations in the CNS generated by substance use may persist for years after abstinence from highly addictive drugs. Treatment for chemical dependency must, therefore, continue well beyond the acute recovery phase to prevent relapse from the sensitization and craving that persists because of CNS remodeling. It is hoped that, as we gain more knowledge of the CNS, we will be able to treat addiction more effectively with specific therapies that target the neural pathways and receptors affected by the disease.
▪ ENVIRONMENTAL AND BEHAVIORAL FACTORS
Environmental and behavioral factors also play a role in addiction. Anesthesiology is one of the only medical specialties in which physicians administer medications directly to patients, and therefore narcotics and other addicting drugs are readily accessible. Diversion of these drugs for self-administration can quickly lead to addiction in individuals with a genetic predisposition. Euphoria and the pleasurable experience resulting from the initial use become linked to the setting where it occurred and the situation in which it took place.5 These powerful associations produce cravings for drugs when the addicted individual encounters or even thinks about them again. Consideration of both the environmental and behavioral factors must form part of treatment.
Because anesthesiologists are familiar with the immediate effects of medications they administer to patients, some may experiment with drugs to treat their own problems, such as stress resulting from financial difficulties, poor patient outcome, potential litigation, perceived professional inadequacy, or sleep deprivation. Some physicians have poor coping skills, characterized by feelings of isolation and have difficulty asking for help. Children of alcoholics or addicts, or individuals, who were abused or neglected during childhood, are at increased risk for substance abuse.
Although there have been reports of anesthesiologists being addicted to all classes of psychoactive substances (including propofol and volatile anesthetic agents), fentanyl and sufentanil are the most commonly abused, parenterally administered drugs. These opioids are easy to obtain and titrate while working in the operating room, quickly produce euphoria of a short duration, and are difficult to detect on routine blood or urine screening
tests. Polydrug use is common, and alcohol is often used in combination with another substance.
tests. Polydrug use is common, and alcohol is often used in combination with another substance.
The addictive potential of fentanyl and sufentanil is extremely high, with addiction and tolerance occurring after only a few doses. This is in contrast to low-potency opiates (such as hydrocodone) or alcohol, which may require many years before the problems of addiction become apparent and are expressed.
How Common Is Addiction in Anesthesiologists, and Is the Disease More Prevalent than in Other Medical Specialties?
▪ INCIDENCE AND PREVALENCE
Studies to determine the incidence or prevalence of addiction in anesthesiologists are extremely difficult to conduct, and therefore published data usually reflect incomplete estimates. Early information from Talbott’s program for impaired physicians suggested that anesthesiologists were overrepresented.6 Of the first 1,000 physicians in treatment, 12.1% were anesthesiologists, but anesthesiologists comprised only 3.9% of all physicians practicing in the United States. In Talbott’s data, it is rarely noted that the greatest proportion of physicians in his treatment program were not anesthesiologists, but were in general or family practice. These specialties comprised 25.7% of physicians in his treatment, although only 12.4% of physicians in the United States were general or family practitioners.
Although these early studies have given the impression that anesthesiologists have a higher risk for addiction than physicians in other medical specialties, more recent studies suggest that this may not be the case. In McGovern’s findings, anesthesiologists represented 4.6% of 108 physicians being evaluated for substance use disorders, a rate that is not greater than the national prevalence.7 A 1992 survey demonstrated that psychiatry and emergency medicine residents had a greater rate of substance use than residents in nine other specialties,8 and the rate for anesthesiology residents was not greater than that of other specialties.
Several investigators have used questionnaires to collect data on rates of chemical dependency among individuals in anesthesia residency programs. A survey of 133 anesthesiology training programs in the United States, conducted in 1998 demonstrated an incidence of controlled substance abuse of 1% among faculty members and 1.6% among residents.9 These rates are similar to those found in several earlier studies of anesthesiology residents. Although academic departments have implemented strategies such as educational programs, satellite pharmacies, and pharmacy accounting procedures, the survey from Booth et al. suggest that the risk has not decreased.9
How Can Addiction Be Detected in the Anesthesia Provider?
Although the only concrete sign of addiction in an anesthesia provider is an actual witness to the self-administration of drugs, there have been many descriptions of the signs and symptoms of addiction in anesthesia personnel. (See Tables 69.1 and 69.2). Unfortunately, the signs and symptoms are relatively nonspecific and require a certain degree of suspicion and experience to identify, and hence do not facilitate the screening of those prone to develop addiction. Moreover, the signs and symptoms may not be obvious until the later stages of the disease when performance at work, the last place the disease expresses itself, is affected.
There are currently no effective means of preventing the disease from developing, and therefore, the goal must be early identification to reduce losses (to life, family, health, license, career) due to the disease. The keys to early identification are awareness and acceptance that addiction is a medical disease, and that the addicted individual is not weak-willed, immoral, or lacks intelligence. Specific strategies intended to reduce mortality from addiction strive for earlier identification through various measures: (i) Educational programs to provide information for anesthesia professionals, their significant others, and operating room personnel; (ii) implementation of pharmacy policies to prevent drug diversion (strict accounting of controlled substances, tracking narcotic utilization, and random testing of returned syringes and narcotic wastage); (iii) institution of policies that permit drug screening for cause10; (iv) providing a therapeutic approach to those that selfrefer; and (v) developing strategies to promote healthy lifestyles (healthy approaches to stress reduction and work schedules that allow adequate sleep). The Accreditation Council for Graduate Medical Education already requires that anesthesiology training programs include education on substance abuse and addiction.
Addiction to alcohol, drugs, and anesthetic agents can occur in anyone. Addiction to medications used in the practice of anesthesiology can occur in all categories of anesthesia professionals including anesthesiologists, residents, certified registered nurse anesthetists, anesthesiologist assistants, and student anesthetists. Medical students and other categories of operating room personnel also risk addiction to medications used in anesthesiology.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree