A selection of ultrasound machines used for regional anesthesia.
A variety of needles, stimulating and non-stimulating, and echogenic needles that are coated or scored are available for use (Figure 2.2). In centers where only ultrasound guidance is used, stimulating needles are not necessary. However, many practitioners still use a combination of nerve stimulation and ultrasound guidance. There also are echogenic catheters available for placement. At this moment there is no clear evidence to show the benefit of echogenic needles and catheters. A variety of nerve stimulators are available if one uses a concurrent nerve stimulation technique.
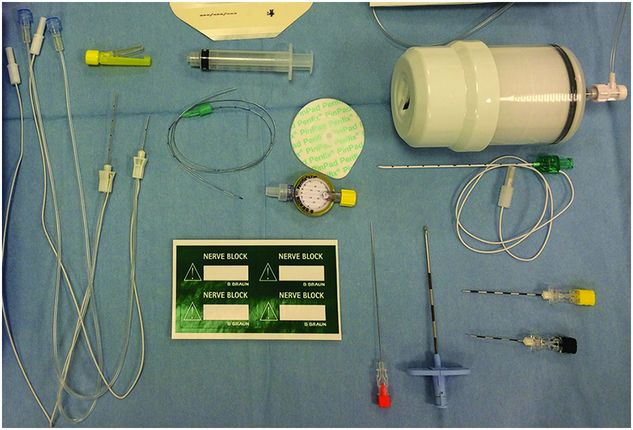
A variety of needles can be used for ultrasound-guided regional anesthesia. A nerve stimulator can be used concurrently with many block needles if required. A catheter should be labeled with a suitable label, e.g. “nerve block,” and can be connected with an elastomeric pump such as the one shown. Needles shown from left to right are: 50 mm and 25 mm 21-gauge stimulating needles; 27-gauge spinal pencil point needle (orange); 18-gauge Touhy-type needle (blue); 20-gauge Touhy-type catheter through needle (green); and pediatric caudal needles – 20-gauge (yellow) and 22-gauge (black).
Long-sleeve probe covers are recommended when perineural catheters are placed. For single injection blocks one can just seal the probe tips with sterile adhesives (Figure 2.3).
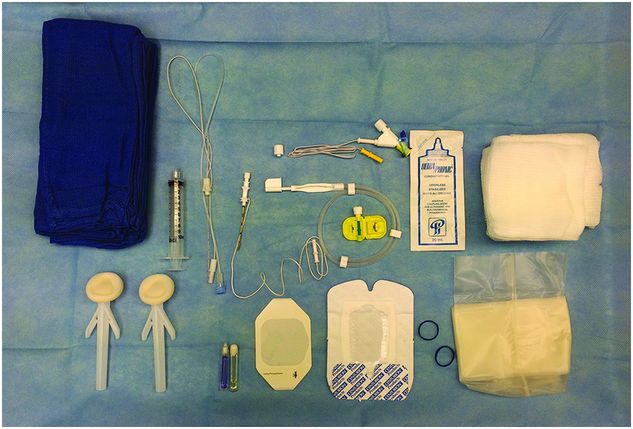
Sterile set-up for an ultrasound-guided peripheral nerve block with catheter placement – includes sterile skin disinfectant, drape, sterile gel and probe cover, and catheter skin adhesive and clear dressing.
Block set up
All patients should have the standard monitors that include pulse oximetry, electrocardiogram (ECG), and blood pressure in addition to a functioning intravenous (IV) line prior to the placement of a block. As most regional anesthetic procedures in children are performed under general anesthesia, one should remember to avoid neuromuscular blockade if nerve stimulation is to be used for performance of the block. The ability to use neuromuscular blockade is an advantage when performing blocks with ultrasound guidance only. Also, when performing the blocks under general anesthesia, there should be assistance available to monitor the patient. The second person may also help with optimizing the ultrasound image, operating the nerve stimulator when used, and injection of the LA. It is also important to pay attention to ergonomics, like raising the table to the desired height and lining up the ultrasound machine, the needle direction, and the line of vision to obtain best results.
Drugs needed for resuscitation, such as epinephrine and Intralipid®, should be readily available to address LAST if it occurs. When blocks are performed in awake/sedated patients, equipment for airway support should be available along with benzodiazepines to treat seizures.
Asepsis
Recent guidelines on the prevention of regional anesthesia-related infection have recommended the use of chlorhexidine in alcohol solutions for all blocks including neuraxial (ASRA 2006; ASA 2010; AAGBI 2014). However, there is ongoing controversy in this area, which is beyond the scope of this chapter. In summary, skin preparation for peripheral nerve blocks can be done using either iodine or chlorhexidine solutions mixed with alcohol. In the case of neuraxial blocks, concerns that chlorhexidine is a neural toxic and that it has been implicated in cases of chemical arachnoiditis in adults have resulted in vigorous debate regarding its use for neuraxial blocks. The most recently published national guidelines (UK and Ireland) recommend chlorhexidine in 70% isopropyl alcohol but at a reduced concentration of 0.5%.
When perineural catheters are placed it is advisable to drape the field just like for a surgical procedure (Figure 2.3). The incidence of infection following placement of perineural catheters in children is less than 1% (Ganesh et al., 2007; Polaner et al., 2012; Gurnaney et al., 2014) and for neuraxial blockade, about 1.1% (Polaner et al., 2012) and less than 1% (Llewellyn and Moriarty, 2007). In most studies there was a clear correlation between the duration of the indwelling catheter and the risk of infection. The incidence of serious infective complications like epidural abscess and meningitis was very low.
Safety and complications
The safety of regional anesthesia in children has been well established (Giaufre et al., 1996; Krane et al., 1998; Llewellyn and Moriarty, 2007; Polaner et al., 2012; Krane and Polaner, 2014; Taenzer et al., 2014b). The incidence of neurologic complications is extremely low and infective complications are mostly confined to local skin infections. There were no cases of deep-seated abscesses in the PRAN study (Polaner et al., 2012) and only 2 cases (out of 10 633 epidurals) in the Pediatric Epidural Audit (Llewellyn and Moriarty, 2007).
A prospective study of 1010 ultrasound-guided blocks found neurologic symptoms in 8.2% of patients after 10 days, 3.7% after 1 month, and 0.6% after 6 months (Fredrickson and Kilfoyle, 2009), which is similar to the overall incidence of complications following peripheral nerve blocks (Auroy et al., 2002). Chapter 4 deals with complications in greater detail. There are no large pediatric studies to evaluate the safety of ultrasound-guided regional anesthesia in children. The incidence of adverse events following peripheral nerve blockade is so low that it is going to be very difficult to demonstrate a superior safety profile with the use of ultrasound guidance. However, the improved success rate and the requirement for lower volumes with the use of ultrasound guidance should result in the increasing use of ultrasound for peripheral nerve blockade.
Interestingly, there has been renewed interest in regional anesthesia as the sole anesthetic technique in children. The effects of general anesthesia drugs on neurodevelopment, particularly on behavioral and cognitive function, has recently added to this debate (Lei et al. 2014). Spinal anesthesia previously performed in neonates or for children at increased risk of apnea, can be safely and effectively performed in older children as well. A pediatric series of 1132 spinal anesthetics for lower abdominal and orthopedic surgeries, in children aged 6 months to 14 years, has been published without a major complication (Puncuh et al. 2004).
Contraindications to regional anesthesia
Contraindications to regional anesthesia in children are very similar to those in adults. Parent or patient refusal, infection at the site, and LA allergy are absolute contraindications. Coagulopathy due to disorders of coagulation, use of anticoagulants, and systemic disorders like overt sepsis are usually absolute contraindications for neuraxial blockade. However, peripheral nerve blockade may be performed with caution in some of these patients (Sripada et al., 2009), but they should be closely monitored for complications with early intervention when indicated (Rodriguez et al., 2011). Imaging with ultrasound prior to neuraxial procedures in infants, particularly those with atypical dimples that are large (>5 mm), high on the back (>2.5 cm from the anus), or appear in combination with other lesions (that include hemangiomas, hairy patches, etc.), may help detect cases of spinal dysraphism and thereby prevent catastrophic consequences (Kriss and Desai, 1998). Relative contraindications include progressive neurologic diseases and the presence of ventriculo-peritoneal shunts (Ecoffey, 2012).
Post-operative care
Whenever feasible all patients who have had a regional anesthetic procedure performed in the operating room need to be evaluated in the recovery room to evaluate the efficacy of the block. This is important as most regional anesthetic techniques in children are performed under general anesthesia and success of the block can only be truly determined in the post-operative period. Supplement analgesia should be ordered for those who have insufficient coverage from the block or when the block is a failure. Pain assessment should be carried out in the recovery room and at least every 4 hours thereafter. Clear instructions need to be given to protect the insensate areas resulting from the block. If there is a possibility of motor blockade, particularly in the lower extremities, adequate weight-bearing instructions need to be provided. In case of continuous peripheral nerve and neuraxial blockade, the catheter site needs to be evaluated at least once a day to look for signs of infection/dislodgement.
When patients are discharged home with indwelling perineural catheters, verbal and written education should be provided about the continuous infusion device system, techniques to remove the catheter, recognition of potential complications (symptoms of LA systemic toxicity), catheter dislodgement, and inadequate pain control. Families should also receive emergency contact information for the pain service. Patients should be cautioned to avoid weight bearing on the extremities that are weak and also to protect insensate areas from injury (e.g. from heat, cold, pressure, and other trauma) (Ganesh et al., 2007; Gurnaney et al., 2014).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








