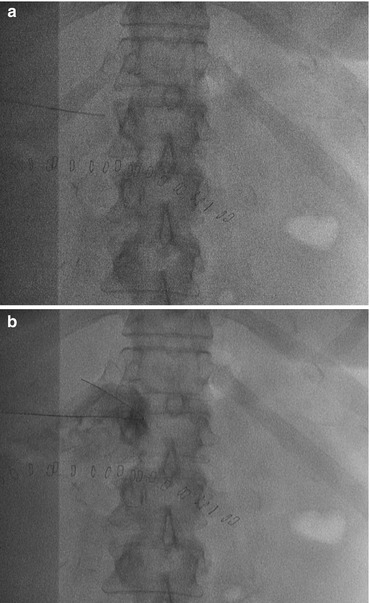
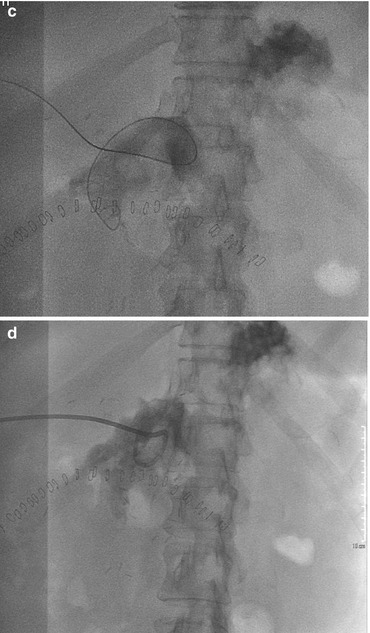
Fig. 21.1
Post-duodenocefalopancreasectomy collection
21.3 Percutaneous Treatment
The first studies on the percutaneous abscess drainage have been published around 30 years ago as an alternative to the more invasive surgical treatments [3–5] and have since then become the standard of care.
The drainage of abdominal fluid collection can be performed with a diagnostic or therapeutic purpose.
Diagnostic
Characterization of the abdominal fluid collection (pus, bile, blood, urine, lymph, pancreatic juice)
Differentiate infected from noninfected collections and characterization of the responsible microorganism
Therapeutic
To treat abscesses that can be fully drained
Adjuvant measure in the cases of multiple incompletely drainable abscesses or in critical patients
21.4 Indications
The main indications of the percutaneous drain placement are the presence of an abdominal infected collection. The abscess size is usually bigger than 4 cm. For the management of smaller (<3 cm) collections, most authors advocate a trial of antibiotics alone with consideration given to needle aspiration to hone antibiotic coverage for persistent cases [6, 7].
Symptoms such as pain or pressure from a large noninfected fluid collection, or obstruction of the bowel or ureter, are also indications for drainage.
The only absolute contraindications to perform a percutaneous drainage are the lack of a safe access or when the access can be impaired by the interposition of organs of vascular structures.
However, in most cases the absence of a safe way to reach the collection can be resolved by changing decubitus or by using curved needles or choosing alternative approaches: transgluteal (Fig. 21.2), transvaginal, or transperineal paths are used for pelvic collections and transhepatic to reach the epiploon and peripancreatic cavities.
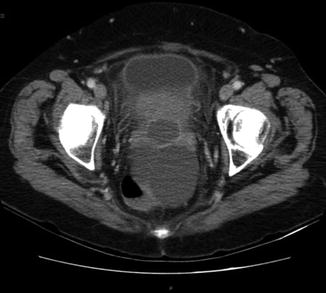
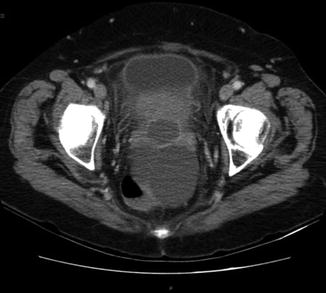
Fig. 21.2
A 69-year-old woman with diverticolitis and pelvic collection. After endovenous mdc subministration, it is possible to clearly differentiate the collection from the free fluid in the Douglas pouch
If the way of access is covered by a small bowel loop or the stomach, the drainage can be done relatively safely through those organs via a needle. However, it is not recommended to pass a needle through the colon.
Coagulopathy, transpleurical pass, echinococcal cyst, and asymptomatic sterile fluid collections are relative contraindication.
The presence of coagulation disorders have to be corrected before the procedure by the administration of fresh frozen plasma or platelets.
Transpleural passage should be avoided as much as possible because it is painful and can cause a pleuric effusion or a secondary infection of the pleural space.
The drainage of echinococcal cysts is not therapeutic and can be complicated by anaphylactic shock and spreading of the disease. Percutaneous treatment of such cysts can be, however, achieved using the so-called PAIR technique (puncture, aspiration, alcohol injection, re-aspiration) [8] with low rate of recurrence and complications.
The drainage of an asymptomatic sterile fluid collection is not recommended, and if it is done, the catheter should be left in place for the shortest possible time, to avoid possible secondary infections.
21.5 Imaging Guidance
Ultrasound and CT are the modalities used most of the times to guide the drainage procedures. Fluoroscopy is sometimes needed in addition to the sonography to monitor the drainage and the eventual presence of fistulas by iodinated contrast injection.
Ultrasound is the most useful way to visualize intra-abdominal abscesses. The main advantages of this technique are:
The possibility to follow the needle pathway in real time, thus allowing the rapid execution of the drainage
The possibility to perform this technique in the same patient’s room (e.g., in cases of patients in intensive care unit)
The easy availability of the equipment
Limitations of ultrasound are deep-located collections (retroperitoneum, pelvis, peripancreatic region) or when there is an overlapping structure (e.g., a bowel loop) impairing the ultrasounds guide.
CT is the preferred choice when a reasonably safe pathway cannot be found using ultrasonography. The main advantage of CT is the perfect visualization of all the anatomic structures and thus the possibility to track particularly difficult and/or deep paths. Another benefit of CT is that, through the administration of EV contrast media, it is possible to further improve the visualization of the fluid collection (Figs. 21.2 and 21.3).


Fig. 21.3
MIP oblique reconstruction of the control scan after positioning of drainage catheter in the collection: 30 ml of pus were aspired. During the multistep procedure of the needle insertion, a sample of the free fluid in the Douglas space was aspirated and cultured and it resulted negative for infection
The drawbacks of CT are the length of the procedure, the limited access to the equipment, the lack of real-time needle visualization during the procedure, the difficulty in following nonorthogonal paths, and the exposition to x-rays.
21.6 Patient Preparation
Coagulative tests: PT < 15 s; INR < 1,5; platelet > 75,000
Test of the kidneys functionality if an intravenous contrast is foreseen.
Fasting
Venous access
Informed consent
Monitoring
21.7 Punction Technique and Other Technical Issues
The first common steps of the procedure are the study of the preliminary imaging to determine the optimal approach, the disinfection and preparation of the skin, a sterile work field large enough to place the guides and catheter and an adequate local anesthesia.
Seldinger Technique
Choose the material. Chiba needles are preferable, having a good echogenicity and being relatively atraumatic.
Position the needle in the collection (Fig. 21.4a). This phase can be done in one step if US-guided, or in more steps when using CT guidance. Using US we have a real time vision of the needle path while with CT, after each step, it will be necessary to monitor the correct needle direction through repeated scans limited to the specific area of interest.