Fig. 73.1
Surface anatomy for lumbar plexus block
The needle is inserted perpendicularly to the skin and advanced slowly until twitches of the quadriceps muscle are observed. The initial current is set at 1–2 mA (2 Hz) and then gradually reduced. Local anesthetic is injected after negative aspiration when the threshold current of 0.5 mA is reached. The skin-to-plexus distance correlates with weight for children aged 3–12 years old and ranging from 1.24 to 1.74 mm/kg [2].
Ultrasound-Guided Technique
A 13-6 MHz linear “hockey stick” probe is commonly used for infants and young children. A lower-frequency (5-2 MHz) curved array probe is required for deeper penetration in older children. The probe is placed longitudinally just lateral to the midline to identify the sacrum. Scan proximally to locate the L5 transverse process and the L4/L5 interspace. From there, the probe is rotated 90° to obtain a transverse view of the spinous process, the erector spinae muscle (superficial and lateral to the spinous process), and the quadratus lumborum muscle (lateral and deep to the erector spinae muscle) (Fig. 73.2). The psoas muscle, which appears slightly hypoechoic with multiple hyperechogenic striations within (i.e., a “starry night” appearance), is located deep to the quadratus lumborum muscle, and the plexus can be found in the muscle belly of the psoas. The nerves often appear as hypoechoic “dots” surrounded by hyperechoic connective tissue. Note that the lower pole of the kidney is usually found at L2/L3 level in adolescents and can reach as low as L4/L5 in young children.
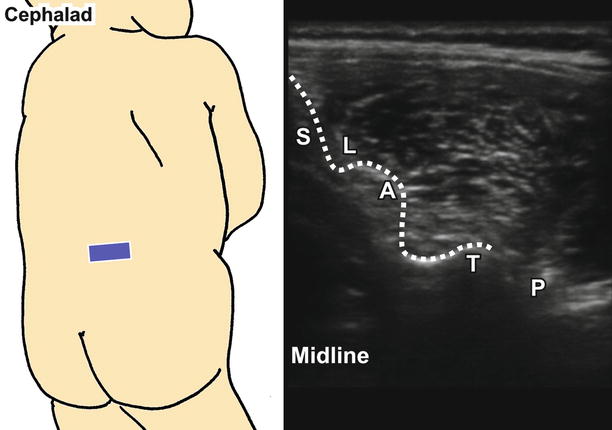
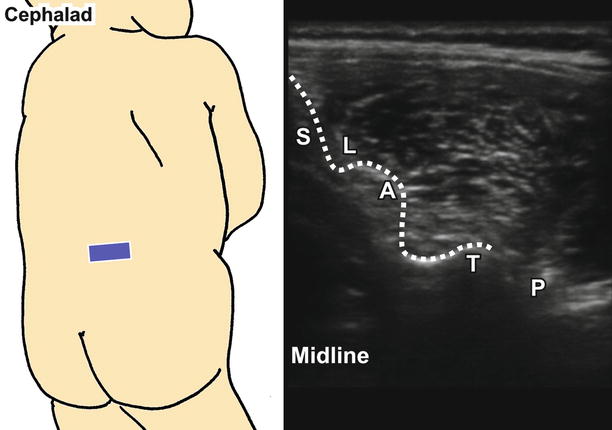
Fig. 73.2
Ultrasound image of major anatomical structures in the lumbar plexus. S spinous process, L lamina, A articular process, T transverse process, P psoas muscle
If the probe is placed longitudinally to view the transverse processes of L3/L4/L5, the psoas muscle can be seen through the acoustic window between the transverse processes, deep to the erector spinae muscle. The plexus lies within the posterior third of the psoas.
The transverse processes and the plexus may be difficult to visualize in older children because of the greater depth and poorer differentiation between muscles and nerves. It may be necessary to switch between transverse and longitudinal scanning to survey the area. Occasionally, the more superficial L3/L4 interspace can be used for better resolution.
Both in-plane and out-of-plane approaches can be used. When using the in-plane approach, the probe is placed longitudinally. The needle is inserted from the inferior end of the probe and directed cephalad to reach the psoas muscle between the L4 and L5 transverse processes. For the out-of-plane approach, the probe is placed in a transverse plane at L4/L5 interspace. The needle is introduced at 45–60° to the skin, 1 cm from the caudad end of the probe. Walk the needle down to reach the plexus while keeping the needle tip in view. Confirm the plexus using nerve stimulation.
For the “offline” technique, the lateral edges of the L4 and L5 transverse processes are marked, and the depth to transverse process is noted during the pre-procedural scan. The needle is inserted perpendicularly to the skin to a depth approximately 1 cm beyond the recorded depth of the transverse process. Locate the plexus using nerve stimulation.
In all cases, avoid directing the needle medially, which may result in unintentional epidural/intrathecal injection. Local anesthetic is injected after negative aspiration. A “flow-like” pattern within the psoas compartment may be seen.
Paravertebral Block
Introduction, Indications, and Complications
The paravertebral space is a wedge-shaped region on either side of the vertebral column which contains the spinal nerves as they exit the intervertebral foramina. In the thoracic region, the paravertebral space is bounded medially by the vertebral body, intervertebral disc and foramen, and spinous processes; anterolaterally by the parietal pleura; and posteriorly by the anterior surface of the transverse process and superior costotransverse ligament. In the lumbar region, the space is bounded anteriorly by the psoas muscle. The paravertebral space communicates medially with the epidural space and, in the thoracic region, laterally with the intercostal space. By depositing local anesthetic into the paravertebral space, the spinal nerves on the operative side can be anesthetized, producing ipsilateral somatic and sympathetic blockade similar to a “unilateral epidural,” although true epidural spread is possible due to the extension of the dural cuff. In addition to single-injection blocks, catheters can be placed to provide analgesia by continuous infusion.
This block is indicated for unilateral surgical procedures. For thoracic paravertebral block, it is commonly performed for breast and renal surgery, thoracotomy, and pain management for rib fractures, whereas lumbar paravertebral block is used in lower limb surgeries. It is an advanced block with potential serious complications, including total spinal anesthesia and, in the case of thoracic blocks, pneumothorax. The use of ultrasound has the advantages of improving the accuracy of needle placement and visualizing spread, while at the same time minimizing inadvertent puncture of the pleura or neuraxial structures.
Patient Positioning, Preparation, Equipment, and Dosage
Under general anesthesia or heavy sedation to avoid any movement, the child lies in the prone or lateral decubitus position with the back assuming a kyphotic posture. The skin is cleaned with antiseptic solution. Prepare the probe surface by applying a sterile adhesive dressing if the ultrasound approach is used.
A 22-G, 50-mm insulated needle is commonly used. Alternatively, an epidural set with an 18–22 G Tuohy needle can be used if seeking loss of resistance. Choices of local anesthetic include 0.125–0.25 % bupivacaine. A volume of 0.5 mL/kg with or without epinephrine (without exceeding the toxic dose) is required to cover a vertical spread of 4–5 vertebral levels. A smaller volume of 0.1 mL/kg should be used if blocks are performed individually at each level.
Landmark Technique
Palpate for the spinous processes in the midline. Locate the bony landmarks: T7 vertebra at the tip of the scapula, C7 vertebra with the most prominent spinous process, L4 vertebra on the intercristal line (L5/S1 for neonates), and S1 on the line between two PSIS (Fig. 73.3). Mark the spinous processes on the skin. Next, locate and mark the transverse processes which are 1–2.5 cm lateral to the spinous processes, depending on the child’s age (see equation below). In the thoracic region, the transverse processes are generally located at one intervertebral space higher than the corresponding spinous process because of the inferior angulation of the spinous processes. In the lumbar region, the transverse processes are located lateral to the corresponding spinous process.
Fig. 73.3
Surface anatomy for thoracic paravertebral block
The needle is inserted perpendicularly to the skin to contact the transverse process. The depth of the transverse process is noted. Redirect the needle 10° superiorly or inferiorly to walk off the transverse process and advance slightly deeper (to a maximum of 1 cm). Angle the needle slightly medially to minimize risk of puncturing the lung (excessive medial angulation may result in intraforaminal injection and should be avoided). A “give,” indicating a loss of resistance, is felt as the needle punctures the costotransverse ligament. When using the epidural set, loss of resistance to air or D5W can be elicited. The depth of the paravertebral space has been found to correlate with the patient’s body weight. Formulae determining the distance of the thoracic paravertebral space from the skin and the spinous process have been developed [3]:
Depth to epidural space (mm) = 0.48 × body weight (kg) + 18.7
Distance from midline (spinous process) (mm) = 0.12 × body weight (kg) + 10.2
The lumbar paravertebral block is technically similar to the thoracic paravertebral block. However, injection at each level is recommended for effective coverage since the vertical spread of local anesthetic is limited at the lumbar level.
Nerve Stimulation Technique
Nerve stimulation for paravertebral block has been reported but is not commonly used for nerve localization. If nerve stimulation is used, a current of 1.5–3 mA is applied after the needle is introduced. Advance the needle slowly until appropriate motor responses (twitches in the ipsilateral thoracic/abdominal wall for thoracic paravertebral block or twitches in the ipsilateral quadriceps muscle for lumbar paravertebral block) are observed. The current is then decreased gradually, and local anesthetic is injected when a threshold current of 0.4–0.6 mA is reached. Bilateral motor responses indicate possible intrathecal/subdural placement or epidural placement when higher-threshold currents are reached.
Ultrasound-Guided Technique
A high-frequency (13-6 MHz) linear probe is used. Both “offline” and real-time scanning can be used. The “offline” approach involves performing a pre-procedural scan to locate the point of needle insertion, depth of the paravertebral space, and needle trajectory prior to needling. The real-time approach involves performing needle insertion under real-time ultrasound guidance and is more commonly used nowadays. Similar to adults, the visibility of the paravertebral space is limited in children older than 3 years old because of the small acoustic window that results from ossification of bony elements.
The probe is placed in the transverse plane in the midline to identify the spinous process and laminae with hyperechoic outline and acoustic shadowing (Fig. 73.4 for thoracic; Fig. 73.2 for lumbar). Locate the transverse process laterally. The lateral distance and depth of the transverse process are noted. Rotate the probe to the midline longitudinal plane to again look for the spinous processes. Scan laterally to identify the lamina, articular processes, and transverse processes (and ribs in the thoracic region) from medial to lateral. For thoracic region, the transverse processes appear as short rectangular structures with hyperechoic outlines and acoustic shadowing, as compared to the overlapping lines for lamina and “lumps” for articular processes (Fig. 73.5). The ribs often have a roundish outline instead of rectangular. The pleura appears as a hyperechoic line under the ribs. In the thoracic region, the paravertebral space can be found deep to the transverse processes between the intercostal muscle and parietal pleura. In the lumbar region, the lumbar plexus lies in the “psoas compartment” between the psoas major and quadratus lumborum muscles. The depth to parietal pleura (for thoracic paravertebral) or psoas major (for lumbar paravertebral) is noted.
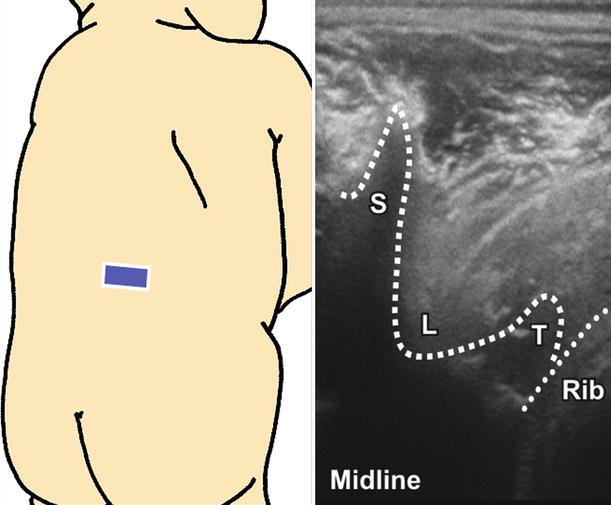
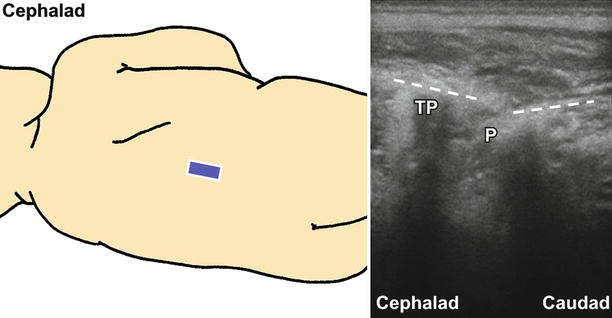
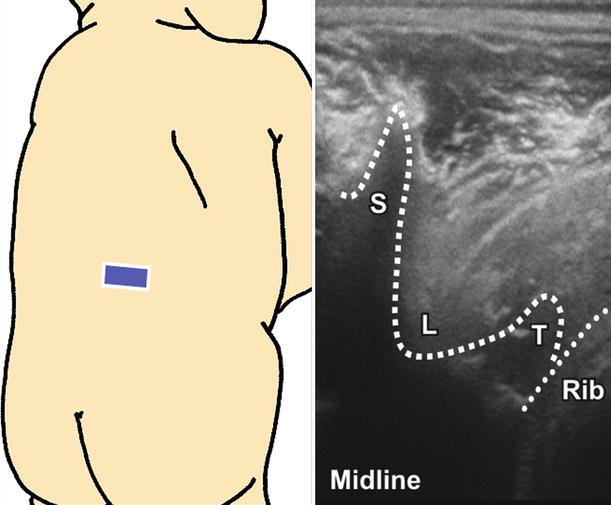
Fig. 73.4
Ultrasound image of transverse view at T9–T10. S spinous process, L lamina, T transverse process
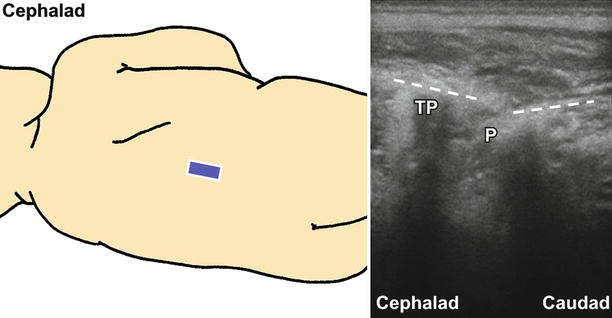
Fig. 73.5
Ultrasound image of midline longitudinal view at T9–T10. TP transverse process, P paravertebral space
Both in-plane and out-of-plane approaches can be used for blocks under real-time ultrasound guidance. If possible, the probe should be placed in the longitudinal plane when using the in-plane approach and the transverse plane when using the out-of-plane approach to avoid excessive medial angulation of the needle. Local anesthetic is deposited into the paravertebral space after negative aspiration for blood or air. For thoracic paravertebral blocks, the pleura will appear to be pushed down by the hypoechoic local anesthetic. For lumbar paravertebral block, the injectate is seen posterior to the psoas. Vertical spread (especially thoracic paravertebral block) to other levels can be seen.
Intercostal Block
Introduction, Indications, and Complications
After emerging from the intervertebral foramina, the thoracic spinal nerves divide into dorsal and ventral rami. The former supply the paravertebral region, while the latter give rise to intercostal nerves. There are 11 pairs of intercostal nerves (T1–T11) and one pair of subcostal nerves (T12). An intercostal nerve runs initially between the parietal pleura and the intercostal membrane and then passes through the membrane near the angle of the rib, travelling between the innermost and internal intercostal muscles. The nerve gives rise to the lateral cutaneous branch (which innervates the lateral trunk) near the midaxillary line and terminates as the anterior cutaneous branch (which innervates the anterior trunk) anteriorly. Within the intercostal space, the nerve travels in the costal groove underneath the intercostal vein and artery.
This block is used in pain management for rib fractures, thoracotomies, hepatobiliary and gastric surgery, and minor procedures such as chest tube insertion. Systemic toxicity is a potential risk, especially if multiple blocks are performed, since systemic absorption can be significant in the intercostal region. Pneumothorax is another possible complication.
Patient Positioning, Preparation, Equipment, and Dosage
The child lies in a lateral decubitus position. The prone position is preferred for bilateral block. The arms are extended forward so that the scapulae move laterally away from midline. The skin is cleaned with antiseptic solution. Prepare the probe surface by applying a sterile adhesive dressing if an ultrasound approach is used.
A 50-mm, 22–24-G short-beveled needle can be used. Extension tubing is attached to the needle to minimize movement of the needle upon respiration. Choices of local anesthetic include 0.25–1 % lidocaine and 0.125–0.25 % bupivacaine, depending on the required duration of action. A volume of 0.5–1 mL of local anesthetic is usually adequate for each level. More diluted solution should be used for small children to avoid overdose. Epinephrine 1:400,000 (with a maximum dose of 4 μg/kg) can be added to decrease systemic absorption.
Landmark Technique
Similar to paravertebral block, nerve stimulation is not commonly used for nerve localization. Depending on the location of the incision (or area of injury for fracture ribs), determine the level of the block. Multiple blocks at consecutive levels are usually needed for effective analgesia.
The midaxillary line runs longitudinally from the axilla. The posterior axillary line runs midway between the midaxillary line and the spinous processes. The lower border of the rib marks the needle insertion site for the nerve of the same level. The point of needle insertion is at the inferior border of the rib at the posterior axillary line (Fig. 73.6). With the fingers of one hand retracting the skin up and over the rib, the needle is inserted at a 20° cephalad angle with the bevel facing cephalad. Advance the needle slowly until it contacts the bone. Withdraw the needle slightly and walk off the inferior border of the rib. Apply a constant pressure to the syringe. A sudden loss of resistance can be felt when the needle enters the intercostal space. Local anesthetic is injected after negative aspiration for blood and air.
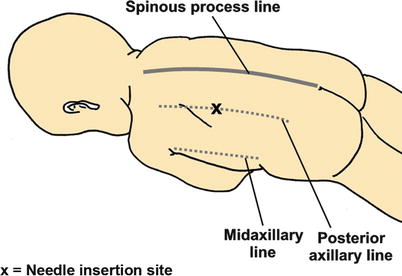
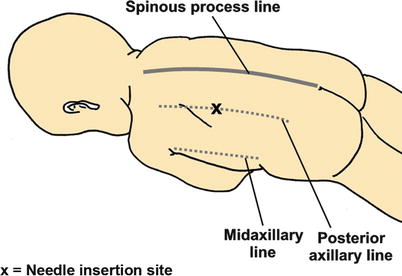
Fig. 73.6
Surface anatomy for intercostal nerve block (posterior approach)
Nerve Stimulation Technique
Not commonly used for this block.
Ultrasound-Guided Technique
A high-frequency (13-6 MHz) linear probe is used. The probe is placed along the mid- or posterior axillary line to obtain a cross-sectional view of two ribs with the intercostal muscle layers and pleura in between (Fig. 73.7). The ribs have a hyperechoic outline with acoustic shadowing, while the pleura is distinguished by its sliding movement with respiration and the hypoechoic pleural cavity underneath. The intercostal vessels, which are situated between internal and innermost intercostal muscles, can be identified on color Doppler. The intercostal nerve is found next to the vessels.
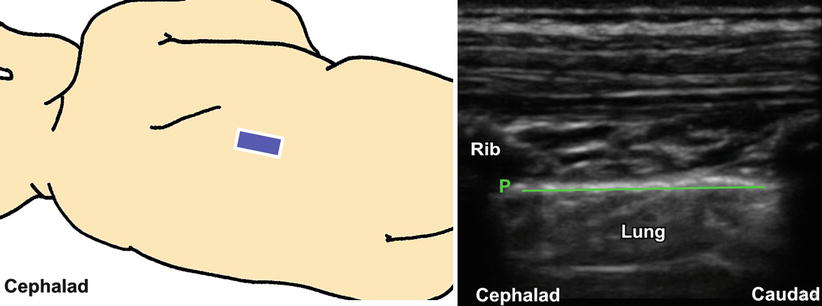
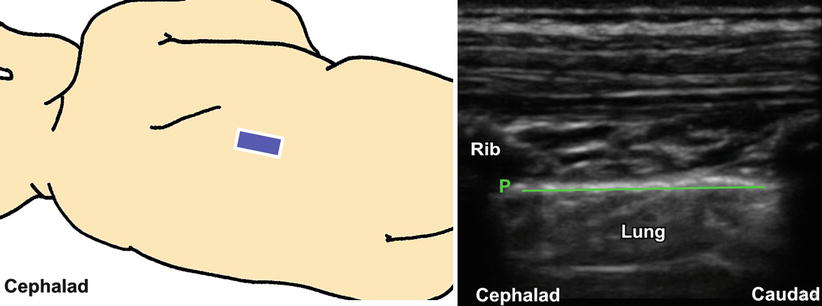
Fig. 73.7
Ultrasound image of the intercostal space. P pleura
Both in-plane and out-of-plane approaches can be used. For the in-plane approach, the needle is introduced at the inferior end of the probe and directed cephalad to the nerve between the internal and innermost intercostal muscles. For the out-of-plane approach, the needle is inserted at the inferior border of the rib to reach the nerve. Local anesthetic is injected following aspiration and injection of a test dose of D5W to visualize the spread which will expand the fascial plane.
Rectus Sheath Block
Introduction, Indications, and Complications
The rectus sheath is formed from the aponeuroses of the three abdominal muscles—external oblique, internal oblique, and transversus abdominis—and encloses the rectus abdominis muscles. The left and right sheaths join at the linea alba in the midline. Above the arcuate line, the rectus muscles sit on the posterior rectus sheath derived from the aponeurosis of the internal oblique and transversus abdominis. Below the arcuate line, the posterior rectus sheath terminates and all three aponeuroses pass superficial to the rectus muscles. The lower seven intercostal nerves (T6–T12), together with the L1 nerve, innervate the anterior abdominal wall. The nerves course anteriorly, lying between the internal oblique and transversus abdominis muscles, and enter the rectus sheath at the posterolateral edge of the rectus abdominis muscle. They then penetrate through the muscle anteriorly to supply the skin.
This block is indicated for midline abdominal incisions (e.g., epigastric and umbilical hernia repair). By placing local anesthetic between the rectus muscle and the posterior rectus sheath bilaterally, the paraumbilical area can be anesthetized. Although not discussed here, an umbilical nerve block can be performed for umbilical hernia repair [4]. Potential complications include peritoneal puncture and puncture of inferior epigastric vessels causing hematoma. The use of ultrasound can reduce these risks and is recommended.
Patient Positioning, Preparation, Equipment, and Dosage
With the child in supine position, the skin is cleaned with antiseptic solution. Prepare the probe surface by applying a sterile adhesive dressing if an ultrasound approach is used.
A 50-mm, 22-G short-beveled needle is used. Choices of local anesthetic include 0.2 % ropivacaine and 0.25–0.5 % bupivacaine. For children aged up to 7 years, 0.2 mL/kg 0.2 % ropivacaine should be used. For older children, 0.2–0.3 mL/kg 0.5 % levobupivacaine is required. The depth of the posterior sheath is usually less than 1 cm.
Landmark Technique
The point of needle insertion is at the lateral edge of the rectus abdominis muscle at the level of the umbilicus (Fig. 73.8). The needle is inserted at 60° to the skin, pointing medially. Advance the needle slowly until a “pop” or give is felt, indicating a loss of resistance as the needle pierces the anterior rectus sheath. Local anesthetic is deposited after aspiration. The block is repeated on the other side.
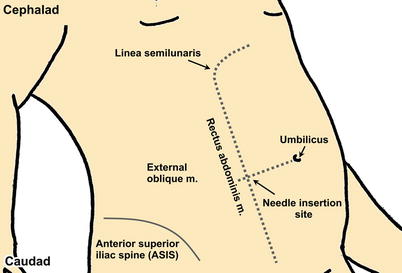
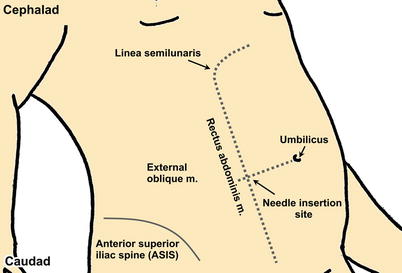
Fig. 73.8
Surface anatomy for rectus sheath block
Nerve Stimulation Technique
Nerve stimulation is rarely performed with these blocks.
Ultrasound-Guided Technique
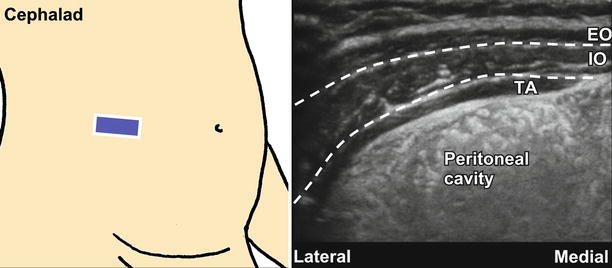
A linear (13-6 MHz) probe is used for a penetration depth of a few cm, depending on the child’s age. The probe is placed in a transverse plane on the anterior abdominal wall to first obtain the view of the three muscle layers: external oblique, internal oblique, and transversus abdominis (Fig. 73.9). Scan medially to identify the rectus muscle, which is oval shaped and enveloped by the hyperechoic rectus sheath. The muscle lies medial to the internal oblique on the same plane. Color Doppler can be used to visualize the inferior epigastric vessels which run through the rectus muscle. The target site for local anesthetic is the plane between the rectus muscle and the posterior rectus sheath (the nerve is too small to be seen).
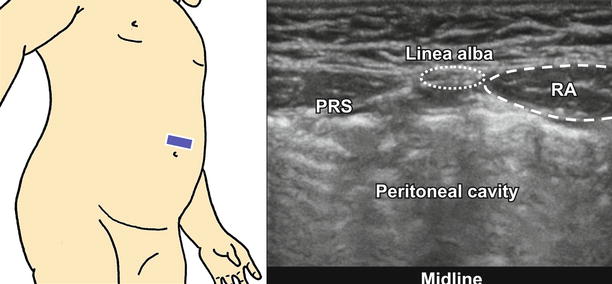
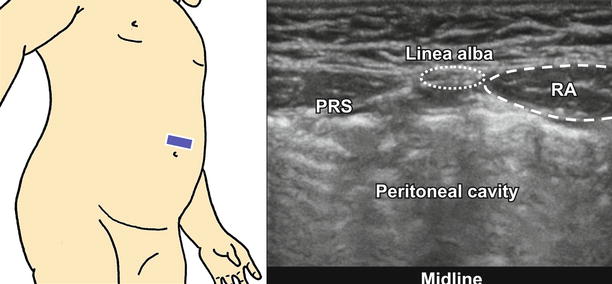
Fig. 73.9
Ultrasound image of the abdominal wall and rectus sheath. PRS posterior rectus sheath, RA rectus abdominis muscle
An in-plane approach is preferred. The needle is inserted in a lateral-to-medial direction and directed to the plane between the rectus muscle and the posterior rectus sheath [5]. Avoid entering the belly of the rectus muscle (which contains the inferior epigastric vessels) by approaching from the lateral side of the muscle. A test dose of D5W is injected to confirm needle-tip position and visualize spread. Local anesthetic is deposited after negative aspiration. To achieve optimal blockade, the block can be performed at the upper and lower ends of the incision bilaterally (i.e., a total of four blocks).
Transversus Abdominis Plane (TAP) Block
Introduction, Indications, and Complications
The transversus abdominis plane (TAP) is the fascial plane between the internal oblique and transversus abdominis muscles in the anterior abdominal wall. It is traversed by the lower seven intercostal nerves (T6–T12) and the L1 nerve, which innervate the anterior abdominal wall. Deposition of local anesthetic in this plane results in unilateral blockade of the skin, muscle, and parietal peritoneum of the anterior abdominal wall. This block is indicated for treatment of postoperative pain for various abdominal and pelvic surgeries and is an alternative to epidural analgesia in children with contraindications to neuraxial block. It may also substitute ilioinguinal and iliohypogastric block since blockade of the L1 nerve can be achieved.
Patient Positioning, Preparation, Equipment, and Dosage
The child can be either supine or lateral, although a more posterior approach permits a more proximal block location for better results. Clean the skin with antiseptic solution. Prepare the probe surface by applying a sterile adhesive dressing if an ultrasound approach is used.
A 50-mm, 22-G short-beveled needle is used. The recommended local anesthetic dose is 0.2–0.3 mL/kg of 0.25 % bupivacaine or 0.2 % ropivacaine on each side (up to a maximum of 3 mg/kg).
Landmark Technique
The triangle of Petit—an area at the lateral abdominal wall bounded anteriorly by the external oblique, posteriorly by the latissimus dorsi, and inferiorly by the iliac crest—is identified (Fig. 73.10). The internal oblique muscle forms the floor of this triangle, so it is the only area of the abdominal wall where this muscle can be localized directly. Since palpation of the triangle of Petit in an anesthetized child can be difficult, an ultrasound-guided block may be a better option.
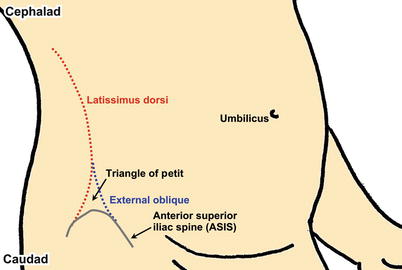
Fig. 73.10
Surface anatomy for transversus abdominis plane block
The point of needle insertion is in the triangle at the point just anterior to the attachment of the latissimus dorsi to the external lip of the iliac crest [6]. The needle is introduced perpendicularly to the skin. Walk off the iliac crest when the needle contacts bone. Advance slowly until a “pop” or give is felt as the needle penetrates the internal oblique muscle to enter the TAP. Local anesthetic is injected after negative aspiration. The block is repeated on the other side for a midline or transverse incision.
Nerve Stimulation Technique
Nerve stimulation is not used for these blocks.
Ultrasound-Guided Technique
A linear (13-6 MHz) probe is used for a penetration depth of a few cm. Occasionally, a curved probe is needed for obese patients. The probe is placed in a transverse plane on the midaxillary line, between the costal margin and the iliac crest, to visualize the three muscle layers separated by the hyperechoic fascia: external oblique, internal oblique, and transversus abdominis (Fig. 73.11). The internal oblique is the widest muscle layer, while the transversus abdominis is the thinnest. The peritoneum and bowel are seen underneath the transversalis fascia deep to the transversus abdominis.