Fig. 11.1
Anatomy of the sphenopalatine ganglion (From Gauci C. Manual of RF techniques, 2004, FlivoPress, Meggen (LU), Switzerland)
The ganglion consists of three types of nerve fibers (Fig. 11.3):
1.
Preganglionic parasympathetic (visceromotor) fibers to the lacrimal, nasal, and palatine glands, reaching the ganglion from the facial nerve through the greater superficial petrosal nerve and the nerve of the pterygoid canal.
2.
Sympathetic fibers coming from the superior cervical ganglion and the internal carotid plexus reaching the ganglion via the deep petrosal nerve which joins the greater superficial petrosal nerve to form the Vidian nerve.
3.
Many afferent fibers crossing the ganglion, originating from the nasal cavity, the soft palate, and the pharynx on their way to the Gasserian ganglion through the maxillary nerve. There is also direct contact between the anterior horn of the spinal cord and the neuro-humeral axis (adenohypophysis) [1, 2]. As the SPG plays a role in the innervation of the brain vascularization, and as such has been described in the “trigeminal vascular system,” it has been suggested that it is probably involved in several forms of vascular headaches and atypical facial pains [3].
Blockade of the Sphenopalatine Ganglion
Blockade of the SPG by local application or injection of a local anesthetic or cocaine has already been described as early as 1908 as an effective method in the treatment of headache; pain in the eyes, mouth, and ears; lumbosacral pain; arthritis, glaucoma; and hypertension [4]. SPG block with local anesthetics may be used for the treatment of acute migraine headache, acute cluster headache, and a variety of facial neuralgias including Sluder’s, Vail’s, and Gardner’s syndromes. This treatment is also useful in the management of status migrainosus and chronic cluster headache. Later on, neurolytic fluids such as alcohol have been used, but uncontrollable spread of fluids has limited the use of this procedure. RF lesioning is a focal neurolysis, making the lesion only around the electrode tip.
The lateral approach is recommended for neurodestructive procedures of the sphenopalatine ganglion in order to avoid lesioning of the maxillary nerve [5].
Radiofrequency lesioning of the sphenopalatine ganglion has predominantly been studied for the treatment of chronic cluster headache unresponsive to conventional management, e.g., drug therapy [6].
The SPG is situated in a richly vascularized region, responsible for a rapid evacuation of the applied heat. Moreover, the size of the ganglion exceeds the size of the RF lesioning. These anatomical characteristics form an explanation for the fact that total nerve destruction of the SPG is never achieved following RF conventional thermolesion using 22-G needles.
The adapted delivery method of the high-frequency current, termed pulsed radiofrequency, delivers the current in bursts of 20 ms followed by 480 ms downtime during which the generated heat is allowed to wash out. In this way, higher voltage, usually 45 V, can be used without generating the neurodestructive temperature (i.e., 43 °C) in the nerve tissue. Pulsed radiofrequency is generally considered as safer than conventional radiofrequency; up till now, no neurological side effect or complication has been mentioned with pulsed radiofrequency treatment of a wide variety of pain syndromes.
Indications for Sphenopalatine Radiofrequency Treatment
I.
Major indication:
1.
Cluster headache
II.
Minor indications:
1.
Atypical facial pain in the maxillary region
2.
Side-locked migraine
3.
Remaining frontal headache after treatment of cervicogenic headache
4.
Trigeminopathy with parasympathetic features such as lacrimation, rhinorrhea, or mucosal congestion
Cluster headache, the major indication for radiofrequency treatment of the sphenopalatine ganglion, is a relatively rare disorder compared with migraine headache. An attack is typically brief, lasting 15 min to 2 h. Attacks occur in groups at the rate of one to several attacks a day over a period of several weeks to many months. The series of attacks may occur twice a year with remission of up to 20 years. When no remission occurs for more than 1 year, the disorder is considered to be chronic. The pain is strictly unilateral and typically in the temporal and periorbital region. The intensity of the attacks is of such severity that some patients have termed cluster headache “suicide headache.” Patients may also use the description of a hot poker being pushed into the eye.
Technique
It is essential that this technique be performed only with fluoroscopic control.
In case patients are using clopidogrel or ASA, they are asked to stop this treatment 5 days prior to the intervention. When patients use coumarin and its derivatives, the intake of these drugs should be interrupted and the INR controlled before the procedure. INR of 1.8 or less is appropriate.
Patient Positioning and Visualization of the Sphenopalatine Ganglion
The patient is lying supine with the head on a radiolucent rest. The head should be gently taped to the headrest in order to prevent movements. The C-arm of the fluoroscope must be positioned in the axis of the operating table.
For a good and consistent anatomical orientation, it is recommended to have the image on X-ray-screen in the same position as the patient is lying (Fig. 11.4).


Fig. 11.4
Patient positioning for the radiofrequency procedure of the sphenopalatine ganglion, C-arm in the axis of the operating table. Image on screen in the same position as the patient
To reduce the operator’s and patient’s exposure to the X-ray beam as much as possible, it is recommended to place the C-arm in lateral position prior to activating the fluoroscope. The position of the fluoroscope is then adjusted until both angles of the mandible are superimposed. This will be achieved by moving the C-arm in both the frontal and axial planes. Next, move the C-arm to a more cranial and ventral position to visualize the essential anatomical structures: the sella turcica, base of the skull, sphenoid sinus, petrous bone, and fossa pterygopalatina. The fossa should now become visible as a “vase” with its base on the floor of the sphenoid sinus. Readjustment of the C-arm is often required to get sharp walls of the fossa. The ganglion is situated in the superior aspect of the fossa.
Needle (Cannula–Electrode) Insertion
In order to find the entry point of the electrode, a metal ruler is projected over the fossa on the side of the patient and a line is drawn over the skin (Fig. 11.5). Palpate the region and mark a point on the drawn line just at the inferior aspect of the zygomatic arch. The entry trajectory runs through the mandibular notch (space between anterior and posterior mandibular ramus (Fig. 11.6)). At first, with a 22-G 2–3-in. needle, local anesthesia is delivered through the skin and the mandibular notch to the deeper soft tissues. This entry point allows the controlling and is important for reaching the sphenopalatine fossa. If necessary, the entry point is corrected.
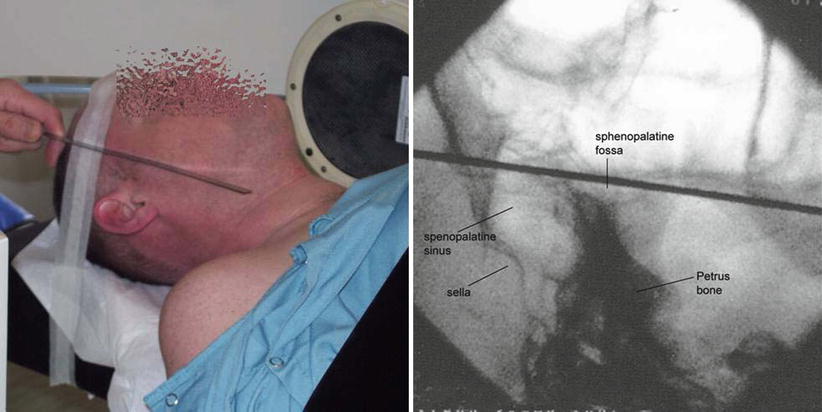
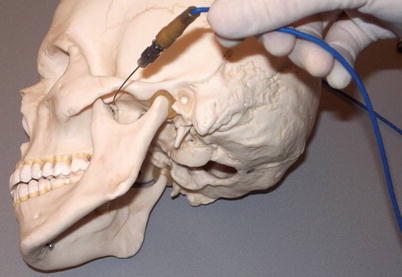
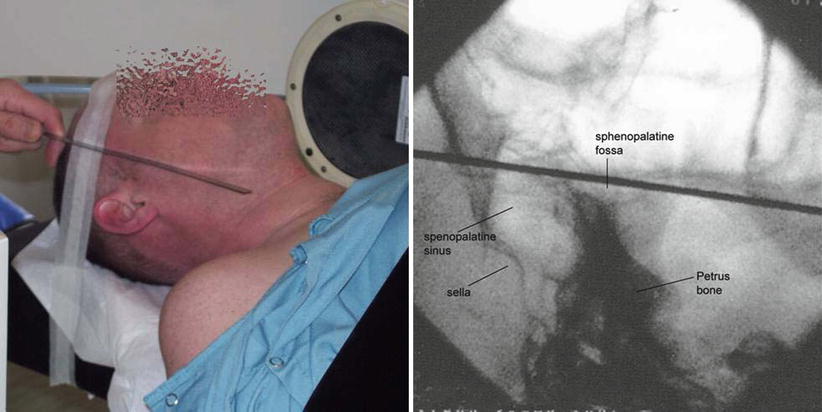
Fig. 11.5
Metal ruler projected over the fossa pterygopalatina, patient and fluoroscopic, X-ray lateral view
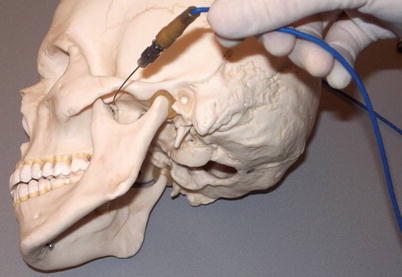
Fig. 11.6
Needle direction to the sphenopalatine ganglion on a model of the skull, infrazygomatic, through mandibular notch
An SMK C-10 needle with a 5-mm active tip is then introduced infrazygomatically to the fossa in a slight anterior and cephalic direction and carefully advanced under lateral fluoroscopic guidance. In case of bone contact, the direction of the needle should be corrected to the target point. After insertion of about 4–5 cm or in case of doubt regarding the depth of the needle, a control in AP projection is performed. The final position is reached when the needle tip has passed the lateral wall of the nose (Fig. 11.7). Just before reaching the end position, the needle may hit the maxillary nerve causing a very unpleasant sensation for the patient. Patients should be informed prior to starting the procedure of this possibility and instructed to signal this straight away. If it occurs, stop advancing the needle immediately and inject carefully and slowly 0.5–1 ml local anesthetic. After waiting approximately one minute, the needle can be redirected to reach the final position.
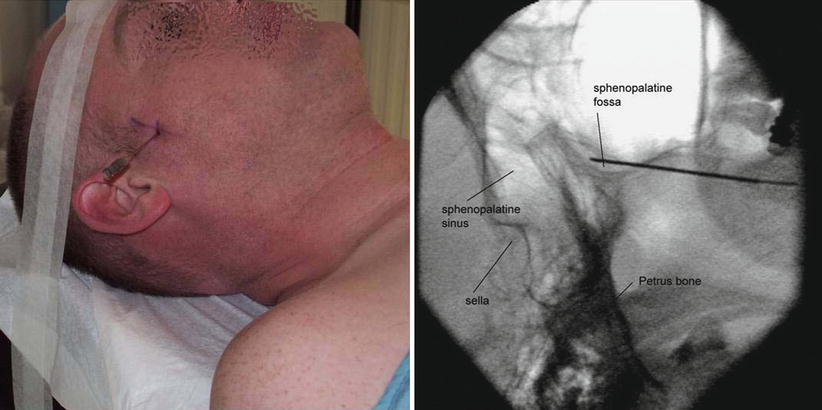
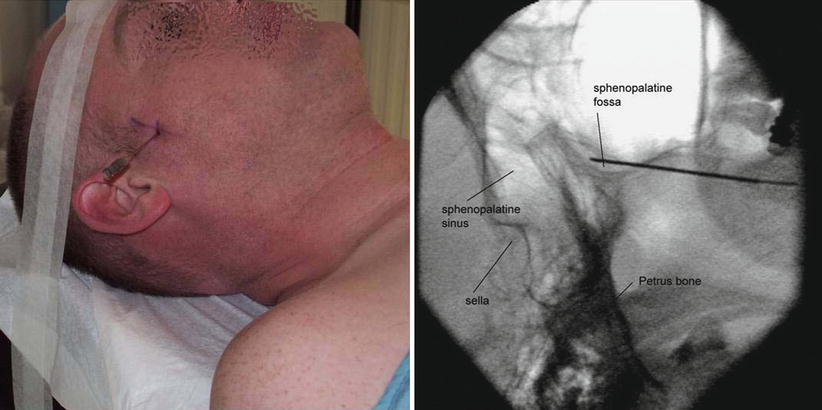
Fig. 11.7
Electrode positioning to the sphenopalatine ganglion, X-lateral view, patient and fluoroscopic
On the AP projection, the nasal septum should be in the midline just over the dens. The needle tip must then be in the lateral wall of the nasal cavity (Fig. 11.8).
Fig. 11.8
Schematic and fluoroscopic visualization of the sphenopalatine ganglion in AP projection
Electrostimulation
At 50 Hz, paresthesia should be felt under 0.7–1.0 V (also depending on the amount of local anesthetic already given and on the duration of interval between administration of the local anesthetic and the electrostimulation). The patient must feel the stimulation in the nose or soft palate. If the paresthesia is felt in the upper teeth or lip, the cheek, or the outer part of the nose, the needle is too close to the maxillary nerve and the needle should be redirected more medially. If stimulation is felt in the hard palate, the needle point is too close to the palatine nerves and the needle must then be redirected more posteriorly and medially. If the position is correct (confirmed with fluoroscopy and electrostimulation), 1–2 ml of local anesthetic is injected. Part of it can flow in the nose and pharynx causing a bitter taste. After having waited for 1–2 min, an RF lesioning of the ganglion is performed.
Radiofrequency Lesion
Radiofrequency lesions are commonly performed in series of two or three, for 60 s at 70–80 °C. Between each lesion, the electrode is moved medially for a few mm until the septum has been touched.
Pulsed radiofrequency current is applied at 45 V for 2 min. After moving the needle to a more medial position, a second treatment is performed.
Complications
Total destruction of the SPG causes dryness of the eye; an “open nose,” since the mucosa has less inclination to swell; and numbness of the palate [8]. Because of the size of the ganglion, the use of 22-G needles, and the high vascularization of the environment, total destruction of the SPG is never achieved.
Other side effects and complications are:
1.
Unilateral sensory loss of the palate: this is usually transient, but you must warn the patient that incidentally it may persist for a longer period.
2.
Epistaxis: in 3–5 % of cases. At the end of the procedure, the patient may sit up with a gauze under the nose. In case of a nasal bleeding, this stops within 10 min.
3.
Hematoma of the cheek: < 1 %, can be treated with pressure and ice packs.
4.
Denervation of the maxillary nerve. This is caused by a wrong technique! Reassure the patient and prescribe antiepileptics like pregabalin and/or clonazepam.
5.
Facial nerve block or diplopia due to spread of local anesthetic to the facial nerve in front of the ear or to the orbit. Reassure the patient and let the patient go home after normalization.
6.
A few weeks after the procedure, very slight intermittent bleeding from the nose may occur, however very seldom. Consultation at an ENT department is recommended.
Evidence for Radiofrequency Treatment of the Sphenopalatine Ganglion
Radiofrequency treatment is indicated when conventional treatment fails. Considering the severity of the pain and the relative low incidence of this syndrome, performing randomized controlled trials comparing radiofrequency treatment to sham intervention is hardly justifiable from an ethical point of view. The comparison with the “gold standard” of conventional treatment may be considered, but for most patients, neurodestructive treatment is the last resort. These factors may explain why no controlled studies have been published up till now and will most likely not be performed.
Several retrospective studies report a long-term effect of radiofrequency treatment of the SPG. Sanders and Zuurmond [6] reported RF treatment of the SPG in 66 patients. Fifty-six patients suffered episodic cluster headache and 10 patients had the chronic form.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree