Gravity reduces blood pressure. Patients with a reasonable, but low, pressure measured in the arm may potentially have ischemia in an elevated head or lower extremity.
Perioperative positioning problems have not been well studied. In many cases, etiologic factors are not well defined or known, although many have been proposed. Although some etiologies are clear (e.g., direct compression of a stoma in a prone-positioned patient that causes ischemia to the externalized stomal tissues), others are not as evident (Fig. 22-1). For example, many plaintiff experts in malpractice legal cases have pronounced that inappropriate patient positioning by anesthesiologists has caused perioperative ulnar neuropathy. Although there is little doubt that direct pressure on ulnar nerves can cause ischemic neuropathy, in many cases it is well documented that the anesthesiologists diligently placed their patients into positions that would avoid direct pressure on their ulnar nerves. Despite this deliberate, presumably preventive approach to patient positioning, patients have developed perioperative ulnar neuropathy.

It is overly simplistic to assume all perioperative neuropathy is due to direct compression of the nerve. Other factors, such as inflammation may also be involved.
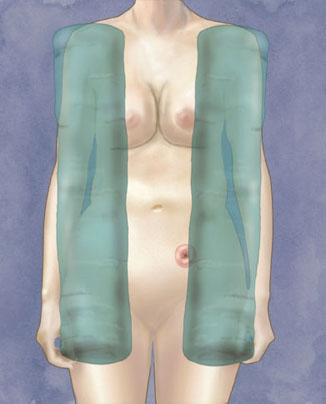
Figure 22-1 Soft tissues can be compressed and even become ischemic if there is too much pressure on them for long periods of time. This figure illustrates how chest rolls may compress the lateral aspects of large breasts or a stoma in prone-positioned patients.
Why would this happen? Most patients who develop perioperative ulnar neuropathy do not become symptomatic until 2 to 5 days after their procedures (1). However, direct compression to nerves should cause immediate ischemia and symptoms of neuropathy. Thus, it appears that factors beyond intraoperative positioning may be at play. Further, recent findings suggest that a number of patients with new-onset ulnar neuropathy have systemic lymphatic microvasculitis of their peripheral nerves, which is treatable with corticosteroids (2). These findings suggest that the perioperative inflammatory response associated with most surgical procedures may be a factor in the development of what initially appeared to be a simple isolated peripheral nerve injury.
There is much more to learn about positioning problems, and simple etiologic assumptions may not be correct until scientifically proven. This chapter explains the mechanisms of soft tissue injury and common perioperative soft tissue injuries, cognizant that etiologic factors and appropriate preventive measures may not be known at this time.
II. Mechanisms of Soft Tissue Injury
Tissue stretch and compression are commonly considered to be associated with positioning-related problems in anesthetized or sedated patients. The perioperative period anatomic considerations include stretch and compression.
A. Stretch
Nerves are typically well vascularized by short nutrient arteries that divide and anastomose upon and within them. These effectively are the structures of a nerve’s vasa nervosum (Fig. 22-2). In peripheral nerves, these minute arteries profusely anastomose to form an unbroken intraneural net. This net rarely leaves any particular segment of a peripheral nerve dependent on a single vessel for nutrient support. This net is not seen as commonly in central nerve tissue.
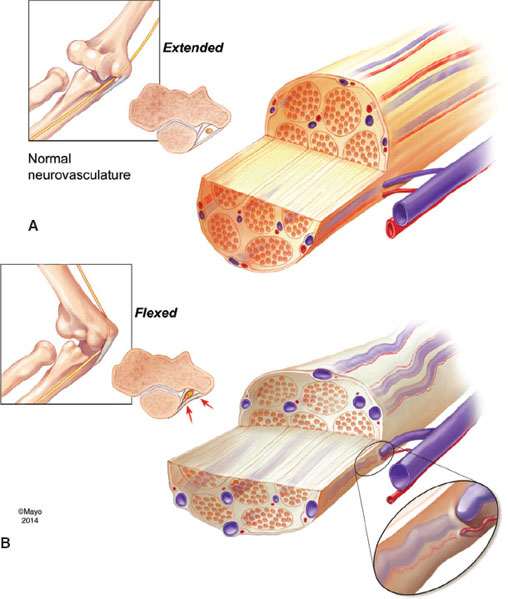
Figure 22-2 Effect of tissue stretch and compression on nerve vasa nervosum. This example shows potential ulnar nerve injury with elbow flexion. A: Extended elbow and relaxed ulnar nerve, noting patent perforating arterioles and venules. B: Flexed elbow, noting that stretch of the penetrating arterioles and venules from elongation of the ulnar nerve or compression by the cubital tunnel retinaculum can lead to vessel kinking and result in reduced arteriole blood flow from outside to inside the nerve (causing direct ischemia) and venous congestion from reduced venule outflow as vessel exits the nerve (leading to indirect ischemia). Prolonged ischemia can lead to nerve injury.
Stretch of nerve tissue, especially to more than 5% of resting length, may kink or reduce the lumens of feeding arterioles and draining venules (3). This phenomenon can lead to direct ischemia from reduced arteriole blood flow; indirect ischemia from venous congestion, increased intraneural pressure, and the need for high driving pressures of arteriolar blood flow; or both. Prolonged periods of ischemia may cause transient or permanent nerve injury. The lack of extensive vascular nets in central nervous tissue suggests that less stretch may be tolerated.
Soft tissues generally are less susceptible to stretch injury than nervous tissue. They are often more compliant and elastic, and many peripheral soft tissues do not need the same level of blood flow as nervous tissue. Nonetheless, prolonged stretch of any soft tissue may result in ischemia and tissue injury. Unique perioperative patient positions may increase the risk of soft tissue stretch (e.g., prone positions and their impact on breast tissue) (Fig. 22-1).
B. Compression
Direct pressure on soft and nerve tissues may reduce local blood flow and disrupt cellular integrity, resulting in tissue edema, ischemia, and, if prolonged, necrosis. The impact is especially damaging to ischemic-susceptible soft tissues (e.g., stomas associated with gastrointestinal diversions into cutaneous stomas) (Fig. 22-1).
III. Common Perioperative Neuropathies
A. Upper Extremity Neuropathies
Ulnar Neuropathy
Ulnar neuropathy is the most common perioperative neuropathy (4). There are a number of factors that may be associated with ulnar neuropathy, including direct extrinsic nerve compression (often on the medial aspect of the elbow), intrinsic nerve compression (associated with prolonged elbow flexion), and inflammation. Key points of interest are:
• Timing of postoperative symptoms: Most develop during the postoperative, not the intraoperative, period. There are good data that most surgical patients who develop ulnar neuropathy experience their first symptoms at least 24 hours postoperatively. This suggests that the mechanism of acute injury occurs primarily outside the operating room setting. Parenthetically, medical patients also develop ulnar neuropathies during hospitalization.
• Impact of elbow flexion: The ulnar nerve is the only major peripheral nerve in the body that always passes on the extensor side of a joint, in this case, the elbow. All other major peripheral nerves primarily pass on the flexion side of joints (e.g., median and femoral nerves). This anatomic difference may play a role in some perioperative ulnar neuropathies. In general, peripheral nerves begin to lose function and develop foci of ischemia when they are stretched >5% of their resting lengths. Elbow flexion, particularly >90 degrees, stretches the ulnar nerve. Prolonged elbow flexion and stretch of the ulnar nerve can result in sufficient ischemic areas to cause symptoms in awake and sedated patients and potential long-lasting damage in all patients.
• Anatomy and elbow flexion: Prolonged elbow flexion of >90 degrees increases intrinsic pressure on the nerve and may be as important an etiologic factor as prolonged extrinsic pressure (5,6). The ulnar nerve passes behind the medial epicondyle and then runs under the aponeurosis that holds the two muscle bodies of the flexor carpi ulnaris together. The proximal edge of this aponeurosis is sufficiently thick, especially in men, to be separately named the cubital tunnel retinaculum. This retinaculum stretches from the medial epicondyle to the olecranon. Flexion of the elbow stretches the retinaculum and generates high pressures intrinsically on the nerve as it passes underneath (Figs. 22-3 and 22-4).
 VIDEO 22-1
VIDEO 22-1
Ulnar Nerve Compression
• Forearm supination and ulnar neuropathy: Supination of the forearm and hand does not, by itself, reduce the risk of ulnar neuropathy. The action of forearm supination occurs distal to the elbow. Supination is typically used when positioning arms on arm boards or at patients’ sides because of the impact it has on humerus rotation. That is, supination is uncomfortable for most patients, and they will externally rotate their humerus to increase comfort. It is this external rotation of the humerus that lifts the medical aspect of the elbow, including the ulnar nerve, from directly resting on the table or arm-board surface. This rotation helps reduce extrinsic pressure on the ulnar nerve.
• Outcomes of ulnar neuropathy: Forty percent of sensory-only ulnar neuropathies resolve within 5 days; 80% resolve within 6 months. Few combined sensory and motor ulnar neuropathies resolve within 5 days; only 20% resolve within 6 months, and most result in permanent motor dysfunction and pain. The motor fibers in the ulnar nerve are primarily located in its middle. Injury to those fibers likely is associated with a more significant ischemia or pressure insult to all of the ulnar nerve fibers, and recovery may be prolonged or not possible.
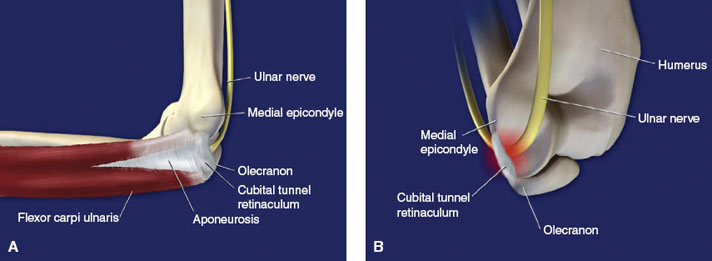
Figure 22-3 A: The ulnar nerve of the right arm passes distally behind the medial epicondyle and underneath the aponeurosis that holds the two heads of the flexor carpi ulnaris together. The proximal edge of the aponeurosis is sufficiently thick in 80% of men and 20% of women to be distinct anatomically from the remainder of the tissue. It is commonly called the cubital tunnel retinaculum. B: Viewed from behind, the cubital tunnel retinaculum intrinsically compresses the ulnar nerve when the elbow is progressively flexed beyond 90 degrees and the distance between the olecranon and the medial epicondyle increases.
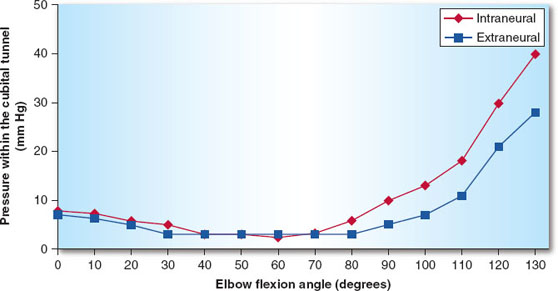
Figure 22-4 Pressure within the cubital reticulum at the elbow escalates once the angle of elbow flexion reaches and exceeds 90 degrees. (From Gelberman RH, Yamaguchi K, Hollstien SB, et al. Changes in interstitial pressure and cross-sectional area of the cubital tunnel and of the ulnar nerve with flexion of the elbow. An experimental study in human cadavera. J Bone Joint Surg. 1998;80(4):492–501, with permission.)

Ulnar neuropathy manifested by sensory loss only has a good prognosis. Most resolve spontaneously within a few days or months.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








