SURGICAL CRITICAL CARE
CHAPTER 46 |
| INTENSIVE CARE UNIT: THE ESSENTIALS–INCLUDING ASSESSMENT OF SEVERITY OF CRITICAL ILLNESS |
Patients managed by acute care surgeons frequently present with organ system dysfunction or are at high risk to develop organ system dysfunction, increasing their risk of adverse outcome and death. The presence of infection, tissue injury, large volume transfusions, or ischemia/reperfusion in this patient population may contribute to the development of a systemic inflammatory response or subsequent immunosuppression contributing to altered tissue healing, infectious complications, organ injury, and organ failure.1–6 Thus, critically ill or injured acute care surgery patients frequently require critical care management to provide timely and appropriate therapeutic interventions, achieve adequate endpoints of resuscitation, appropriately assess the risk and presence of complications, mitigate the risk of organ dysfunction, and treat organ dysfunction and failure. In this chapter, the contribution of intensive care unit (ICU) and critical care management for the acute care surgical patient is reviewed as (1) timely, targeted, and appropriate application of therapeutic interventions; (2) assessment and recognition of risk; and (3) prevention of complications and minimization of the propagation of organ injury.
THE CRITICAL CARE TEAM AND SYSTEM OF CARE
The concept of critical care has evolved dramatically since the first three-bed ICU was established by Walter Dandy at the Johns Hopkins Hospital in 1926.7 ICUs were originally developed to provide increased nurse staffing ratios, increased monitoring, and ventilator management. As our understanding of the pathophysiology of critical illness and its treatment has progressed and as patient acuity has increased over time, the concept of critical care has evolved into one of a multidisciplinary team providing a system of care to deliver timely and targeted interventions to address the underlying pathologic condition and the global and organ-specific dysfunction. This is achieved while limiting the risk of complications and iatrogenic organ injury. Critical care may be defined as the process of high-intensity physiologic monitoring coupled with short response pharmacologic, hemodynamic, ventilatory, and procedural interventions. These efforts are designed to reestablish normal homeostasis and minimize primary, secondary, and iatrogenic injury. Importantly, the mitigation of risk of complications and further exacerbation of organ injury may be the most significant contribution of critical care systems. Critical care is generally the most expensive, technologically advanced, and resource intensive component of medical care. Despite the high incremental cost of providing intensivist-directed critical care management, numerous studies have demonstrated considerable incremental benefits of intensivist-directed critical care on mortality, morbidity, and overall cost.8–15
Considerable heterogeneity exists across ICUs relative to physician responsibility, physician staffing and availability, provision of ancillary services, and organization of teams and processes. This heterogeneity complicates the ability to assess the contribution of individual components of critical care to the outcome. In Table 46.1, various descriptions of physician staffing models are provided.16 In general, closed unit staffing models provide reductions in mortality when compared to open unit models–913 and the inclusion of multidisciplinary teams appears to provide incrementally greater reductions in mortality when combined with closed unit models.17
TABLE 46.1
TERMINOLOGIES TO DESCRIBE ICU PHYSICIAN STAFFING MODELS
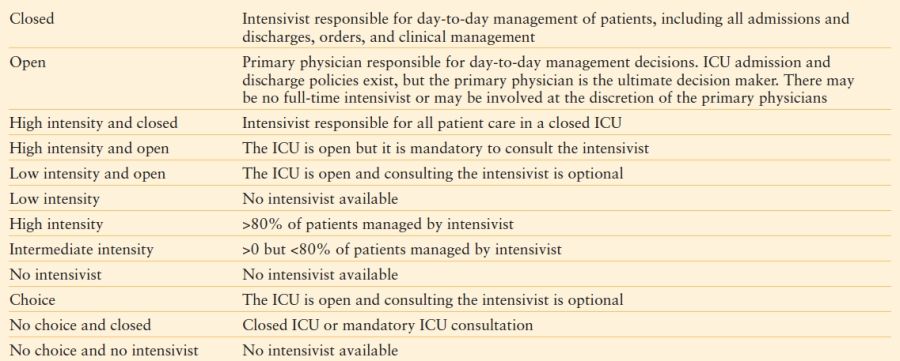
Gajic O, Afessa B. Physician staffing models and patient safety in the ICU. Chest. 2009;135:1038–1044.
TIMELY, TARGETED, AND APPROPRIATE APPLICATION OF THERAPEUTIC INTERVENTIONS
Regardless of the structural organization of individual ICUs, the provision of timely, targeted, and appropriate therapeutic interventions improves the outcome of critically ill and injured patients. These concepts are discussed in detail in Chapters 4, 7, 12, and 13and in chapters in Section IV. Mainstays of therapy for the critically ill acute care surgery population include (1) goal-directed resuscitation and appropriate inotropic support, (2) appropriate and timely antibiotic therapy, and (3) timely and effective source control of infectious, hemorrhagic, or ischemic insults.
While early resuscitation has long been accepted to improve outcomes in the critically ill acute care surgery population, debate continues regarding strategies and appropriate endpoints.4,18–23 Measures of tissue hypoxia such as base deficit, elevated lactate, and decreased mixed venous saturation correlate with the development of organ system dysfunction and mortality following the onset of hemorrhage and sepsis and early correction (likely within 6 hours in at-risk groups) of these abnormalities is associated with improved outcomes.4,18–21,23–29 Resuscitation strategies that target adequate tissue oxygenation as endpoints, and that both respond to the alteration in physiology and limit excessive fluids, appear to have better outcomes than those that do not employ these measures. However, no perfect set of markers has been identified to guide resuscitation in all settings.
For patients with both community and hospital-acquired infections, the time to appropriate antibiotic therapy has been shown to significantly alter outcomes. Thus, establishment of the likelihood of the presence of infection, the source of infection if present, likely pathogens, and potential resistance of pathogens involved, all factor into timing and selection of antibiotic therapy. Inadequate empiric antimicrobial therapy is associated with twice the mortality in studies of mixed hospital-acquired infections,30 ventilator-associated pneumonia,31–33 hospital-acquired bloodstream infections,34,35 and peritonitis.36,37 Prior antibiotic exposure was associated with inadequate empiric therapy in many of these studies with selection of more resistant pathogens.30,34,36 As the severity of illness increases, the timing of antibiotic initiation appears to assume increasing importance in septic patients. In a study of 335 surgical ICU patients with infections, using logistic regression analysis, Barie et al.38 demonstrated that each 30-minute delay in initiation of antibiotic therapy from the onset of fever was associated with a 2% increase in mortality. For patients with septic shock, the influence of antibiotic timing appears to be even greater. In a study of 2,731 patients with septic shock from 14 ICUs in the United States and Canada, Kumar et al.39 demonstrated that each 1-hour delay in antibiotic therapy from the onset of hypotension was associated with a 12% increase in mortality. The increased risk of death was consistent across subcategories including intra-abdominal, skin and soft tissue, respiratory, blood stream, community, and nosocomial infections; only 50% of patients received therapy within 6 hours of the onset of hypotension. These studies highlight the importance of systems that enable the early identification of infectious processes and the administration of early empiric antibiotic therapy appropriate for the clinical setting.
A significant portion of critically ill patients managed by acute care surgeons require source control as part of therapeutic interventions, most commonly patients with intra-abdominal processes or skin and soft tissue infections. Severely septic patients may require rapid resuscitation and stabilization in an ICU setting prior to operative intervention for source control. For patients with necrotizing skin and soft tissue infections, the time to effective source control is associated with outcome and these patients may require multiple operative interventions before source control is achieved.40,41 Critical care support may be required during this period for the treatment of sepsis and septic shock, to support and minimize organ system dysfunction, and to assist with wound management. Critically ill patients with peritonitis present the acute care surgeon with unique challenges. In general, critically ill patients with peritonitis are at higher risk for failure of primary source control and the development of secondary complications such as abdominal compartment syndrome, recurrent intra-abdominal infection (abscess and tertiary peritonitis), and fistula formation than patients with peritonitis who are not critically ill.
One clear demonstration of compliance with timely, targeted, appropriate interventions in critically ill patients is provided through the efforts of the Surviving Sepsis Campaign (SSC).43 The SSC established evidence-based management guidelines and implemented a broad educational program to facilitate integration of these guidelines in clinical practice in North America, South America, and Europe. Elements of the guidelines were grouped or bundled into two sets of targets to be completed within either 6 hours or within 24 hours of admission. Numerous studies have demonstrated an associated benefit of compliance with the SSC.45 A before and after analysis of participating sites was conducted on data submitted from January 2005 through March 2008. Compliance with elements in the bundle increased linearly throughout the period and resulted in a 5.4% adjusted absolute decline in mortality over the 2-year period.46
ASSESSMENT AND RECOGNITION OF RISK: ASSESSMENT OF PATIENTS WITH PERITONITIS
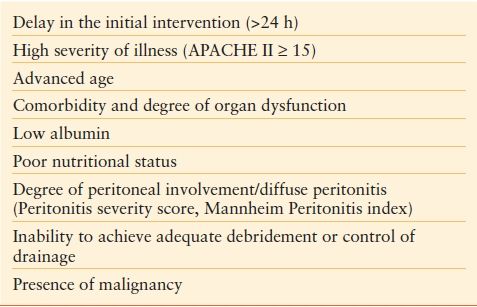
Patients with severe sepsis (organ dysfunction and criteria of systemic inflammatory response syndrome) secondary to peritonitis, while representing a small portion of all patients with peritonitis, are at higher risk of mortality.47 Patients more likely to develop severe sepsis from peritonitis include those with more advanced age, those with diffuse peritonitis, and those with preexisting organ dysfunction.47 Not surprisingly, factors that predict development of severe sepsis are similar to those that predict failure of treatment and mortality from peritonitis as well. Multivariate analysis in numerous studies has identified advanced age, low serum albumin, poor nutrition, preexisting organ dysfunction, and high Acute Physiology and Chronic Health Evaluation (APACHE) II scores as associated with failure of source control and death.48–54 In an analysis of 217 patients entered into a randomized trial of complicated intra-abdominal infections, 14% of patients had APACHE II scores of 15 or greater with failure rates in these patients >40%. If APACHE II scores were >20, failure rate exceeded 50%.55 Each of these risk factors is a measure of the degree of variance from the host’s normal physiologic state. In addition to these physiologic risk factors, the degree of inflammation and bacterial burden within the peritoneum also predicts the risk of failure of source control. Diffuse peritonitis, moderate or extensive residual contamination at the completion of the source control procedure, or inability to achieve adequate source control also predicts failure.54,56–58 Risk factors for failure of source control from intra-abdominal infections are summarized in Table 46.2. Knowledge of these risk factors should be utilized to estimate the postoperative clinical course, to help determine the level of support and monitoring, and predict the likelihood of postoperative intra-abdominal infectious complications. The assessment of risk of failure is important as delays to definitive therapy in patients who fail source control are associated with increased mortality.62
TABLE 46.2
CLINICAL FACTORS THAT PREDICT FAILURE OF SOURCE CONTROL FOR INTRA-ABDOMINAL INFECTIONS55,59,–61
ASSESSMENT AND RECOGNITION OF RISK: MODELING SEVERITY OF ILLNESS IN THE ICU
Scoring systems for severity of illness can broadly be divided into those that are targeted for a specific disease process or organ system (e.g., the Model for End-Stage Liver Disease (MELD) score in liver disease, the Mannheim Peritonitis Index for intra-abdominal infection, and the Glasgow Coma Score for brain injury) and those that are generic for all ICU patients. This section focuses on these generic scores that can be divided into those that assess disease severity on admission and those that assess the degree of organ system derangement or injury at variable time points in any given patient. Scoring systems for severity of illness utilize a variety of demographic, clinical, physiological, and laboratory variables. The most common scoring systems that assess disease severity upon admission include the APACHE, the Simplified Acute Physiology Score (SAPS), and the Mortality Probability Model (MPM), all of which were developed to predict likelihood of survival.63 Common scoring systems used to assess the presence and severity of organ dysfunction on admission and during the ICU stay include the Multiple Organ Dysfunction Score and the Sequential Organ Failure Assessment.63
Each of the three scoring systems used to assess disease severity upon admission and predict outcome (i.e., APACHE, SAPS, MPM) uses variables obtained within a 24-hour period of admission, typically the worst value recorded. Each has had multiple generations, with the most recent version undergoing adjustment of the prediction model based upon new datasets, equations for which are proprietary. Prediction equations for older, nonproprietary versions are no longer being adjusted. Versions of these scores are frequently used to stratify patient severity within studies or to control for variation in severity within a defined population when assessing performance.63 They may also be used to determine eligibility for inclusion in clinical trials, for therapeutic interventions,42,43 or to assess the likelihood of therapeutic failure.55 Generally, these systems perform well when comparing outcome within specific critically ill patient populations, but not across varying populations of critically ill patients.
Measures of organ injury and dysfunction may be used to assess organ dysfunction at admission but may also be used as outcome variables. Thus, they are dynamic, varying among individuals and within a given individual over time and thus can be used to assess and quantitate change in organ function over time. However, outcome prediction and organ dysfunction scores are not mutually exclusive and provide different types of information, which together can complement the clinician’s subjective evaluation of a patient’s status. These scores may be employed to provide a quantitative response to therapy and direct subsequent therapeutic interventions.64,65
More recently, a new system for analysis of sepsis has been developed, the predisposition, insult, response, organ dysfunction (PIRO) system. The PIRO system was created so that a clinically useful staging system, similar to cancer staging, could stratify patients based on their baseline risk for an adverse outcome and their potential to respond to therapy across the very heterogenous patient population defined as septic.66 While further studies are needed, performance for the prediction of outcome in sepsis is very promising.67
PREVENTION OF COMPLICATIONS AND MINIMIZATION OF THE PROPAGATION OF ORGAN INJURY
While relatively few interventions have been shown in randomized, controlled trials to consistently impact outcome in the ICU, outcome of critically ill patients is improving.38 The improvement in outcome is likely related to both the introduction of specific therapeutic strategies that limit the development and progression of organ dysfunction as well as the complex systems of delivery required to provide highly specific and targeted therapies. Several therapeutic strategies that impact the outcome of patients include those involving respiratory management, sedation and delirium management, cardiovascular risk management, renal management, transfusion practices, endocrine support, infection control, nutritional provision, prevention of airway loss, skin breakdown, deep vein thrombosis, and stress ulcers, as well as the safe performance of invasive, bedside procedures. Each of these areas has a large body of literature that continues to support the advancement of care for the critically ill and injured patient. A full discussion of these topics is beyond the scope of a single chapter, although they will be discussed briefly below. Evidence-based guidelines may assist with the appropriate application of many of these areas listed. However, maintaining high level compliance with both simple and complex components of care within each is difficult and is aided by multidisciplinary teams and informatics support.
Respiratory Management
Appropriate respiratory management of mechanically ventilated, critically ill patients impacts the outcome considerably. Strategies directed toward liberation from ventilatory management, prevention of lung and remote organ injury through low volume ventilatory strategies (i.e., ARDS Net), and strategies to limit the development of ventilator-associated pneumonia have important implications for patient outcome.43 Clear support for systems and teams that continuously evaluate the appropriateness and ability to wean patients from ventilator support have been shown to reduce the number of ventilator days and improve outcome.43 Application of weaning protocols, avoidance of weaning of intermittent mandatory ventilation rate, daily spontaneous breathing trials, targeted sedation and daily cessation of sedation, and appropriate use of tracheostomies reduce ventilator days and improve outcomes in certain patient populations. Use of a low-volume ventilation strategy also limits the progression and severity of acute lung injury and acute respiratory distress syndrome, as well as measures of systemic inflammation. However, despite clear data from randomized studies, application of this strategy has been slow to be widely adopted in practice.68 The need for mechanical ventilation and the presence of an endotracheal tube greatly increases the risk of the development of pneumonia. However, the application of several interventions has been shown to limit the risk of pneumonia in randomized studies.69,70 These include spontaneous breathing trials, targeted sedation, head of bed elevation, dental and oral care, and hypopharyngeal suctioning. However, high level compliance with each of these may be difficult to achieve and systems to monitor and enhance compliance may improve their application.71
Sedation and Delirium Management
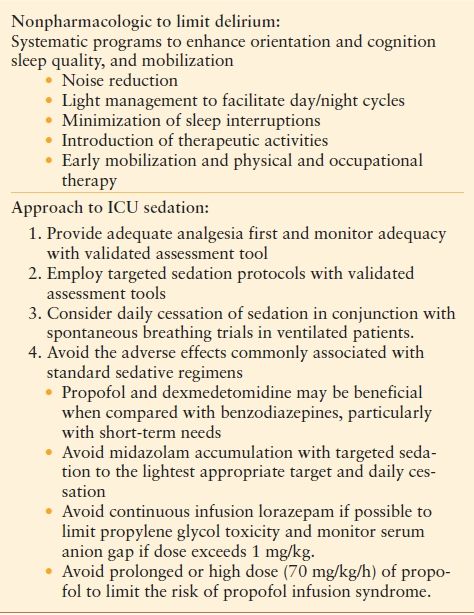
The complex interrelationships between sedation, pain management, sleep, delirium, cognitive dysfunction, and outcome are increasingly recognized but are incompletely understood. While the prevention of pain and anxiety remains an important goal in the management of critically ill patients, oversedation has been recognized to contribute to prolonged mechanical ventilation, altered sleep patterns, and increased delirium.72–75 Targeted sedation and pain control and daily cessation of sedation have been shown to substantially decrease the time of mechanical ventilation, ICU and hospital length of stay, and outcome.73,74 Delirium occurs in up to 80% of ICU patients but is frequently underrecognized.76 The presence and severity of delirium correlates with both cognitive deficits post discharge and overall outcome.–7678 Both the depth of sedation and agents used to provide sedation contribute to the severity of delirium. At present, inadequate data regarding pharmacologic therapy to limit the development of delirium exists to make recommendations.73 For the treatment of agitated delirium, few randomized trials exist and the use of antipsychotics, either conventional (Haldol) or less common agents, may be considered. A summation of recommendations for nonpharmacologic efforts to limit delirium and approach to ICU sedation is provided in Table 46.3.
TABLE 46.3
RECOMMENDATIONS FOR DELIRIUM AND SEDATION MANAGEMENT IN THE ICU
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









