CHAPTER 15

ACUTE CARE SURGERY IN SPECIAL POPULATIONS
ACUTE CARE SURGERY IN THE ELDERLY
Introduction
Surgical emergencies are diverse and challenging for the acute care surgeon. In patients over 60 years, age-related anatomic and physiologic changes as well as preexisting medical conditions can alter clinical presentation and management and have considerable impact on outcomes. As the population of elderly increases globally, it is important for all surgeons to understand how “aging” affects the presentation and progression of acute surgical disease.
In 1900, only 40% of the population lived to age 65; a century later, over 80% live past 65 years.1 Two population trends will impact the age characteristics of elder patients in the near future. Significant increases in the population over 65 years will occur with the aging of the “baby boomers,” the post World War II generation born between 1946 and 1964. This large cluster of seniors will accelerate the percentage of elderly.2 The number of persons over age 65 years is expected to increase by 70 million persons by 2030.3,4 Concomitantly, improvements in life expectancy suggest that the younger cohorts of elderly will live longer and enjoy a more active lifestyle and better health.5 Improvements in longevity have already led to a steady increase in the numbers of the “oldest old,” those over 85 years; by 2030, the number of seniors over age 80 will increase to 19.5 million persons.3 As these two cohorts (boomers and the “oldest old”) age, they will experience the common age-related chronic health conditions, consequences of senility, and the disabilities of “wearing out.” They will require increasing prescription and over-the-counter drug use, physician office visits, and trips to the emergency department (ED).6,7
Injuries will be the most common surgical emergency among elders. While older Americans are injured at lower rates than those under the age of 65 (7,980/100,000 vs. 10,230/100,000 in 2005), they have higher injury mortality rates (118/100,000 vs. 50/100,000).8 The percentage of emergency hospital admissions for injury increases with patient age, as well as hospitalization for injury.4 The same types of injury are experienced in younger people; however, injury pattern, effect, postinjury course, and outcomes differ substantially.9 Seniors aged 65–74 are usually more active and have injury patterns more similar to younger adults (motor vehicle crashes (MVSs) and falls from heights), and as they pass age 80, activity decreases, and the age-related changes, decreased vision, osteoarthritis, balance problems, low-level falls are dominant.
The presence and severity of preexisting disease, American Society of Anesthesiologist (ASA) physical status classification grade, delays in diagnosis, and time to surgery have substantial effects on morbidity and mortality.10 Some have suggested that increasing age is an independent risk factor for operative mortality, while others report conflicting results.10,11
Physiologic Changes Associated with Aging
The combination of normal age-related changes that affect each organ system and the presence of chronic disease states result in a declining physiologic reserve and an enhanced susceptibility to disease.12 The result is a diminished ability to handle the “stress” of surgery, trauma, and infection.
Cardiovascular System Cardiovascular disease is common, seen in 80% of patients over 80 years of age.13 As the heart ages, a progressive loss of myocytes occurs with subsequent enlargement of the remaining myocytes, leading to reduced compensatory capacity and myocardial dysfunction.14 Cardiac function is often affected by depressed myocardial contractility, decreased compliance in response to preload, and poor response to endogenous and exogenous catecholamines. Fibrosis of autonomic tissue causes conduction abnormalities, arrhythmias, and heart block.15 Maintenance of cardiac output is difficult in elderly patients as the aged heart responds poorly to endogenous and exogenous catecholamines and is often preload dependent.14 Cardiac medications, such as beta-blockers, calcium channel blockers, or digitalis, can blunt reflexive- or catecholamine-induced tachycardia. Arteriosclerotic vascular disease, common as we age, predisposes to impaired blood flow to organs.
Pulmonary System Respiratory function declines as the chest wall stiffens, respiratory muscles weaken, and lung elasticity decreases.13 Arterial oxygenation decreases due to alveolar collapse and resultant diminished surface area for gas exchange.16,17 Diminished pulmonary compliance, an inability to mount an effective cough, and impaired gas exchange often result in respiratory insufficiency and failure, especially in the setting of acute illness or injury. The elderly patient developing respiratory distress may appear comfortable as changes in chemoreceptor and respiratory drive are altered.14 Inadequately treated postoperative or injury-related pain results in poor inspiratory effort, atelectasis, and pneumonia.18 Epidural analgesia/anesthesia is an adjunct or alternative to commonly used enteral and parenteral opioids and nonsteroidal anti-inflammatory drugs (NSAIDs).
Renal System Structural and functional changes occur in the kidney as we age. Structural changes include decrease in effective renal cortex, resulting in 20%–25% cortical loss, hyalinization of blood vessel walls, and decrease in the number of glomeruli.19 Functionally, decreased glomerular filtration rate (GFR) and impaired renal tubule reabsorption and secretion result in problems with solute clearance, acid–base balance, and fluid homeostasis. Hormonal responses of the renin-angiotensin-aldosterone axis and antidiuretic hormone are blunted. Despite decreased renal function, serum creatinine concentrations can remain within the normal range due to a decrease in lean body mass (BM) and creatinine production.14 For this reason, serum creatinine concentration alone is an inadequate measure of renal function; creatinine clearance measurement or calculation based on age and BM should be used.
Gastrointestinal System Gastrointestinal function is relatively preserved; however, the catabolic state induced by critical illness or injury leads to rapid muscle breakdown. Protein-deficient malnutrition develops more rapidly in the elderly, and 17%–65% of acutely hospitalized patients become malnourished.14 Impaired nutrition is related to an increased mortality in older patients requiring mechanical ventilation and is an independent risk factor for infection, impaired wound healing, and longer ICU stays. Early and sufficient nutritional support reduces hospital length of stay, mechanical ventilation days, and results in improved outcomes.20,21
Neurologic System Many neurologic and cognitive changes occur in the elderly.12 Cortical atrophy becomes more rapid after age 60 based on several studies of postmortem human brains.22 Pathologic changes such as amyloid deposition and arteriosclerotic cerebrovascular disease affect most past 80 years.13 Decreases in cerebral blood flow and brain oxygen consumption can manifest as blunted sensation (visual, auditory, and tactile), altered cognition, and blunted pain perception. Anxiety, agitation, and delirium are more common in the postoperative and posttrauma period and more difficult to manage. Alterations in cerebellar function, gait, balance, and vision increase the risk of injury, especially falls.
Pharmacology There is an altered response to many drugs in the elderly.23 Older patients often have an exaggerated response to central nervous system (CNS) active drugs due to underlying decline in CNS function and increased sensitivity to benzodiazapines, anesthetics, and opioids. A decreased effect of beta-adrenergic agents exacerbates the changes in autonomic function, leading to decreased baroreceptor reflex and orthostasis. Lastly, caution is advised with all nephrotoxic agents, such as iodinated contrast solutions, antibiotics, diuretics, and vasoactive medications.12
Clinical Presentation
The elderly can present with atypical symptoms or nonspecific complaints for surgical conditions.24 Moreover, the history of the present illness may be difficult, and even impossible to elucidate secondary to dementia or previous neurologic insult (stroke). The medical history is often complex and unless supplemented by a family member or caregiver may be incomplete. Systemic response and findings on physical examination are often benign, especially with abdominal problems and soft tissue infections.
Abdominal pain is the main complaint in 15% of ED visits for older patients. Many physicians report greater difficulty with diagnosis and management of abdominal pain in older patients. In addition, abdominal and pelvis computerized tomography (CT) frequently adds critical information, with change in the diagnosis of acute abdominal pain in elderly patients.25 Thus, early surgical consultation, directed computed tomography, and inpatient monitoring and observation are required for the elderly with a suspected surgical illness.
Perioperative Management of the Elderly
Increasing age in and of itself is not indicative of increased mortality, and many scoring systems have been developed to predict mortality for the elderly patient undergoing emergency surgery.26 Nearly all scoring systems have clinical limitations because of time and amount of data required to calculate the score. The Acute Physiology and Chronic Health Evaluation II score (APACHE II) has been studied for its preoperative predictive value as well as its intended purpose of predicting ICU mortality. The Reiss Index compiles age, urgency of surgery, ASA score, presence of malignancy, and diagnosis in predicting mortality in patients undergoing laparotomy. Although the ASAs classification of fitness for surgery was not devised as a risk assessment tool, it has been used for many years in most emergent surgical cases (Table 15.1: ASA Score). 27 In six studies observing mortality after emergency surgery in the elderly, increasing ASA grade was associated with increased mortality irrespective of age. This subjective and simple-to-calculate score has been shown to be a good estimate of mortality risk even in octogenarians.28
TABLE 15.1
ASA GRADE
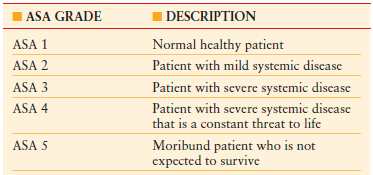
ASA, American Society of Anesthesiologists.
Modified from Owens WD, Felts JA, Spitznagel EL. ASA physical status classifications: a study of consistency ratings. Anesthesiology. 1978;49:239–243.
As stated, the prevalence of chronic disease is quite high in the elderly. The National Center for Health Statistics reported that 80% of Americans over age 65 live with one chronic medical condition and 50% have at least two.29 Chronic hypertension, arthritis, coronary heart disease, and diabetes are common. The management of these diseases requires medications (both prescription and over the counter), which further alter physiology and can affect a nontargeted organ. For example, NSAIDs can have deleterious effects on gastric mucosa, and beta-blockers can blunt a normal tachycardic response to hypovolemia. Thus, evaluation of the older patient with a surgical emergency is complex, and in many emergent cases complete preoperative assessment and risk stratification is impossible.
The current American College of Cardiology/American Heart Association (ACC/AHA) guidelines for cardiac risk stratification for patients undergoing noncardiac surgery can be used for preoperative assessment.30 While the guidelines are primarily focused on patients undergoing elective noncardiac surgery, the guidelines list a Class I recommendation for patients in need of emergency surgery. These patients should proceed to the operating room without extensive preoperative cardiac assessment, followed by subsequent perioperative surveillance and postoperative risk assessment and risk factor management. The basic clinical evaluation should include a careful history and physical examination, pertinent laboratory tests (complete blood count to assess for anemia, which can impose stress on the cardiovascular system), and ECG to aid in determining the presence of active cardiac conditions. In elective surgery patients, the presence of unstable coronary artery disease, severe hypertension, uncompensated heart failure, valvular disease, or severe arrhythmia would lead to delay in surgery. However, in the emergent setting, where the risk of delaying the surgery would affect mortality, maximal medical therapy is instituted, and the procedure is performed. Most emergent general surgery procedures include the abdomen and fall into the intermediate cardiac risk category (1%–5%), including cardiac death and nonfatal myocardial infarction (MI).
The most frequent cause of morbidity and mortality in the elderly surgical patient is underlying cardiovascular disease.14 Atrial fibrillation (AF) is the most common arrhythmia (1% of the general population over 60 years) and occurs in 5% of noncardiac surgical intensive care patients.31 Advanced age (over 60), higher Injury Severity Score in trauma and increased Simplified Acute Physiology Score II, as well as catecholamine use and fluid and transfusion therapy are major risk factors for AF.32 Patients who develop AF have considerably longer ICU length of stay, hospital length of stay, and higher mortality. Asymptomatic, hemodynamically stable patients can be treated pharmacologically with calcium channel blockers, beta-blockers, amiodarone, or digitalis to achieve either rate control or chemical cardioversion. Side effects of these medications are common. Electrical cardioversion is used for hemodynamically unstable patients or electively, often with cardiology consultation for patients with refractory AF.33
MI is the leading cause of postoperative death in patients over 80 years.14 Preexisting cardiovascular disease and postoperative stressors including emergence from anesthesia and major fluid shifts contribute to myocardial ischemia and infarction in the elderly. Most postoperative MIs occur in the first 72 hours after surgery, and many are “silent.” Thus, a high index of suspicion for cardiac ischemia must be present when an older patient presents with tachycardia, hemodynamic abnormalities, or chest pain. Initial management includes hemodynamic stabilization and support while addressing the underlying acute disease process, in addition to aspirin and heparin (where appropriate), beta-blockers, oxygen, and pain relief. Early cardiology consultation should be sought, particularly when coronary revascularization is beneficial.
The ACC/AHA guidelines of 2009 gave a class I recommendation that patients who were receiving beta-blockers on an outpatient basis be continued in the perioperative period.34 Initiation and titration of beta-blockers in the perioperative setting for patient undergoing noncardiac emergency general surgery (intermediate risk) is controversial and requires cardiac risk stratification and recommendations usually made by a cardiologist. Many elderly patients have undergone percutaneous coronary intervention (PCI) with or without stent(s) (bare-metal or drug-eluting). Most are on antiplatelet therapy in the periprocedure time frame or long term to prevent stent thrombosis and subsequent MI. The ACC/AHA guidelines recommend maintenance of patients on antiplatelet therapy in the perioperative period, especially if drug-eluting stents were used. If drug-eluting stents were placed within 1 year of presentation for emergent surgery, then dual antiplatelet therapy should be considered. Obviously, the bleeding risks versus antiplatelet and coronary protective benefits must be evaluated on a case-by-case basis.
Other situations arise in which treatment of chronic medical conditions with antiplatelets or anticoagulants is necessary, such as peripheral arterial disease, deep venous thrombosis (DVT), and AF. Aspirin irreversibly inhibits platelet activity for the lifetime of the platelet (~7–10 days). Clopidogrel, however, has a long half-life and will affect newly transfused platelets. Platelet transfusion is the classic modality of treatment for platelet-associated coagulopathy. Desmopressin or DDAVP has been described in treating uremic platelet–associated coagulopathy and aspirin-induced platelet dysfunction.35 Fresh plasma or fresh frozen plasma (FfP) has traditionally been used to reverse warfarin-induced coagulopathy. 10 mL/kg–15 mL/kg of FfP transfusion is often needed, which can result in as many as 4–6 units of plasma transfused (800–1200 mL).36 In elderly patients with limited cardiopulmonary reserve, pulmonary edema can result. Alternatives to FfP do exist. Vitamin K is usually administered via the intravenous route (5mg or 10 mg) in the bleeding patient with warfarin-induced coagulopathy. Intravenous Vitamin K produces a more rapid response but has been associated with anaphylaxis.37 Recombinant activated factor VIIa (rFVIIa) was initially described in the treatment of hemophilia and more recently has been used to treat moderate coagulopathy in traumatic brain injury.38,39 rFVIIa enhances the thrombin-generating potential of activated platelets and aids in the activation of thrombin-activated fibrinolytic inhibitor, which results in a stable hemostatic plug that is resistant to premature lysis. A single dose of rFVIIa has been shown to be safe and effective in this cohort. Prothrombin complex concentrates are derived from human plasma, undergo viral inactivation, and contain vitamin K-dependent coagulation factors (II, VII, IX, and X). In the acute setting, such as traumatic brain injury, prothrombin complex concentrates have been shown to be effective in elderly patients in decreasing time to reversal of international normalized ratio.40
Perioperative respiratory insufficiency and failure are common and the need for mechanical ventilation is common in the elderly.41 In addition, acute lung injury occurs more frequently with a higher mortality (60%) when compared to younger age groups.42 Recognition and aggressive management of chronic pulmonary disease, such as chronic obstructive pulmonary disease and asthma, can minimize postoperative respiratory complications. Attention to postoperative and postinjury pain control with patient-controlled analgesia and epidural anesthesia is beneficial to the elderly patient.43,44 Epidural or regional anesthesia promotes ambulation and provides excellent pain control while minimizing systemic opioids. In particular, patients over 65 years are susceptible to major complications after blunt thoracic trauma with even a few isolated rib fractures; mortality increases with increasing numbers of rib fractures in the elderly. Early use of mechanical ventilation that promotes spontaneous breathing and minimal barotrauma are the mainstays in management.
Specific Considerations
The common surgical emergencies in the older patient are injury and trauma, especially musculoskeletal, and diseases related to the abdomen, vascular insufficiency, and soft tissue infections.
Trauma The leading causes of nonfatal injury in older Americans are (1) falls, (2) pedestrian struck by automobiles, (3) MVC, and (4) violence.8 Falls have become the main cause of hospitalizations for the elderly.24 While younger adults tend to fall from heights (ladders), older adults fall from standing or sitting positions.45 Up to 6% of falls result in fractures, with 1%–2% of these being hip fractures.24 Pelvic fractures in the elderly have a higher risk of bleeding and of requiring interventional control.46 Age-related changes in vision, hearing, cognition, and reflexes contribute to the higher rate of MVC in the elderly, but different driving patterns lead to more MVCs during the day. Elders account for more than 20% of automobile-pedestrian fatalities.9 Violence is an unfortunate reality in the elderly, as older patients are more susceptible to unintentional injury and abuse.
The initial trauma evaluation and workup follow the principles of the Advanced Trauma Life Support (ATLS™) course with special attention to recognize preexisting medical conditions, chronic medications, and altered physiologic responses.47 In addition, while resuscitation is ongoing, contacting family, caregivers, or physicians for medical information, health status, medications, and advanced directives is important. A heightened suspicion for occult injury, blunted cardiovascular response, and potential for early deterioration is required. Early use of ultrasound, placement of invasive monitoring or echocardiography to determine volume status and cardiac performance is helpful. Pain control is essential but should be given in smaller interval doses. Establishment of baseline mental status is important and early brain CT is critical in all cases. An age-related approach to patient care is presented in Table 15.2: Age-Related Approach to Patient Care.
TABLE 15.2
AGE-RELATED APPROACH TO PATIENT CARE
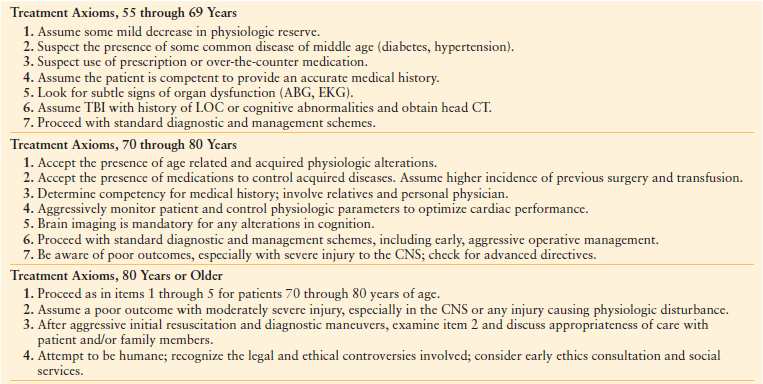
Modified from Schwab CW, Kauder DR. Trauma in the geriatric patient. Archives of Surgery, 1992;127:701–706. Copyright © (1992) American Medical Association. All rights reserved.
Abdomen While the incidence of peptic ulcer disease in decreasing in the general population, the incidence of hospitalization and mortality due to gastric and duodenal ulcer in the elderly remains high.48 This phenomenon can be attributed to the high prevalence of Helicobacter pylori infection and the increasing use of ulcerogenic medications, such as aspirin and NSAIDs. The treatment option for the management of perforated gastric ulcer begins with nonoperative measures, which include nasogastric decompression, analgesics, proton pump inhibitors, and appropriate antibiotics.49 Mortality approaches 5% for nonoperative management of perforated peptic ulcer; therefore, this approach is advocated with caution in those over age 70. Patient history and overall stability will determine if nonresectional surgery with omental patching is more appropriate than definitive acid-reducing operation.50,51 Recent studies have advocated the use of laparoscopic exploration, peritoneal lavage, and gastric or duodenal omental patching with excellent outcomes.52
Patients over age 80 with gallstone disease are more likely to present with obstructive jaundice or biliary colic.53 Nonoperative management has a high failure rate and mortality (17%). Laparoscopic and open cholecystectomy in patients over 80 years for complicated choledocholithiasis requiring endoscopic sphincterotomy is associated with increased morbidity and mortality.54 Failure to perform early cholecystectomy often leads to readmission with an increased percentage of those patients requiring open procedures. Thus, early laparoscopic cholecystectomy is the standard of care even in the face of a multitude of comorbidities.55 Percutaneous cholecystostomy with interval cholecystectomy remains an option in the acutely ill and septic patient.56
Small bowel obstruction is a common reason for emergency surgical admission. Postoperative adhesions are by far the most common etiology of small bowel obstruction, with hernia (internal and external), malignancy, and inflammatory bowel disease accounting for the rest.57,58 A high index of suspicion for necrotic bowel is necessary in the evaluation of the elderly patient with vague complaints and misleading signs and symptoms of abdominal pain, distention, and emesis. Delay in operation can result in loss of viable bowel and possible loss of life. The principles for fluid resuscitation with correction of electrolyte abnormalities, radiographic evaluation, and management are similar for younger patients with the caveat of performing laparotomy in cases without prompt improvement.
Colorectal emergencies are common in the elderly. In cases of bleeding, perforation, and obstruction, resection with creation of an ostomy is often the safest procedure. Emergency resection and primary anastomosis can be performed with an acceptable leak (6%) and mortality (9%) rates in the elderly who present with left-sided obstructing colorectal cancer, minimal soilage, and favorable physiology.59 Acute appendicitis presents late in the course and is more complicated and lethal.60,61 While abdominal CT is useful in the diagnosis of appendicitis and laparoscopic appendectomy has been shown to be beneficial in terms of improved postoperative pain, neither has affected outcome with respect to mortality in the elderly population.62–64 Early appendectomy remains the mainstay of treatment and the most effective means to avoid perforation, abscess formation, and sepsis. Interval appendectomy performed after a period of conservative management with antibiotics and percutaneous drainage for perforated appendicitis and periappendiceal abscess can be beneficial in adults.65 The prevalence of diverticular disease increases to 50%–70% in those over the age of 65.66 Chronic health conditions have been associated with poor outcomes in acute diverticulitis. Conservative management of acute noncomplicated diverticulitis with bowel rest, analgesia, and antibiotics are the initial treatment. Recurrent episodes are less well tolerated, and early resectional therapy should be considered. Surgery is reserved for abscess, perforation, or peritonitis.67
Hernias Elective repair of abdominal wall and groin hernias is one of the most common general surgical operations.68 Emergencies, including obstruction, incarceration, and strangulation are frequent. External hernia repair has a 5% overall mortality, and this is largely associated with bowel resection for necrosis.69–71 Other risk factors for unfavorable outcomes are advanced age, ASA class, coexistent disease, late presentation, and misdiagnosis. Older, stable patients who present with incarcerated body wall hernias should undergo attempts at manual reduction with appropriate sedation and analgesia as long as there are no signs of peritonitis or local cellulitis over the hernia. If reduction is successful, the patient should be observed in the hospital. If the patient develops abdominal pain, fever, tachycardia, or leukocytosis, emergent abdominal exploration to inspect the viscera and hernia repair should be completed. If attempted reduction fails or if the patient has signs or symptoms of strangulation or bowel necrosis, urgent operative intervention is necessary. If the peritoneal fluid is abnormal or the bowel is compromised, inadequately visualized, or reduces into the abdomen prior to inspection, full abdominal exploration is recommended for visceral inspection.
Vascular emergencies Mesenteric ischemia is uncommon but has a high mortality approaching 90%.72 The three primary etiologies are acute mesenteric ischemia (arterial embolism or thrombus), mesenteric vein thrombosis, and nonobstructive mesenteric ischemia (low flow state). It is essential to maintain a high index of suspicion in the elderly patient who presents with abdominal pain out of proportion to physical exam findings and a history of comorbidities consistent with vascular disease or cardiac dysrhythmia. While angiography remains the gold standard as a diagnostic and therapeutic tool in acute mesenteric ischemia, CT angiography (CTA) is more readily available and commonly used. CTA also gives information about mesenteric vein thrombosis, bowel wall thickening, and pneumatosis. Management focuses on volume resuscitation and broad-spectrum antibiotics followed by operative exploration to determine bowel viability, resection, second-look procedures, and occasionally damage control procedures.
Acute lower extremity ischemia is a common surgical emergency, and the early recognition of symptoms can lead to limb salvage. Patients commonly present within a few hours of the ischemic event with the 6 “Ps”: pain, pallor, paresthesias, paralysis, poikilothermia, and pulselessness (a late finding). A complete history and physical exam (with a detailed vascular pulse exam) will help elucidate the preexisting cardiovascular comorbidities that may have predisposed to the event, as well as the findings that identify the etiology of the event, that is, AF and embolus. The Rutherford Criteria have been used to grade the clinical severity of acute limb ischemia and are indicative of whether emergent surgical intervention is indicated and whether the limb is salvageable.73 Category II (sensory loss, possible muscle weakness, and inaudible arterial doppler signals) represents a threatened limb that is salvageable with immediate therapy, and in category III (profound sensory loss and muscle weakness and inaudible arterial and venous doppler signals), the patient has substantive disease with an unsalvageable limb that will require amputation. Imaging should examine both inflow and outflow anatomy. Arteriography is the gold standard with magnetic resonance angiography and CTA becoming more common. Initial therapy includes systemic heparinization followed by thrombolysis, mechanical thrombectomy, or open revascularization. Endovascular advances and interventional percutaneous techniques are now common, and early consultation with a vascular surgeon is recommended. In the elderly patient, especially with substantial comorbidity and limited activity level, amputation may be a better option than surgical revascularization.
Skin and Soft Tissue The presence of underlying skin conditions and chronic disease states, such as diabetes, place the elderly at high risk for skin and soft tissue infections.74 Necrotizing soft tissue infections (NSTI) are caused by microbial invasion of the subcutaneous tissues (SC) that occurs either through external trauma or direct spread from perforated viscus or urogenital organ.75 Most NSTIs are polymicrobial in nature and occur in the perineal and trunk area, often in immunocompromised patients, diabetics, and patients with peripheral vascular disease. Because of nonspecific findings and a variable time course to fulminant disease, a high index of suspicion must exist to diagnose NSTI expeditiously. Erythema, pain beyond the margins of erythema, woody induration of the soft tissues, and swelling are common findings. CT of the involved body region often demonstrates inflammatory changes, abscesses, and fascial edema. Laboratory findings are nonspecific and include elevated white blood cell count and hyponatremia. The gold standard in diagnosis is operative exploration with the findings of “dishwater” or foul-smelling discharge, necrosis, and loss of normal resistance of the fascia to finger dissection. The mainstay of therapy for NSTI is wide surgical debridement well beyond the rim of cellulitis.75 Prompt operation and adequacy of initial debridement are the most important determinants of survival. Broad-spectrum antibiotics are initiated and should include coverage for gram-positive, gram-negative, and anaerobic organisms. Antibiotic coverage for methicillin-resistant Staphylococcus aureus (MRSA) is also recommended. IV immune globulin and hyperbaric oxygen are additional therapies that have been described. Patients who survive NSTI have high morbidity, often necessitate multiple operations, and require prolonged ICU care. V.A.C. Therapy, nutritional support, and physical therapy are the additional mainstays of the long-term therapy. Outcomes in those over 70 years are poor.
Ethical and End-of-Life Issues
The primary objective of ICU care is to survive the acute threat to life. Success is achieved 75%–90% of the time, yet 20% of all deaths occur in the ICU.76 Most of these are older patients in their 8th, 9th, and 10th decades. The Society for Critical Care Medicine (SCCM) guidelines call for shared decision making between the health care team, the patient, and the patient’s family. Furthermore, even in cases of withdrawal or withholding of support, continued care and symptom management for dying patients is beneficial to both patient and family. Nearly 80% of the deaths that occur in the ICU occur after a decision has been made to limit life support measures (do not resuscitate or DNR).77 Most DNR decisions are made within the first week of ICU admission, and decisions to withdraw or withhold treatments are usually made around day 7. Older age, more severe illness or injury are associated with earlier end-of-life decisions. Advances in critical care medicine and technology have complicated decisions regarding futility and withholding or withdrawing of care. Critically ill patients who have decision-making capacity have the right to determine their level of care and treatment.78 When elderly patients are unable to participate in decision making, advanced directive and communication with family (next-of-kin, and power of attorney) must guide the health care team.
ACUTE CARE SURGERY AND PREGNANCY
Introduction
Caring for the pregnant woman presents a unique challenge to the acute care surgeon as there are two patients to manage: the mother and the fetus. The guiding management principle is that optimal care delivered to mother is the best initial treatment to the fetus. Often, managing the pregnant patient with a surgical emergency or critical injury is a multidisciplinary effort with input from the surgeon, obstetrician, anesthesiologist, and neonatologist.
Approximately 6%–7% of pregnancies are complicated by trauma, which is the leading nonobstetric cause of maternal death. The mechanisms of trauma for pregnant patients are most commonly motor vehicle collision (49%), fall (25%), and assault (18%). Penetrating trauma and burns comprise the minority of patients.79
General surgical procedures will be required in approximately 1 in 500 pregnant patients.80 The incidence of surgical diseases in the pregnant population is similar to the nonpregnant population. Presenting clinical patterns for these conditions are commonly the same for pregnant patients as for nonpregnant patients. However, expected anatomic and physiologic changes during pregnancy and the normal spectrum of symptoms associated with the pregnancy itself can make prompt diagnosis and management challenging.81 The section to follow will review the expected changes in pregnancy and the management approaches for the most commonly encountered acute care surgical scenarios.
Normal Physiologic Changes Associated with Pregnancy
Women undergo substantial physiologic changes as they progress through the trimesters of pregnancy. These changes involve virtually every organ system. It is essential for the acute care surgeon to be familiar with the nature of these normal changes to interpret a given patient’s physiologic status, diagnostic maneuvers, and clinical trajectory appropriately.
Intravascular Volume Volume expansion in pregnancy is profound and progresses throughout pregnancy until it plateaus at 32–34 weeks of gestation. The volume expansion occurs to maintain perfusion to organs and the growing uteroplacental interface. The larger plasma volume also prepares the mother for blood loss associated with giving birth. Total body water (TBW) increases by 4–5 L and is regulated by changes in the renin-angiotensin-aldosterone system, which results in increased sodium reabsorption and water retention. Most of the increased TBW is found in the fetus, placenta, and amniotic fluid. Maternal blood volume augmentation is comprised of increased plasma volume (1,200–1,300 mL) and increased red blood cell volume (300–400 mL). The much larger increase in plasma volume when compared to red blood cell volume explains why the normal hematocrit in late pregnancy is lower, 31%–35% (physiologic anemia of pregnancy). These changes allow an otherwise healthy pregnant patient to sustain blood loss volumes up to 1,500 mL before manifesting signs and symptoms of hypovolemia.82
Cardiovascular System Consistent with the increase in intravascular volume to maintain organ and fetal perfusion, the cardiovascular system undergoes changes to achieve the same goals. Cardiac output increases by 50% to 6 L/min in the first two trimesters of pregnancy, primarily due to an increase in stroke volume. An increase in heart rate also occurs gradually throughout pregnancy, contributing to augmented cardiac output, reaching 10–20 beats per minute faster by the third trimester.82,83
As pregnancy progresses, uterine blood flow increases to approximately 25% of the total maternal cardiac output at term. Because uteroplacental perfusion lacks autoregulatory mechanisms, fetal perfusion relies primarily on maternal mean arterial blood pressure (MAP). Accordingly, maneuvers that result in decreasing maternal MAP or cardiac output may compromise fetal perfusion. A patient in the supine position during the second half of pregnancy will have compression of the vena cava and impaired venous return causing a decrease in cardiac output to as much as 30%.82,83 Therefore, as a rule, all females in the second and third trimesters are positioned with the right side of the torso bumped up, shifting the weight of the uterus and fetus to the left. In addition, care should be taken when administering anesthesia of medications that can alter hemodynamics.
The hormone, progesterone, causes blood vessels to vasodilate. Coupled with the low resistance of the placental perfusion bed, systemic vascular resistance in pregnancy decreases by 15%. Resultant decreases in systolic and diastolic blood pressures by 5–15 mm Hg are observed by the end of the second trimester with a return to the prepregnancy range by term. Vasodilation also results in greater venous distensibility and higher venous pressures, particularly in the lower extremities.82
Physical findings associated with these cardiovascular changes of pregnancy include increased peripheral edema, mild tachycardia, jugular venous distension, and mild hypotension (depending on trimester). These expected changes in cardiovascular physiology warrant careful interpretation when evaluating a pregnant patient for emergency surgery.82
Pulmonary System Anatomical changes in the abdomen and chest wall account for a variety of changes in pulmonary mechanics during pregnancy. Resting lung volume decreases by 5% as the diaphragm elevates with displacement of the abdominal viscera by the enlarging uterus. Minute ventilation, the product of tidal volume and respiratory rate, increases in pregnancy by 30%–50%. The increase is primarily due to an increase in tidal volume as the respiratory rate in pregnancy is largely unchanged. This increase in minute ventilation results in a decrease in PaCO2 levels (40 mm Hg down to 32 mm Hg) and is believed to be due to the increased levels of progesterone, a respiratory stimulant. The lower baseline PaCO2 in pregnancy provides the necessary gradient to facilitate the transfer of carbon dioxide across the placenta from the fetal circulation to the maternal circulation for elimination.82,83
Oxygen demand increases during pregnancy because of the increased oxygen consumption of the maternal systems and the presence of the placenta and fetus. In total, these factors diminish maternal oxygen reserve. Difficult endotracheal intubation is a leading cause of morbidity and mortality in the pregnant patients. Airway edema and the generalized increase in BM of pregnancy contribute to airway obstruction and reduced glottis opening, and as such, smaller endotracheal tubes may be required.82
Renal System GFR increases as a result of the decreased vascular resistance and increased cardiac output. Alterations in sodium reabsorption result in water retention and plasma expansion. The higher GFR translates into decreased serum creatinine concentrations. It is important to consider the increased GFR during pregnancy to make appropriate adjustments to doses of medications cleared by the renal system. Glycosuria is a common finding during pregnancy.82,83
Anatomically, the collecting system dilates during pregnancy. This is mediated partially by the smooth muscle relaxing effect of progesterone. Also, the enlarging uterus compresses the distal ureters (right greater than left) in the pelvis, which also contributes to collecting system dilation. These expected findings should be noted and carefully interpreted on radiographic evaluation in the context of the patient’s clinical symptoms. The ensuing urine stasis predisposes pregnant women to urinary tract and renal infections as well as renal stones.82
Gastrointestinal System The main alterations in the gastrointestinal system are due to the enlarging uterus in the abdomen causing cephalad displacement of the abdominal and pelvic viscera and general relaxation of smooth muscle. Intraperitoneal structures shift in position, resulting in unusual presentations of common surgical conditions. Similarly, the operative approach for managing common surgical conditions may require adjustment in incision selection to account for the gravid uterus.82 Overall gastrointestinal motility and especially gastric emptying slow during pregnancy. The larger stomach volume and slower motility predispose pregnant women to aspiration when sedation is required during evaluation or management.82
Hematologic System As previously stated, the physiologic anemia of pregnancy is due to the proportionately larger increase in plasma volume compared to red blood cell volume. In addition to this dilutional anemia, iron stores are transferred to the fetus, a contributing factor to the anemia of pregnancy. Leukocytosis is observed during pregnancy and marked during labor that is endocrinologically mediated. This finding should not be mistaken for a marker of infection. Platelet counts remain relatively unchanged in pregnancy.82,83
The most noteworthy changes in the hematologic system during pregnancy involve the coagulation system. Essentially all procoagulant factors increase in pregnancy. Coupling this with a concomitant decrease in fibrinolysis puts the pregnant patient in a hypercoagulable state.82,83 The incidence of venous thromboembolic events including DVT and pulmonary embolism (PE) has been shown to be five times higher in pregnant patients.84 Following emergency surgery and trauma when additional factors of immobility, endothelial injury, and inflammatory mediators are exaggerated, the risk of DVT is even higher. As such, careful attention must be paid to DVT prophylaxis when managing pregnant patients, who often require pharmacologic prophylaxis.
Specific Considerations
Trauma The leading presenting mechanism of injury for the pregnant patient is blunt trauma after motor vehicle collision or fall.85 As with all trauma patients, the evaluation of the pregnant trauma patient follows ATLS™ protocol beginning with a primary survey to identify and address any life-threatening injuries. The expected changes of pregnancy must be carefully interpreted and managed in the context of the patient’s stage of pregnancy, mechanism of injury, signs, and symptoms. Foremost is the potential for a difficult airway, decreased oxygen reserves, and a full stomach. Substantial blood loss can occur before any changes in maternal hemodynamics are evident, manifesting first as fetal distress. Positioning the gravid patient in some degree of left lateral decubitus or manually displacing the uterus to the left side improves venous return by relieving pressure on the inferior vena cava.86 Early fetal assessment is essential as even if the mother’s vital signs are normal, the fetus may be inadequately perfused. Tocodynamometry and electronic fetal monitoring aids the diagnosis and treatment. Continuous monitoring is preferred and should be performed when the fetus is beyond 20–24 weeks.79 Approximate gestational age can be estimated by examination of fundal height with a fundus palpable at the umbilicus, corresponding to 20 weeks.87 Fetal viability is likely beyond 26 weeks gestation, and birth weight may have more impact than actual gestation age, with fetuses born <500 g less likely to survive.88
The following points are added in the care of the pregnant patient: palpation of the uterus for tenderness or contractions and pelvic examination to evaluate for fluid, bleeding, membrane integrity, and cervical status. Vaginal bleeding is concerning for abruptio placentae, which is the leading cause of fetal demise after maternal shock and death. Uterine rupture, though rare, is possible with considerable blunt trauma. Physical examination of the abdomen will reveal pain, palpable fetal anatomy and/or inability to palpate the uterus, or abnormal uterine shape or position.86
The secondary survey and appropriate adjunct diagnostic tests are employed to identify other injuries. The risk for potential harm to the fetus under 8 weeks gestation (during organogenesis) should not overshadow the necessity for radiographic imaging of the injured pregnant patient when there is need for accurate diagnosis. Radiation exposure of <0.1 Gy is considered safe; refer to Table 15.3: Absorbed Radiation Dose for radiation doses of specific imaging studies.87 Again, the best initial management of the fetus is the optimal resuscitation, diagnosis, and care of the mother linked to early fetal assessment.79,86
TABLE 15.3
ABSORBED RADIATION DOSE
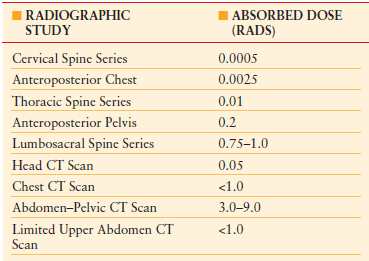
Modified from Tinkhoff G. Care of the Pregnant Trauma Patient. In Peitzman A, Rhodes M, Schwab CW, et al. eds. The Trauma Manual. 2008, 3rd ed. Philadelphia, PA: Lippincott, Williams & Wilkins Publishers.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








