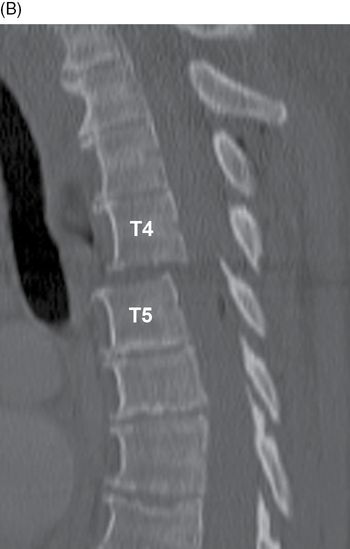
73-year-old woman in high-speed motor vehicle crash. Sagittal CT of the upper thoracic spine (left to right). There is retrolisthesis of T4 on T5 with widening of the facet joints (arrow) and widening of the anterior intervertebral disc space (arrowhead). There are multilevel underlying degenerative changes. This is a hyperextension fracture-dislocation injury. This injury is rare and usually grossly unstable. T4-T5 and T5-T6 constitute the most common locations for thoracic spine fracture-dislocations [1]. (Source: Chew FS. Skeletal Radiology: The Bare Bones. 3rd Edition. Copyright © 2010 by Felix Chew.)
Case 8–2
Thoracic spine fracture-dislocation T10-T11

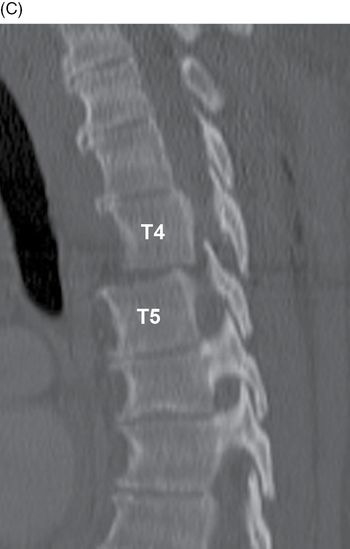
35-year-old man in high-speed motor vehicle crash. AP radiograph (A) and sagittal CT (B) of the lower thoracic spine. The AP radiograph shows gross lateral misalignment of the spine at T10-T11. The left eleventh rib has stayed with T10, while the right eleventh rib is fractured (arrow) but has stayed with T11, indicating the severity of the T11 fractures. The sagittal CT shows gross anterior dislocation of T10 over T11 and complete obliteration of the spinal canal. An anterior superior avulsion fragment of T11 has remained with T10 (arrowhead). The T10 spinous process (long arrow) has been avulsed. This is a flexion distraction injury. All three columns are disrupted, the anterior column on the compression side and the middle and posterior column on the tensile side. The ligamentum flavum, interspinous ligaments, and supraspinous ligaments are disrupted. When all three columns are disrupted from shear forces, dislocation can occur. The extent of translational injury or dislocation determines the degree of instability. In fracture-dislocations of the thoracic spine caused by flexion injury, the three main forces are axial compression, axial distraction, and translation. Compression and distraction may occur simultaneously at the opposite sides of the same level. Displacement of the spinal column, as seen in this case, indicates a translational component.
Case 8–3
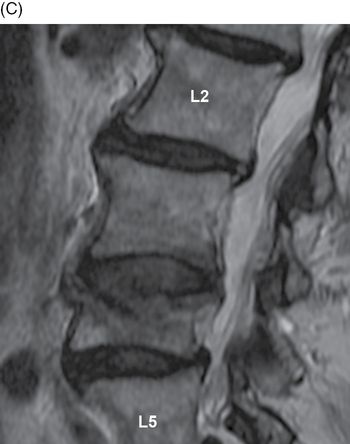
Hyperflexion injury T3-T4


45-year-old woman who crashed her motorcycle into a guardrail at 50 mph. Sagittal CT (A) of the upper thoracic spine and axial CT (B) of T4. There are fractures of T3 and T4. The T3 fracture involves the body and extends into the posterior elements, including the spinous process (arrowhead). The T4 fracture is a burst fracture that has resulted in loss of approximately 30% height and mild retropulsion. The T4 body is split into multiple fragments and the posterior elements are involved. There is a prevertebral hematoma (*) at T3-T4 displacing the esophagus.

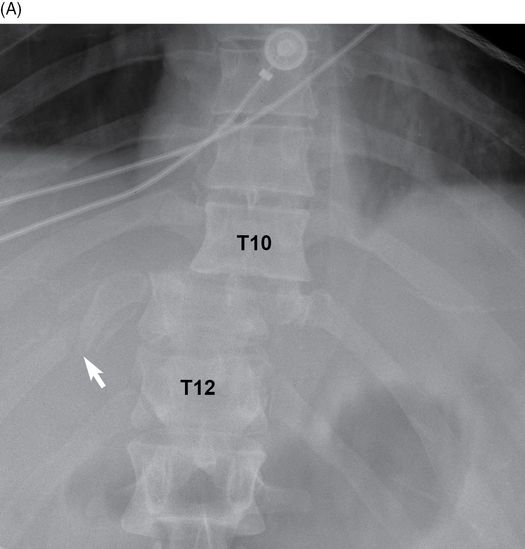
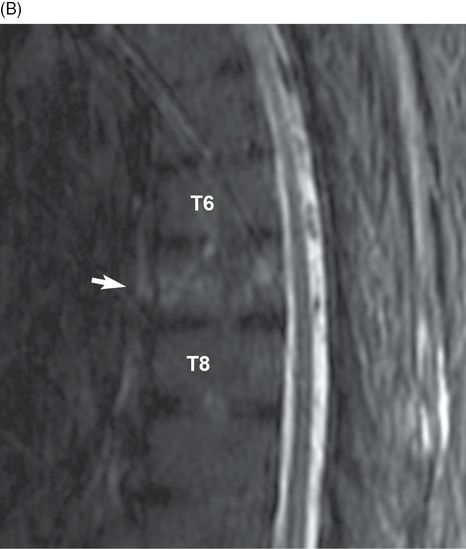
Sagittal T2 (C) and STIR (D) MRI of the upper thoracic spine. There is diffuse bone marrow edema within the vertebral bodies T3 and T4 with mild retropulsion. There is disruption of the anterior longitudinal ligament, posterior longitudinal ligament, and disc space of T3-T4, However, there is no cord edema. Robertson [2] compared spine injuries in motorcycles and cars and found thoracic spine injuries were more common in motorcyclists, whereas cervical spine injuries were more common in car occupants. The most common site of injury in motorcyclists was mid-thoracic, whereas the most common site in car occupants was upper cervical [2]. Thoracic spine injuries in motorcyclists occur with hyperflexion [3]. Axial loading is concentrated at the point of maximal flexion and results in injuries predominantly in the mid-thoracic spine (T4-T7), with T6 being the most common location [4].
Case 8–4
Fracture-dislocation T5-T6


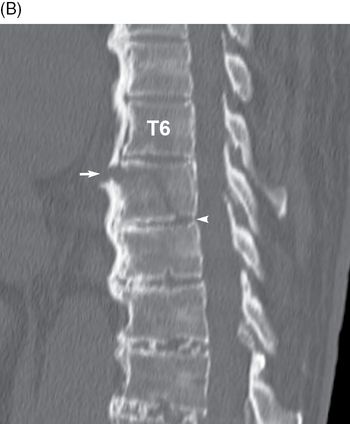
17-year-old woman who was ejected during a motor vehicle crash. Sagittal CT (A) of mid-thoracic spine and axial CT (B) at T6. There is anterior subluxation of T5 on T6 with compression fracture involving the superior endplate of T5 and compression fracture of T6 (arrow). There is a widely displaced spinous process fracture of T5 (arrowhead) that indicates a flexion-distraction mechanism of injury. There are also fractures of the spinous process of T3, T4, and T6. The spinal canal narrowing (*) caused by the anterior subluxation of T5 on T6 is concerning for transection of the cord, with spinal canal narrowing confirmed on the axial CT. There is prevertebral hematoma (long arrows). The patient had an ASIA A spinal cord injury at T5.


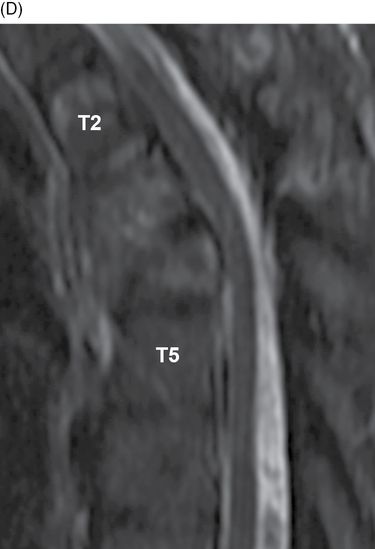
Sagittal T2 (C) and STIR (D) MRI of the mid-thoracic spine. There is anterior subluxation of T5 on T6 with disruption of the anterior longitudinal, posterior longitudinal, intraspinous, and interspinous ligaments. There is spinal cord edema. There is also hyper-intense signal within the paraspinal muscles from T4 to T7. Fracture-dislocation injuries result from compression and/or distraction forces combined with some degree of shear or rotation [5]. These injuries are unstable and have the highest incidence of complete neurologic injury of any of the thoracolumbar injury patterns [5]. The most common location is the thoracolumbar junction. Pickett et al. [6] looked at spinal cord injuries in Canada between 1997 and 2001 and found the most common cause of spinal cord injuries was motor vehicle collisions, whereas the second most common cause was falls. Car crashes were more frequently seen in younger patients, whereas ground-level falls were more frequently seen in elderly patients. Complete spinal cord injuries were most closely associated with burst fractures and bilateral facet fracture-dislocations [7]. A recent study of patients with thoracic and lumbar spine injuries from motor vehicle collisions from the Crash Injury Research and Engineering Network (CIREN) database identified 57.5% of the injuries with compression fractures, 24.9% with burst fractures, 8.8% with flexion-distraction injuries, 2.4% with flexion-dislocation injuries, and 6.4% with extension injuries [8].
Case 8–5
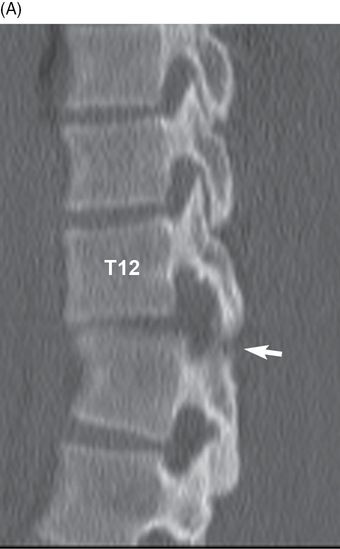
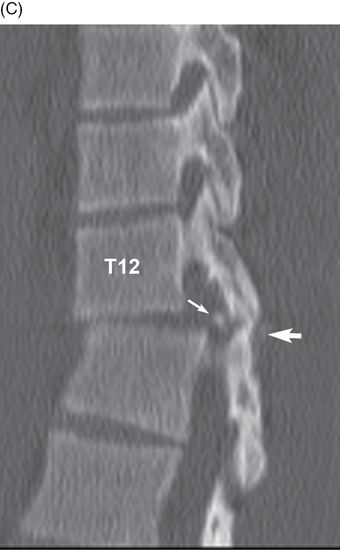
Compression fracture T12

44-year-old man whose motorcycle collided at high speed with a deer. Sagittal CT of the thoracolumbar junction. There is a wedge compression fracture at the superior endplate body of T12 (arrow). The posterior elements are not distracted, and there is no translation of T12 over L1.
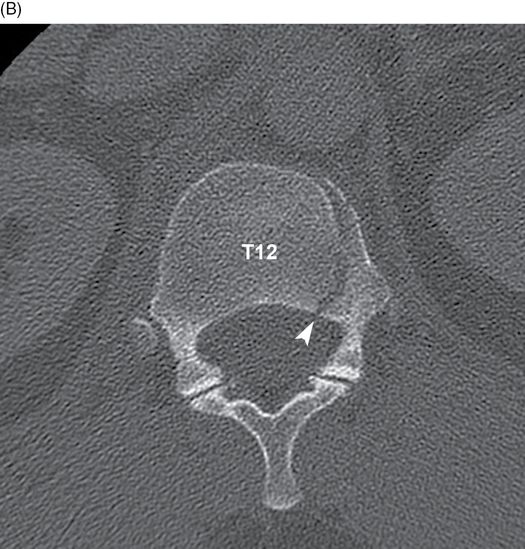

Axial CT at T12, superior (B) and inferior (C). A wedge compression fracture can be seen along the left lateral aspect of the superior endplate of T12 (arrowheads). There are comminuted fractures involving the right costovertebral junction, right twelfth rib, right pedicle, and right lamina. No translational component is present and the spinal canal is patient and unobstructed. This is likely an axial compression injury in which the vertebral body failed on the left and the posterior elements failed on the right.
Case 8–6
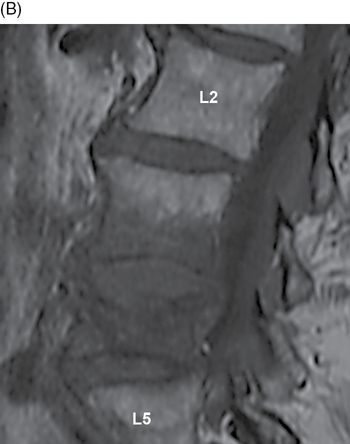
Hyperflexion fracture-dislocation T9-T10

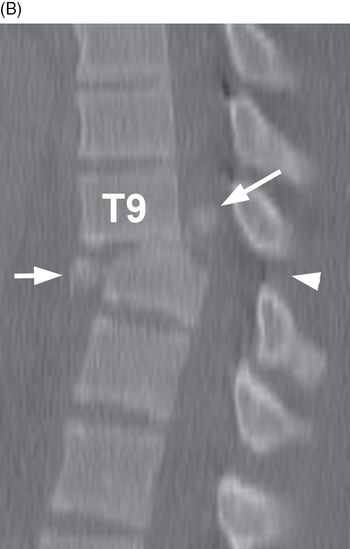
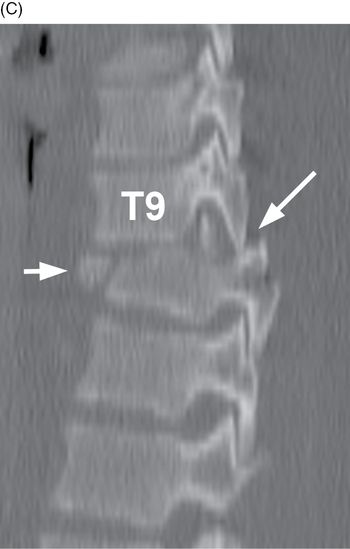
17-year-old man who was ejected from his vehicle during a motor vehicle collision. He was unrestrained. Sagittal CT of the lower thoracic spine, right (A) to left (C). There is a comminuted burst fracture of the T10 vertebral body (short arrows) with retropulsion of fragments. The fracture extends through the posterior elements (arrowheads). There is anterolisthesis of T9 over T10, and focal kyphosis. The retropulsed fragment (long arrow) occupies the spinal canal and the patient has a complete spinal cord transection. These injuries are consistent with a hyperflexion fracture-dislocation pattern. The posterior column fails under tension while the anterior and middle columns fail under compression. (Source: Chew FS. Skeletal Radiology: The Bare Bones. 3rd Edition. Copyright © 2010 by Felix Chew.)
Case 8–7
Distraction/shearing injury T11-T12

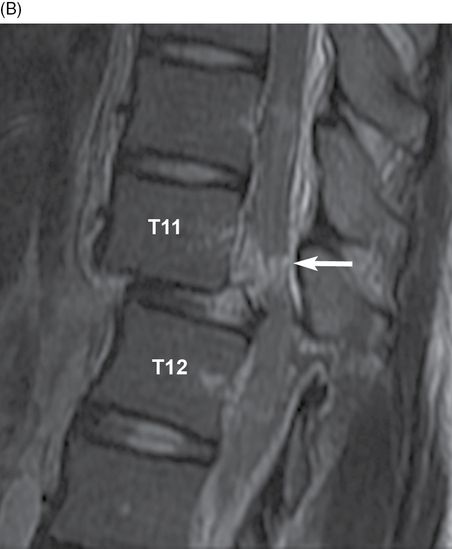
19-year-old man who crashed his car into a telephone pole that then fell onto his vehicle. Sagittal CT (A) and T2 MRI (B) of the lower thoracic spine. There is anterior translation of T11 over T12. The anterior disc space of T11-T12 is narrowed, while their spinous processes are splayed apart (short arrow). There is a small avulsion fracture of the posterior inferior margin of the T11 body (arrowhead). There is extensive edema and hemorrhage in the spinal cord (long arrow).

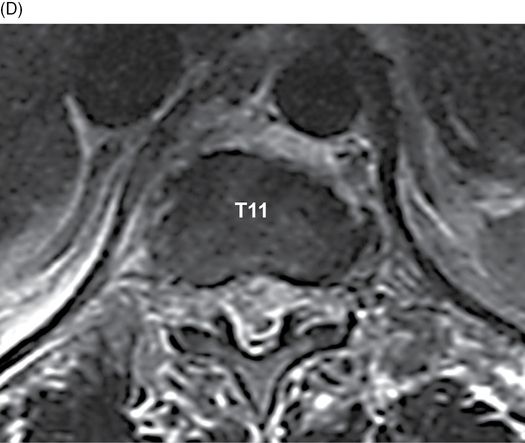
Axial CT (C) and T2 MRI (D) at T11. There is disruption of the anterior and posterior longitudinal ligaments as well as hyper-intense signal within the spinal cord at the level of T11. There was also hemorrhage at the level of the transection, which is not well visualized on these images. In a study of 100 patients with thoracolumbar spine fractures, Hsu et al. demonstrated that imaging was required in patients with high-energy injuries who met any of the following criteria: back pain/midline tenderness, local signs of thoracolumbar spine injuries, abnormal neurologic signs, cervical spine fractures, GCS less than 15, major distracting injury, and ETOH/drug intoxication [9]. In a study of 407 trauma patients in Korea, of which 123 were intoxicated and 284 were not, there was no significant correlation between alcohol consumption and spine injury severity although head and face injuries appeared worse [10]. Cord transection is evident on T2 MRI as interruption of the normal low-signal intensity of the cord. Frequently, a post-traumatic syrinx will develop months or years after the injury to the spinal cord. This begins as myelomalacia, which represents a softening of the cord as a result of the injury, eventually coalescing to form larger cyst or syrinx. However, it is important to distinguish myelomalacia from syrinx, as the syrinx can be shunted to restore neurologic function, but the myelomalacia cannot be shunted and does not respond to surgery. Spinal cord atrophy may also occur [11].
Case 8–8
Diffuse idiopathic skeletal hyperostosis with fracture T7


82-year-old man injured in ground-level fall. Sagittal CT of the mid-thoracic spine, right (A) to left (C). There is diffuse idiopathic skeletal hyperostosis (DISH) with flowing ossification of the anterior longitudinal ligament bridging the vertebral bodies at multiple contiguous levels. The intervertebral disc spaces are not narrowed, although several are calcified. At T6-T7, there is a horizontal fracture through bridging phytes (arrows) that extends in the axial plane through the T7 vertebral body, just inferior to the superior endplate, and then passes in the coronal plane to the posterior portion of T7-T8 disc space (arrowhead). There is mild lordotic angulation at the fracture site, in keeping with an extension mechanism of injury. The posterior elements are intact, and the facet joints are not ankylosed. This patient also sustained a C7 fracture (not shown). Spine fractures through DISH were first described in the cervical region [12] and later described in the thoracic region [13]. Rigidity of the spine predisposes it to fracture with minimal trauma, usually by hyperextension mechanism. Associated neurologic injuries are common.
Case 8–9
Ankylosing spondylitis with fracture T7

86-year-old man fell backward down the stairs. Sagittal CT of the mid-thoracic spine. There is a non-displaced fracture line through the vertebral body of T7 (arrow). There is diffuse osteopenia throughout the thoracic spine. There is ossification of the spinal ligaments, joints, and discs at multiple levels. There is no evidence of retropulsion or narrowing of the spinal canal.
Sagittal T2 MRI of the mid-thoracic spine. There is diffuse bone marrow edema and fracture through the vertebral body of T7 (arrow). There is no spinal cord edema. Fractures of the ankylosed spine can occur with minor trauma owing to rigidity and osteoporosis [14–15]. One study found the prevalence of vertebral fractures among patients with ankylosing spondylitis to be approximately 19% [16]. The incidence of spinal cord injury in spine trauma patients with underlying ankylosing spondylitis is 2% [17]. Caron et al. [18] found a 32% mortality rate following a traumatic fracture through an ankylosed spine (including both ankylosing spondylitis and DISH).
Case 8–10
Chance fracture L1



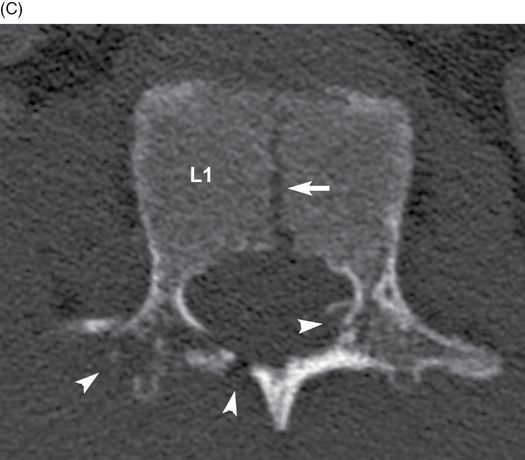
17-year-old man who fell from a 30-foot height and landed upright on his buttocks. Sagittal CT of the thoracolumbar junction, right (A) to left (C). There is a fracture in the axial plane extending through the L1 vertebral body (long arrows) and pedicles and into the spinous process (short arrows). There is mild focal kyphosis with minimal anterior wedging of the vertebral body. There is a mild compression fracture of the anterior superior corner of the L2 vertebral body (arrowhead). The Chance fracture pattern is caused by flexion-distraction without compression [19]. It is a horizontal fracture through the vertebral body and posterior elements, typically sustained in motor vehicle crash with a lap belt (but neither shoulder belt, nor airbag). It has been described as a fulcrum fracture because the seat belt acts as a fulcrum and absorbs the flexion or compression force and the spine, being posterior to the fulcrum, sustains the tensile forces through all its columns, thereby making it a distraction injury [20–21]. In a conventional flexion distraction type injury, the anterior column of the spine acts as the fulcrum and absorbs the compressive forces that leads to significant anterior wedging, a finding that is not typically seen with Chance fractures.
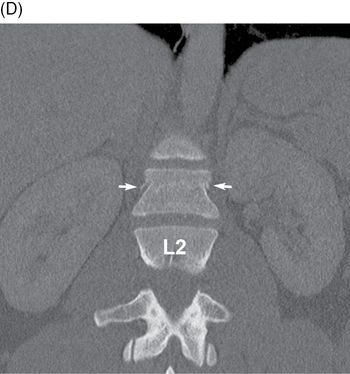
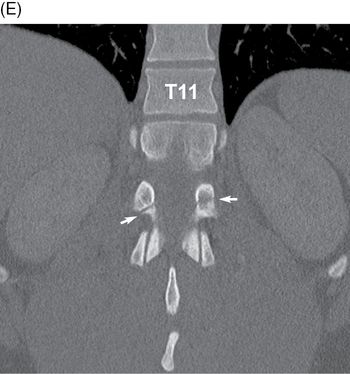
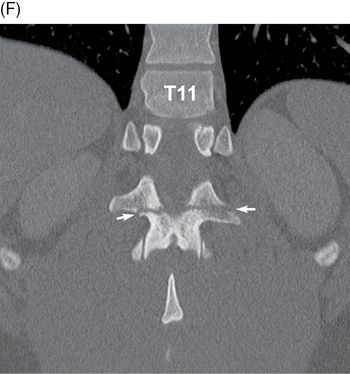
Coronal CT of the thoracolumbar junction, anterior (D) to posterior (F). Three patterns are seen with Chance fractures and variants. One involves disruption of the posterior ligaments and facet joints and posterior disc. Another involves a horizontal fracture through the posterior elements. The third is a horizontal fracture that dissects through the posterior elements and vertebral body. When a compression deformity occurs it is confined to the anterior superior part of the vertebral body. Associated bowel, pancreas, and mesenteric injury can be seen 15–20% of the time [21].
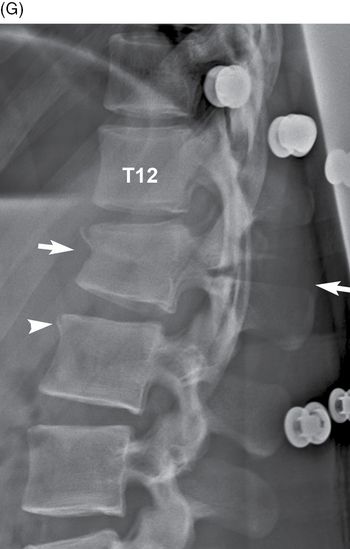
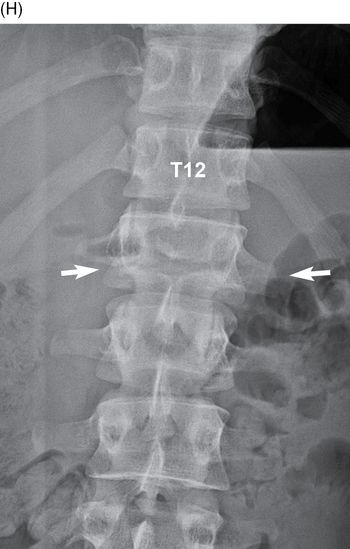
Lateral (G) and AP (H) radiographs of the thoracolumbar junction. The patient has been mobilized and is wearing a brace. The fracture plane (arrows) extends through the body and posterior elements of L1, with minimal impaction anteriorly and persistent distraction posteriorly. The fracture at the anterior superior corner of the L2 body is visible (arrowhead).
Case 8–11
Chance fracture L1


23-year-old man who rolled his car into a ditch. Sagittal CT (A) and T2 MRI (B) of the thoracolumbar junction. There is a horizontally oriented fracture through the vertebral body of L1 with loss of approximately 50% height (arrow) with fractures extending into the right pedicle, lamina, and spinous process (arrowhead). MRI shows the L1 vertebral body fracture (arrow) and marrow edema within the vertebral body. There is extensive edema in the posterior elements and posterior paraspinal soft tissue, including the interspinous ligaments (*).
Axial CT at L1. There is a fracture of the vertebral body, right pedicle, lamina, and spinous process of L1. No retropulsion is identified. The Chance fracture was first described by Q. Chance in 1948 [19], but it was not until 1965 that Howland et al. related these fractures to use of lap belts during motor vehicle accidents [22]. The most common locations are between T11 and L2. However, with the advent of the three-point safety belts in the late 1960s, seat belt injuries became less common [23]. The indications for surgery include ligamentous involvement of the posterior column or initial kyphotic angulation more than 15 degrees [24–26].
Case 8–12
Thoracolumbar flexion-distraction injury

35-year-old man injured on a construction site when he fell 12 feet while inspecting a pipe. Sagittal CT of the thoracolumbar junction, right (A) to left (C). On both the right and the left, the facet joints at T12-L1 are perched (short arrows), with distraction evident between the spinous processes in the midline (arrowheads). There is a small posterior element fracture fragment visible on the right side within the neural foramen. There is mild compression of the superior endplate of L1 (long arrows) with narrowing of the intervertebral disc space anteriorly. There is anterolisthesis of T11 over L1 (*), mildly compromising the spinal canal. There is a mild kyphosis at the T12-L1 level.
Case 8–13
Superior endplate compression fracture T12


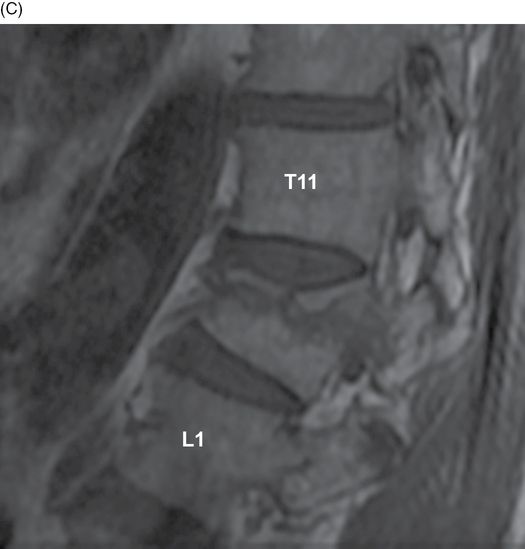
68-year-old man injured when an all-terrain vehicle fell on top of him. Sagittal CT (A) and STIR (B) and T1 (C) MRI of the thoracolumbar junction. There is a compression fracture of the superior endplate of T12 with approximately 30–40% loss of height. No retropulsion is identified. MRI demonstrates compression fracture of the superior endplate of T12 with high bone marrow signal, consistent with bone marrow edema in an acute fracture. There is no associated posterior distraction injury. This patient had no neurologic deficit. Anterior wedge compression fractures account for almost 50% of all thoracolumbar fractures [7]. The mechanism of injury typically involves axial loading with or without an element of flexion. The two populations that are commonly associated with compression fractures are trauma patients and osteoporosis patients. Compression fractures primarily involve the anterior cortex and retropulsion is infrequent. The fracture is often not well visualized on axial CT images because the axial plane is parallel to the fracture line. However, the fracture should be clearly seen on the sagittal and coronal reformatted CT images. On MRI, vertebral body bone marrow edema should suggest an acute fracture.
Case 8–14
Compression fractures of multiple vertebral bodies

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








