Fig. 15.1
Anatomy of the deep cervical plexus (With permission from Danilo Jankovic)
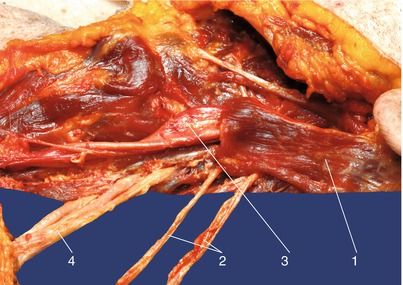
Fig. 15.2
Deep cervical plexus on the level of the C3, C4. (1) Sternocleidomastoid muscle (dissected), (2) deep cervical plexus from C3 and C4, (3) common carotid artery, and (4) trunks of the brachial plexus (With permission fom Danilo Jankovic)
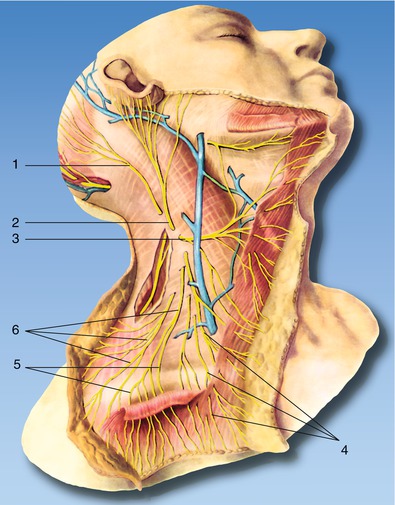
Fig. 15.3
Anatomy of the superficial cervical plexus. (1) Lesser occipital nerve, (2) great auricular nerve, (3) transverse cervical (colli) nerve, (4)medial supraclavicular nerves, (5) intermediate supraclavicular nerves, and (6) lateral supraclavicular nerves (With permission from Danilo Jankovic)
The muscular branches of the cervical plexus include segmentally arranged nerve branches supplying the deeper anterior neck muscles (the rectus capitis anterior and lateralis, longus colli, longus capitis and intertransverse, scalenus anterior and medius, and levator scapulae), as well as the inferior descending cervical nerve, the trapezius branch, and the phrenic nerve. The inferior descending cervical nerve (from C2 and C4) gives off several fibers to the carotid and jugular neural plexus and joins with the superior descending cervical nerve to form the ansa cervicalis. The area supplied includes the sternothyroid muscle, sternocleidomastoid muscle, thyrohyoid muscle, geniohyoid muscle, and omohyoid muscle.
The trapezius branch appears at the surface just below the accessory nerve and passes to the trapezius muscle. The phrenic nerve (from C4 and C3/5) is the motor nerve for the diaphragm, but it also contains sensory and sympathetic fibers that supply the fibrous pericardium, the mediastinal pleura, and the central part of the diaphragmatic pleura as the nerve courses through the thorax. Connections have been described between the phrenic nerve (left or right branch) or the phrenic plexus and the following structures: inferior and middle cervical ganglion, subclavian plexus, pulmonary plexus, inferior vena cava, esophagogastric junction, cardiac end of the stomach, hepatic portal, suprarenal cortex, etc.
Block of the Superficial Cervical Plexus
Indications
1.
Superficial procedure for submandibular, postauricular, and lower neck area
2.
Combined with deep cervical plexus block for surgical procedures listed below
3.
Isolated nerve (supraclavicular nerve) block adjunct to brachial plexus block for shoulder surgery
Procedure
With ultrasound, the typical morphology of cervical transverse processes from C2 to C7 can be easily revealed (Fig. 15.4a–g). At the level of C4 or C5, the superficial cervical plexus can be seen deep to the sternocleidomastoid muscle (Fig. 15.5). Both the in-plane and out-of-plane approaches can be performed, and a total of 5 mL of local anesthetic will be sufficient.
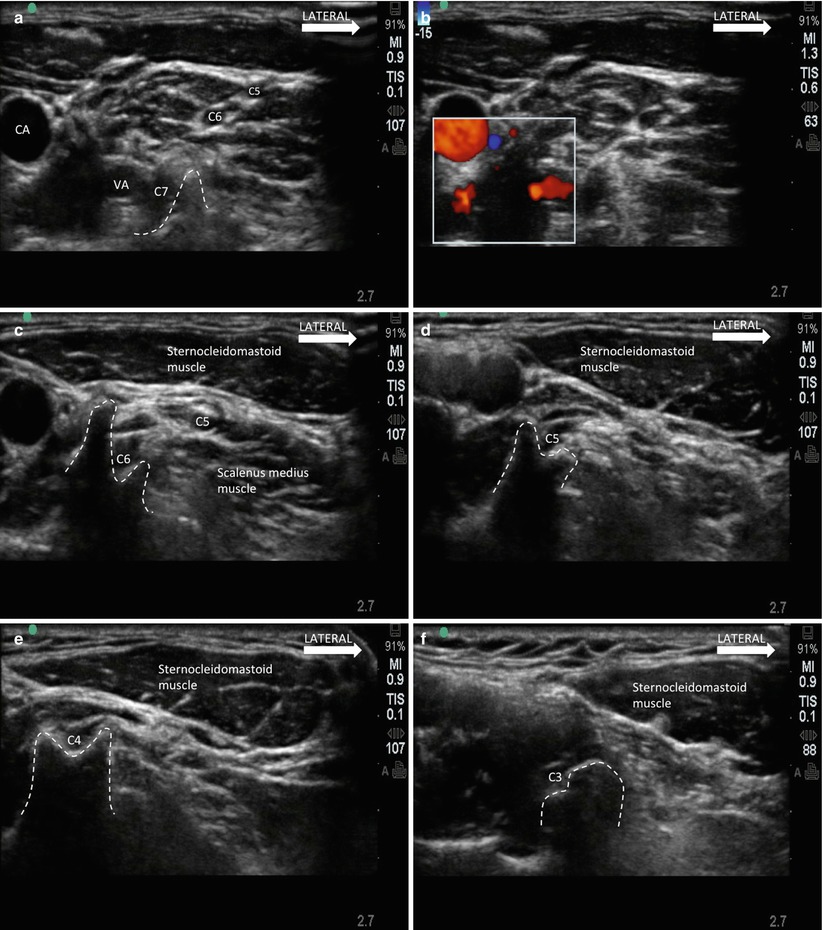
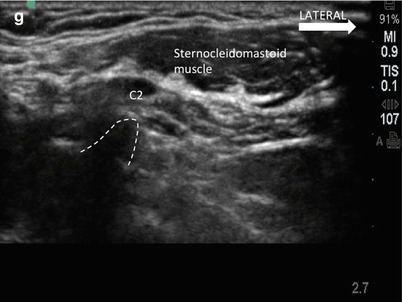
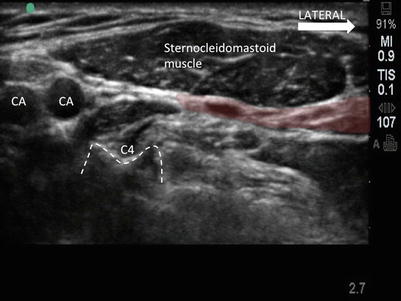
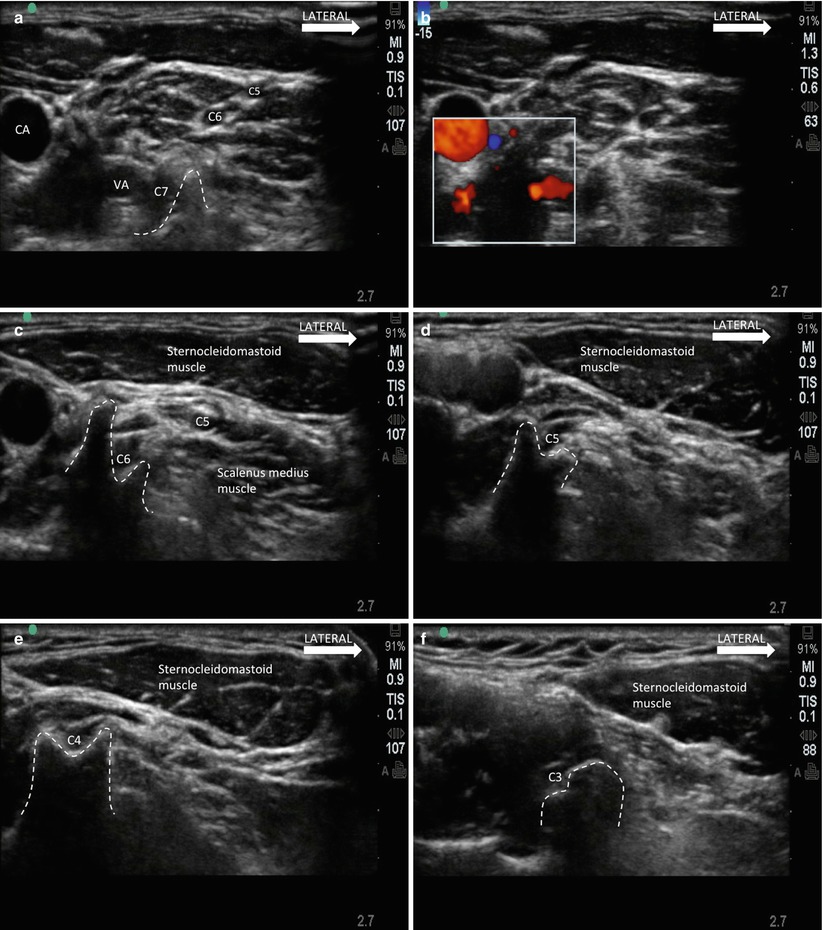
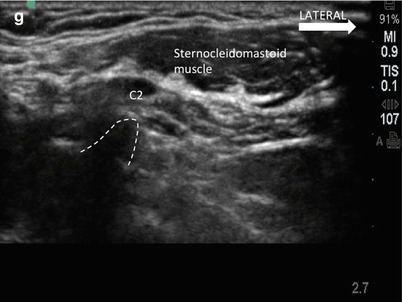
Fig. 15.4
(a) Sonogram showing transverse process of C7. Note that only the posterior tubercle is seen as the anterior tubercle is usually vestigial. The nerve roots C5 to C7 are seen aligned in the interscalene groove. The vertebral artery (VA) and carotid artery (CA) is seen in this sonogram and better shown in Doppler in (b). (c) Sonogram showing the transverse process of C6. Note the prominent anterior tubercle of C6. (d) Sonogram showing C5. Note the anterior and posterior tubercles are similar in size, contrast to that in C6. (e) Sonogram of C4. Note the morphology is similar to C5 but the tubercles are usually closer together than that of C5. (f) Sonogram of C3. Note the discrepancy in the shape of anterior and posterior tubercle. (g) Sonogram of C2. Note the prominence of the posterior tubercle (Reproduced with permission from Philip Peng Education Series)
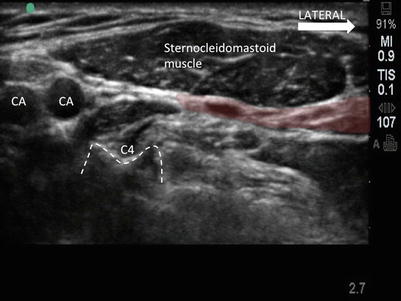
Fig. 15.5
Sonogram of the superficial cervical plexus (shaded with purple color) at the level of C4. Multiple nerves in short axis are seen sequestered in this space deep to the sternocleidomastoid muscle. CA, carotid artery, which bifurcates into internal and external carotid arteries (Reproduced with permission from Philip Peng Education Series)
For the clavicle, blockade of the supraclavicular nerve of the superficial plexus is possible. The anatomical landmark is the supraclavicular area 2–3 cm above the clavicle, posterior to the sternocleidomastoid muscle superficial to the deep cervical investing fascia (Fig. 15.6). The nerve usually appears as a single nerve trunk before it branches into medial, intermediate, and lateral branches and is in intimate relation to the external jugular vein. To inject this nerve, only 2 mL of local anesthetic is sufficient.
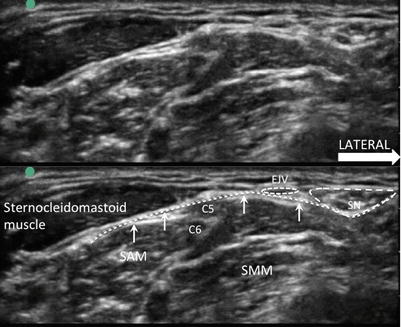
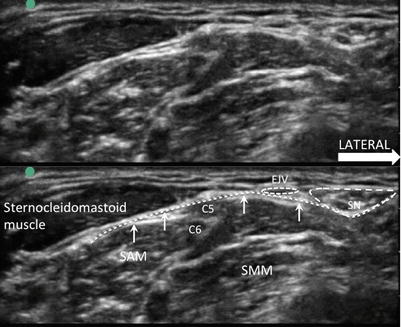
Fig. 15.6
Sonogram of the supraclavicular nerve (SN). The top picture is the unlabeled version of the bottom picture. Note the investing layer of the deep cervical fascia (dotted line indicated by arrows). The SN is superficial to this layer and is in close proximity with external jugular vein (EJV). SAM scalenus anterior muscle, SMM scalenus medius muscle (Reproduced with permission from Philip Peng Education Series)
Block of the Deep Cervical Plexus
Indications
Diagnostic
Localization and differentiation of various types of neuralgia
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








