This chapter provides recommendations on the ICU care of Ebola virus disease in resource-rich environments. Prior to the 2014–2015 West African Ebola outbreak, the disease was thought to be nearly universally fatal. Recent clinical experience in West African nations, the United States, and Europe have shown that with aggressive supportive care, many patients infected with Ebola are able to make a complete recovery. In 2014, a small number of hospitals in the United States gained experience in the care of patients with Ebola primarily as a result of repatriation of U.S. citizens who contracted the disease in West Africa. The primary source of information in this chapter is the clinical experience of the Biocontainment Unit (BCU) at the University of Nebraska Medical Center (UNMC), where three patients received comprehensive care for confirmed Ebola virus disease.
I. BACKGROUND ON EBOLA VIRUS / 2014 OUTBREAK
A. Ebola virus disease (EVD) is an infectious disease caused by the Ebola virus of the Filoviridae family. The Ebola virus is most likely animal-borne, with bats as the likely reservoir. Humans contract Ebola through direct contact with the body fluids of a person or animal that is sick with or has died from Ebola or from contact with an object contaminated with infected fluid.
B. Ebola was discovered in 1976 in what is now the Democratic Republic of the Congo. A few small outbreaks of EVD have occurred in Africa since 1976, and in 2014 a large epidemic began in Liberia, Guinea, and Sierra Leone.
C. The 2014 West African Ebola epidemic was the largest of all time and resulted in more than 27,000 cases and more than 11,000 deaths.
II. COLLABORATIVE CARE: Optimal care of the patient with EVD requires intense collaboration by multiple teams.
A. Strategic Planning by the leadership of the following teams is essential: infectious disease, critical care, emergency medicine, hospital administration, nursing, clinical laboratory, respiratory care, infection control, pharmacy, radiology, clinical research, media relations, security, and public health departments.
B. An Infectious Disease specialist and a Critical Care physician should be clearly identified as the attending physicians responsible for the overall care of a patient with EVD.
III. DIAGNOSIS OF EVD requires a high index of suspicion on the part of the clinician.
A. Identification of Patients at Risk for EVD involves analysis of the following:
1. Recent travel to areas with active EVD (e.g., West Africa in 2014–2015) or known contact with EVD.
2. History and physical findings may include fever, headache, myalgias, fatigue, diarrhea, emesis, abdominal pain, unexplained bleeding, or bruising. It is notable that in the 2014 outbreak, EVD was rarely associated with bleeding despite its former name “Ebola hemorrhagic fever.”
B. The diagnostic workup for detection of Ebola should be directed by an infectious disease specialist and the public health authorities at the local, state, and federal levels.
1. Assays for Ebola include ELISA, PCR, IgG, and IgM analyses. Optimal testing depends on timing and clinical situation.
C. A Differential Diagnosis must be constructed, as the vast majority of patients with these signs and symptoms have a disease other than EVD. Routine diagnostic testing for other possible diseases (e.g., malaria) should not be delayed for persons under investigation for EVD.
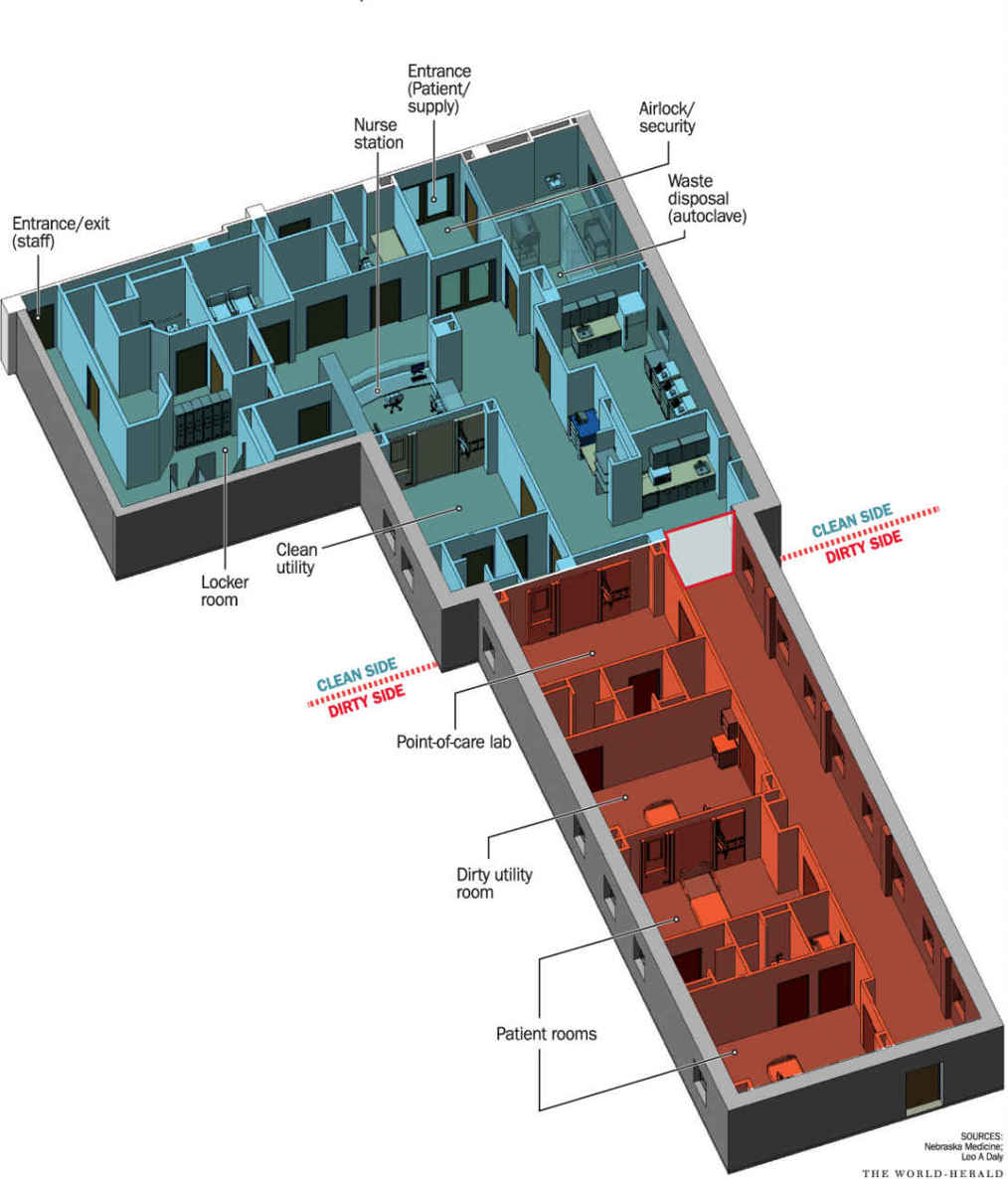
IV. FACILITIES: The care of a patient with EVD requires a significant amount of dedicated physical space capable of enabling full critical care services. While most hospitals lack a prededicated BCU, space can be created within an existing ICU provided that other patients can be located elsewhere and traffic within that ICU can be strictly controlled (Fig. 13.1).
A. At Least Four Rooms are needed to provide care for an individual with EVD:
1. A private isolation room for the patient
2. A room for the storage of clean supplies and personal protective equipment (PPE). The following equipment should be dedicated to the unit (most equipment can be safely decontaminated by special cleaning procedures): portable X-ray, ultrasound machine, code blue cart, and an airway cart with a video laryngoscope.
3. A room for point-of-care laboratory testing
4. A room for the processing of contaminated supplies and equipment
B. Video and Audio Monitoring between the patient room and the nurses station is very useful as it allows clinicians and family members to observe the patient without coming into direct contact.
1. To minimize exposure, one physician can examine the patient and call out physical findings while a colleague remains at the video monitor to act as a scribe.
2. Frequent video and audio contact between the patient and family members are helpful for both as they endure the stress of battling a high-mortality illness.
V. The initial workup of a patient with confirmed EVD should include a comprehensive metabolic panel, calcium, magnesium, phosphorus, complete blood count with differential, PT-INR, PTT, fibrinogen, blood culture (aerobic and anaerobic), venous blood gas, portable chest X-ray, 12-lead EKG, and blood type. A complete antibody screen creates a high risk for splash exposure and thus should be omitted.
A. Laboratory testing should be performed with point-of-care equipment whenever possible. Any laboratory samples removed from the immediate patient care area must be handled with extreme caution so as to minimize the risk of transmission to a health care worker or to another patient. Extensive coordination with directors of clinical laboratories is necessary for optimal and timely utilization of laboratory tests.
B. Point-of-care ultrasonography can be especially helpful in the care of patients with EVD, as advanced imaging modalities such as CT and MRI are unavailable. Bedside ultrasonography can be used to assess for cardiac function, volume status, extravascular lung water, pleural effusion, atelectasis, pneumonia, abdominal fluid, and deep venous thrombosis, in addition to guidance for invasive procedures such as central venous and arterial line placement. A standard ICU ultrasound system can be successfully decontaminated after use on a patient with EVD.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree