Complications of The Beach Chair Position
Robert R. Kirby
David J. Cullen
CASE SUMMARY
A 61-year-old, American Society of Anesthesiologists physical status classification I (ASA I), male patient underwent general anesthesia for repair of a torn rotator cuff in his right shoulder. After induction of anesthesia, he was placed in an upright, 60 to 65 degree, modified beach chair position. Throughout the 2 hour and 20-minute operation, his blood pressure was measured noninvasively by a cuff placed on his left arm, varying from 130/50 to 90/55 mmHg. Pulse oximeter readings were 97% or above, and his partial pressure of end-tidal carbon dioxide ranged from 30 mmHg to 38 mm Hg. Blood loss was minimal, and urine output was not measured.
At the end of the case, he was extubated in the operating room and transported to the postanesthesia care unit (PACU). The PACU nurse listed him as comatose with no activity, no consciousness, and an Aldrete score1 of 4/10. Seven hours later, the patient had not regained consciousness and was transferred to the intensive care unit. During the interval, he exhibited withdrawal one time to the application of a peripheral nerve stimulator. Otherwise, he was stated to be unresponsive and/or unarousable on at least six occasions.
A noncontrast computerized tomography scan showed no significant abnormalities. The following day magnetic resonance imaging (MRI) and magnetic resonance angiography were unremarkable. Four days later, a repeat MRI showed bilateral cortical ischemia and infarction, right basal ganglion infarct, effacement of right cortical sulci, and compression of the right lateral ventricle. Magnetic resonance angiography remained unremarkable. Eight days later, MRI revealed extensive cortical injury, infarction of the right and left heads of the caudate nuclei and the right lenticular nucleus, cortical laminar necrosis, and Wallerian degeneration on the right side. Magnetic resonance angiography showed little, if any, change. Subsequently, he was transferred to a rehabilitation center and later to a chronic care facility in a persistent vegetative state.
What Is the Beach Chair Position?
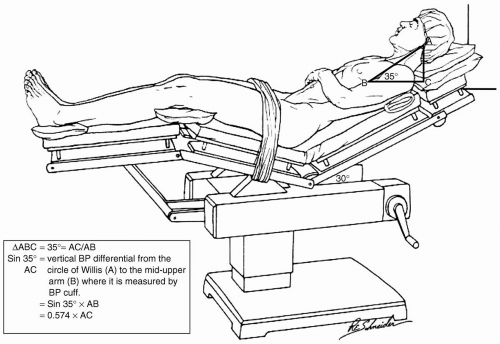
This position was developed in the 1980s for orthopedic shoulder arthroscopy procedures.2 Patients are placed upright at angles varying from 30 to 90 degrees above the horizontal plane (see Figs. 58.1 to 58.3.) Pillows are placed beneath their ankles and knees and behind their head. The danger of brachial plexus and forearm neuropathies is decreased compared to the lateral decubitus position. Both the surgeon and anesthesia provider have excellent access to the shoulders, head, and neck.
HEMODYNAMIC CONSEQUENCES
Potentially significant hemodynamic consequences can occur when patients are moved to the upright position. Marked decreases in mean arterial pressure (MAP), central venous pressure (CVP), pulmonary artery occlusion pressure (PAOP), stroke volume, stroke volume index, cardiac output, cardiac index, and PaO2 have been described, together with significant increases in (PaO2-PaO2), pulmonary vascular resistance, and total peripheral resistance.3,4 In addition, the upright posture during general anesthesia decreases the linear velocity of cerebral blood flow (CBF) which, when coupled with the reduced stroke volume, creates a risk of cerebral tissue ischemia.5 Because the neurogenic mechanisms of CBF autoregulation may be disordered during anesthesia, stabilization of central hemodynamics at all stages of anesthesia is an important factor for optimizing brain tissue perfusion.
Changes in intrathoracic blood volume caused by a change in body position also occur in anesthetized patients. When measurements of cardiac index, intrathoracic blood volume, pulmonary blood volume, and total circulating blood volumes were performed in anesthetized patients in the supine and sitting positions, a significant decrease in intrathoracic blood volume was accompanied
by similar significant decreases in cardiac index, stroke volume index, and MAP after change from the supine to the sitting position.6 If one considers the potential for peripheral vasodilatation and myocardial depression that can occur in patients who are anesthetized with potent inhalational agents, the detrimental effects of the upright position and anesthesia can be significant.2
by similar significant decreases in cardiac index, stroke volume index, and MAP after change from the supine to the sitting position.6 If one considers the potential for peripheral vasodilatation and myocardial depression that can occur in patients who are anesthetized with potent inhalational agents, the detrimental effects of the upright position and anesthesia can be significant.2
What Is Cerebral Autoregulation?
▪ LOWER AND UPPER LIMITS
For decades, cerebral autoregulation has been thought to maintain CBF constant between an MAP of 50 mmHg (the lower limit of cerebral autoregulation [LLA]) and 150 mmHg (the upper limit of cerebral autoregulation [ULA]) as shown in Figure 58.1. Therefore, the consequences of reduced MAP, cardiac index, and the other changes discussed in the preceding paragraphs caused little concern, at least not so long as the MAP remained above 50 mmHg. This particular value appears to have been fostered by a publication by McCall.7 Forty-two pregnant women, or women in the early puerperium (24 preeclamptic and 18 normal), were treated with hydralazine or Veratrum viride to observe the effects of reduced MAP on CBF. Although MAP in the two normal groups of nine patients each was reduced to 57 mmHg with Veratrum viride and 64 mmHg with hydralazine, CBF remained constant in the former group and actually increased in those treated with hydralazine. This publication was cited by Lassen8 in 1959, and according to Drummond,9 has been quoted ever since as evidence of the 50 mmHg LLA.
Modification of Thresholds
Thresholds for autoregulation of CBF in certain patient populations are modified as necessary. In poorly controlled hypertensive patients, autoregulation of CBF is shifted to the right, requiring higher MAP and cerebral perfusion pressure (CPP) to ensure adequate cerebral perfusion. However, animal studies suggest that adequate antihypertensive medication may, in time, return this curve to its normal values10 so that patients with well controlled hypertension may have normal threshold values. Autoregulation is also influenced by the time course over which CPP changes occur. Rapid changes, even when within normal autoregulation limiting values, may induce transient (3 to 4 minutes) alterations in CBF.11
▪ MEAN ARTERIAL PRESSURE VERSUS CEREBRAL PERFUSION PRESSURE
In recent years, significant evidence has been presented suggesting that the quoted value of 50 mm Hg for the LLA is incorrect for humans.12,13,14,15,16,17,18,19 Instead, a range of normal LLA exists, which varies from 70 mmHg to 93 mmHg, with a mean value of 80 ± 8 mmHg9,20 (see Table 58.1). Because the LLA in patient populations varies so widely, the predicted value for an individual patient should not be based on quoted averages. Instead, each specific patient’s LLA should be calculated at a suggested value that is 25% less than the resting MAP.2,9 Taking these facts into account, investigators should not portray the cerebral
autoregulation curve as traditionally shown in Figure 58.4. Rather than sharp and incorrect inflection points at the LLA and ULA, the “shoulders” should be rounded, thereby reflecting the range of normal LLA rather than a specific value of 50 mmHg20,21 (see Fig. 58.5).
autoregulation curve as traditionally shown in Figure 58.4. Rather than sharp and incorrect inflection points at the LLA and ULA, the “shoulders” should be rounded, thereby reflecting the range of normal LLA rather than a specific value of 50 mmHg20,21 (see Fig. 58.5).
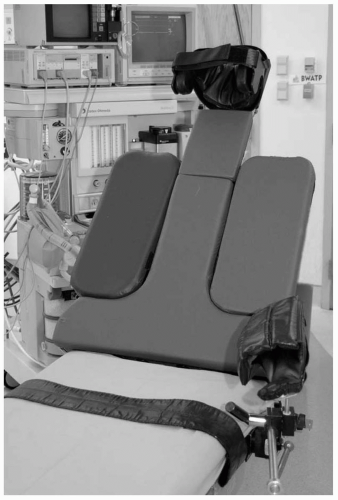 FIGURE 58.3 Frontal view of the beach chair attachment showing the head and arm holders. The two lateral support pads can be removed, allowing free surgical access to the upper arms and shoulders. |
Drummond11 pointed out that the units on the x-axis of autoregulation curves determine the correct inflection points. If the MAP is being discussed, the LLA normally is not less than 70 mm Hg. MAP usually is portrayed, because the true CPP, equal to the MAP minus the intracranial pressure (ICP) or CVP, commonly is unknown. If a normal ICP of 10 to15 mmHg is assumed in a supine individual, the LLA expressed as MAP would be 70 mm Hg, whereas the LLA expressed as CPP would be 55 to 60 mmHg (70 mmHg minus 10 to 15 mmHg). Clearly, if the LLA expressed as MAP was higher,12,13,14,15,16,17,18,19,20 the CPP also would be higher.
Safe Limits
Although studies have shown that normal cerebral oxygen metabolism can be maintained down to CPP of 30 to 40 mm Hg with deliberate hypotension, values so low are not recommended.21 Such limits serve no useful purpose and leave no margin for error in case the lower CPP is further reduced. This situation is an excellent example of the general statement that just because we can do something does not mean that we should.
TABLE 58.1 Lower Limit of Cerebral Autoregulation in Human Studies | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||
DELIBERATE VERSUS INADVERTENT HYPOTENSION
Techniques used to induce deliberate hypotension when the patient is in the supine or lateral position are different from the factors that decrease CPP below a generally recognized safe LLA when the patient is upright. A comparison of deliberate but controlled hypotension with maintained cardiac output versus inadvertent hypotension from hypovolemia or myocardial depression, with an associated decrease in cardiac output, is akin to comparing apples to oranges. Two reports demonstrate this fact.22,23
In the first study,22 induced hypotension produced by extradural anesthesia was assessed in patients with medically controlled hypertension. The hemodynamic response to hypotension was assessed in 38 nonhypertensive and 31 controlled hypertensive patients. All received extradural anaesthesia to T4 or above, which decreased MAP to 52 mmHg and 55 mmHg in the normotensive and hypertensive patients, respectively. Cardiac output (thermodilution) was maintained by low dose, continuous infusions of epinephrine (1 to 5 µg per minute).
The second study,23 a randomized, controlled clinical trial, included 235 older adults with comorbid medical illnesses undergoing elective primary total hip
replacement with 0.75% bupivacaine epidural anesthesia and adjunctive midazolam, fentanyl, and thiopental sodium as needed. The patients were randomly assigned to one of two levels of intraoperative MAP management: A markedly hypotensive MAP range of 45 to 55 mmHg and a less hypotensive range of 55 to 70 mm Hg.
replacement with 0.75% bupivacaine epidural anesthesia and adjunctive midazolam, fentanyl, and thiopental sodium as needed. The patients were randomly assigned to one of two levels of intraoperative MAP management: A markedly hypotensive MAP range of 45 to 55 mmHg and a less hypotensive range of 55 to 70 mm Hg.
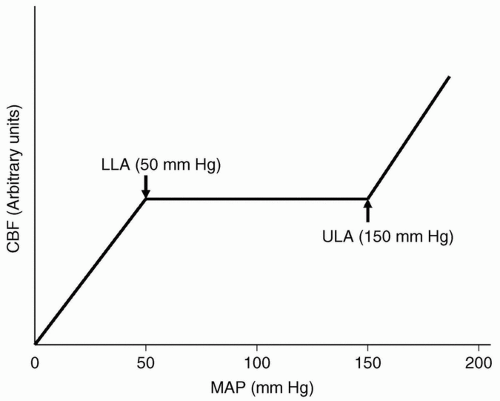 FIGURE 58.4 A classic representation of the CBF-pressure (autoregulation) curve is made up of three straight lines: one horizontal line between the LLA and the ULA and two sloped lines below the LLA and above the ULA, respectively. Between the LLA and ULA, CBF is autoregulated by changing vessel diameter, and CBF remains constant. Vessels dilate as pressure decreases and reach their maximal size when pressure falls below the LLA. Similarly, vessels constrict as pressure increases and maintain their minimal size when pressure rises above ULA. The two sloped lines are parallel, and the LLA and LUA are represented as specific points (knees) at 50 mmHg and 150 mm Hg, respectively. CBF, cerebral blood flow; LLA, lower limit of cerebral autoregulation; ULA, upper limit of cerebral autoregulation; MAP, mean arterial pressure.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|