In Duchenne muscular dystrophy, succinylcholine is contraindicated due to risk of hyperkalemia and rhabdomyolysis.
II. The Myotonias
Myotonic dystrophy is an autosomal dominant disorder caused by gene mutations that lead to RNA toxicity, ion channel dysfunction, and myotonias, or impaired skeletal muscle relaxation. Progressive muscle wasting with weakness combined with multisystem involvement characterizes this disorder. Myotonic dystrophy is divided into two chief genetic entities. Myotonic dystrophy type 1 (DM1), the predominant major type, is subdivided into congenital, child, and adult onset. Myotonic dystrophy type 2 is rare, with a highly variable, late adult onset presentation.
Adult onset DM1, the most common subtype, is characterized by muscle weakness, myotonias, and cataracts. Facial, neck, and distal limb weakness progress to muscle wasting, immobility, and bulbar palsies. Respiratory dysfunction is compounded by aspiration and respiratory muscle weakness.
Functional and anatomical brain dysfunction is manifested by cognitive dysfunction and diffuse white matter atrophy. Systolic and diastolic cardiac failure are complicated by conduction defects, such as atrioventricular conduction blocks and tachyarrhythmias. Sudden cardiac death due to dysrhythmias is common. Gastrointestinal signs include constipation and diarrhea. Impaired endocrine function results in hypothyroidism and insulin resistance. Treatment is primarily supportive.
A. Management of Anesthesia
Cardiopulmonary abnormalities, muscle weakness, and clinical myotonia are the primary causes of perioperative risk in adult onset DM1, regardless of anesthetic technique. Sedatives should be used with caution due to potential exaggerated response to their respiratory depression side effects. Succinylcholine should be avoided due to its potential to trigger a severe myotonic muscle contraction. Both nondepolarizing and reversal agents may exacerbate muscle weakness and should be avoided. Respiratory insufficiency can occur. Transcutaneous pacing pads should be considered.
There is potential for prolonged labor, postpartum hemorrhage, and congenital myotonic dystrophy of the neonate.
III. Familial Periodic Paralysis
Channelopathies are a heterogenous group of defects in ion channel function that result in a spectrum of anomalies. Familial periodic paralysis is a subgroup of inherited defects comprising hyperkalemic and hypokalemic periodic paralysis.
A. Hyperkalemic Periodic Paralysis
Hyperkalemic periodic paralysis is an autosomal-dominant inherited disease characterized by episodes of hyperkalemia-related muscle weakness and myotonia. The episodes are triggered by transient hyperkalemia from exercise, fasting, or consumption of potassium-rich foods.

Hypokalemic periodic paralysis is the most common periodic paralysis disease, characterized by recurrent episodes of hypokalemia-related flaccid paralysis, which can last hours to days.
B. Hypokalemic Periodic Paralysis
Hypokalemic periodic paralysis, the most common periodic paralysis disease, is an autosomal-dominant disease characterized by recurrent episodes of hypokalemia-related flaccid paralysis, lasting hours to days. Respiratory insufficiency and cardiac arrhythmias can occur during acute attacks. Chronic proximal myopathy is a common outcome in many cases.
C. Management of Anesthesia
Potassium homeostasis is the goal of perioperative management. Electrolyte levels should be monitored and corrected with an emphasis on avoiding metabolic states or medications that may alter serum potassium levels, either directly or indirectly. Nondepolarizing muscle relaxants are best avoided due to unpredictable patient sensitivities. Succinylcholine should be avoided, because it may cause transient hyperkalemia (2).
IV. Myasthenia Gravis
Myasthenia gravis (MG) is a neuromuscular autoimmune disease characterized by skeletal muscle weakness worsened by exertion and improved with rest. Extraocular muscles are affected primarily, with less frequent impact on limb and respiratory muscles strength.

Myasthenia gravis is caused by a decrease in the number of functional postsynaptic, acetylcholine receptors in the neuromuscular junction available for acetylcholine binding.
The etiology is a decrease in the number of functional postsynaptic, acetylcholine receptors (AChR) in the neuromuscular junction available for acetylcholine binding. Direct antibody receptor blockade, increased antibody-mediated receptor turnover, and postsynaptic membrane complement–mediated injury can contribute to AChR decline. Abnormal thymus tissue is frequently involved.
Signs include ptosis, blurred vision, diplopia, dysphagia, dysarthria, and generalized limb weakness. Myasthenic crisis is a progression to severe muscle weakness and respiratory failure, usually requiring ventilatory support. Cardiac abnormalities include bundle branch blocks, atrial fibrillation, and focal myocarditis.
Transient neonatal myasthenia is known to occur in newborns of women with active MG, with feeding problems and respiratory distress immediately postpartum. Edrophonium testing is used to diagnosis MG with high sensitivity. Serologic testing, tomographic imaging, and electrophysiological testing comprise a comprehensive MG workup. Treatment is aimed at both symptom management and immunomodulation.

The newborn of a mother with myasthenia gravis can suffer from a condition known as transient neonatal myasthenia, which may present with feeding problems and respiratory distress at birth.
Acetylcholinesterase inhibitors, such as pyridostigmine, minimize MG symptoms by increasing the acetylcholine available at neuromuscular junction sites. Excessive drug administration can result in severe cholinergic side effects, or cholinergic crisis, characterized by hypersalivation, abdominal cramping, bradycardia, and weakness. Plasmapheresis and intravenous immunoglobulin can provide short-term relief. Chronic therapy includes steroids and nonsteroidal immunosuppressants. Thymectomy is recommended for MG patients with thymomas (3).
A. Myasthenic Syndrome (Lambert-Eaton Syndrome)
Lambert-Eaton myasthenic syndrome (LEMS) is an autoimmune, neuromuscular disorder of transmission mediated by antibodies to voltage-gated calcium channels at the presynaptic, motor nerve terminal, resulting in acetylcholine release reduction. It is characterized by proximal limb weakness, autonomic dysfunction such as dry mouth, and diminished deep tendon reflexes. In contrast to MG, exercise in LEMS might suddenly improve symptoms. LEMS is a paraneoplastic condition, often associated with small cell lung cancer. Increasing presynaptic, neurotransmitter release with 3,4-diaminopyridine is considered the mainstay of treatment.

The Lambert-Eaton myasthenic syndrome is associated with small cell lung cancer and, in contrast to myasthenia gravis, exercise might improve the muscle weakness-related symptoms.
V. Guillain-Barre Syndrome (Polyradiculoneuritis)
Guillain-Barre syndrome (GBS) is an autoimmune disorder characterized by the acute or subacute onset of ascending skeletal muscle weakness or paralysis of the legs occurring in the context of a viral or bacterial infection. This inflammatory, multifocal demyelinating disease usually produces varying degrees of autonomic dysfunction. Respiratory muscle weakness is common during severe cases of GBS. Treatment is primarily supportive (4).
A. Management of Anesthesia
Multifocal demyelination and muscle disuse atrophy in GBS prohibit the use of succinylcholine due to the risk of life-threatening hyperkalemia. Expected muscle relaxation from nondepolarizing agents may be highly variable and unpredictable and should be avoided. Autonomic nervous system lability is common, which can result in hyperdynamic and hypodynamic responses to stimuli or transient preload changes, respectively; therefore, hemodynamic support should be judicious.

In addition to respiratory muscle weakness, Guillain-Barre syndrome is accompanied by autonomic nervous system lability, which can result in hyperdynamic and hypodynamic responses.
VI. Central Nervous System Diseases
A. Multiple Sclerosis
Multiple sclerosis (MS) is an inflammatory multifocal demyelinating disorder caused by autoimmune neurodegenerative changes leading to progressively irreversible neurologic deficits. The clinical course is characterized by subacute, relapsing–remitting changes that correlate to activated T-cell blood–brain barrier penetration with subsequent multifocal gray and white matter demyelination and edema (Fig. 17-1).
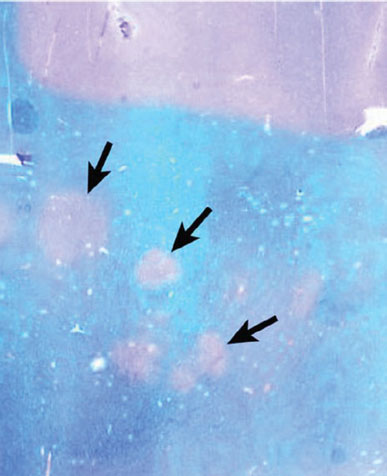
Figure 17-1 The subcortical white matter of a patient with multiple sclerosis showing multiple, small, irregular, partially confluent areas of demyelination (arrows). Normal intact myelin stains blue in this Luxol fast blue–stained section. (From Rubin R, Strayer DS, Rubin E. Rubin’s Pathology. 6th ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins, 2011, with permission.)
MS has a peak incidence at age 20 to 40 years. Signs and symptoms can be vague or specific, usually determined by the neurologic site focally affected. Symptoms include headache, fatigue, and depression. Sensory symptoms such as numbness and paresthesias are common. Partial paralysis of the lower limbs is a common motor symptom that usually correlates to anterior column spinal cord lesions. Visual loss, diplopia, nystagmus, and papillary abnormalities reflect cranial nerve involvement. Diagnosis is based on history and clinical examination with reliance on magnetic resonance imaging to characterize demyelinating, often clinically silent, focal lesions. Cerebral spinal fluid may demonstrate intrathecal immunoglobulin production.
Management strategies are evolving to target acute relapse and symptomatic control. Corticosteroids can hasten acute clinical recovery. Plasma exchange removes harmful antibodies to treat relapses. Interferon-beta and glatiramer acetate block antigen presentation to minimize relapsing–remitting events. Mitoxantrone, an antineoplastic agent, reduces lymphocyte counts to delay progression to secondary degenerative phase. Symptomatic management is usually determined by the diffuse nature of MS. Severe fatigue is common and should be treated promptly with central nervous system stimulants, such as amantadine. Routine depression screening and early treatment are important given the propensity to affect quality of life in this disease. Spasticity treatment requires both physical therapy and antispasticity medications. Intrathecal baclofen pump implantation is reserved for severe cases. Pain is usually due to varied factors, such as neuropathic pain, indirect pain from MS, and treatment-related pain. As a result, pain management is multimodal, potentially involving antiepileptics, tricyclic antidepressants, nonsteroidal anti-inflammatory drugs (NSAIDs), and antispastic agents.

In multiple sclerosis, pain is caused by a variety of mechanisms; therefore, the best treatment is using multimodal analgesia.
B. Epilepsy
Epilepsy is a disorder characterized by sudden, unprovoked, and recurrent seizures. A seizure is a neurologic symptom characterized by a transient attack of rhythmic electroneuronal discharges, resulting in altered consciousness and disturbances in brain function. Seizures can be provoked by factors such as metabolic derangements, or unprovoked, by intrinsic brain disease.
Epilepsies and seizures are mostly clinical diagnoses with reliance on history, physical examination, laboratory testing, electroencephalography, and neuroimaging. Investigating the paroxysmal event, triggers, and recurrence potential helps exclude or confirm the diagnosis.
Epilepsies are broadly divided into focal and generalized. In focal epilepsies, usually localized pathologic conditions, such as brain tumors, lead to focal cortical discharges that can generalize and recruit other cortical regions. In generalized epilepsies, diffuse cortical discharges develop, affecting the cortex and bilaterally. Grand mal seizure is the most recognized type of generalized epilepsy. It is characterized by a loss of consciousness followed by several minutes of a tonic phase of body stiffening, followed by a clonic phase
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








