CHAPTER 41

ANORECTAL ABSCESS
Anorectal abscess is by far the most common colorectal disease requiring acute care and surgery. The overwhelming majority of anorectal abscesses originate from infection in anal glands, which drain into the crypts of Morgagni at the dentate line. Occlusion of the draining channel in bacteria-rich environment produces an abscess in the intersphincteric space before spreading to adjacent spaces (Fig. 41.1).
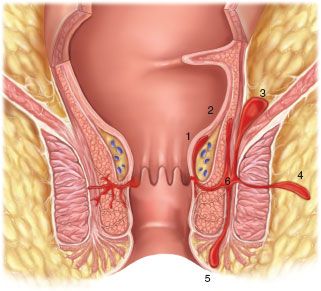
FIGURE 41.1. Anal glands opening in anal crypts.Extension of abscess to adjacent spaces: 1. Submucosal; 2. High intermuscular; 3. Supralevator; 4. Ischiorectal; 5. Perianal; 6. Intersphincteric.
Other causes of anorectal abscess include Crohn’s disease, rare specific infections such as tuberculosis, actinomycosis, and pinworm infestation in children. Trauma with external (penetrating) injuries or internal perforation of anorectum (from ingested sharp objects such as toothpicks, fish or chicken bones) may cause an abscess, which can also appear acutely or as a smoldering infection, often difficult to diagnose.
The presenting symptoms of anorectal abscess vary depending upon the extension of infection in perianal or perirectal spaces and whether the abscess is located proximal or distal to the anorectal ring (Fig. 41.2). Low abscesses , that is, those located distal to the anorectal ring, include intersphincteric, perianal or ischiorectal, depending on the anatomic site of the purulent collection between the sphincters, at the anal verge or in the ischiorectal fossa. These abscesses are associated with intense localized symptoms such as pain, swelling, erythema, cellulitis, tenderness, and fluctuation later in the disease process. In intersphincteric abscesses, the pain is aggravated with Valsalva maneuver (coughing, sneezing, laughing) On the other hand, the patient may have little or no systemic symptoms of fever, chills, and malaise, probably because of earlier diagnosis and intervention. The low abscesses are easier to diagnose, with the exception of posterior midline intersphincteric abscesses in male patients where the infection is sequestered in the intersphincteric or deep postanal space. The only way to reliably make the diagnosis is a careful bidigital examination, which may need to be done under anesthesia if the patient is in too much pain to tolerate examination otherwise. With the index finger, gently pushing posteriorly and the thumb pressing between the coccyx and the anus, the warm, tender swelling and induration can be easily palpated. The more superficial perianal or ischiorectal abscess can be drained urgently in the office, clinic, or emergency department with liberal use of local infiltration anesthesia.
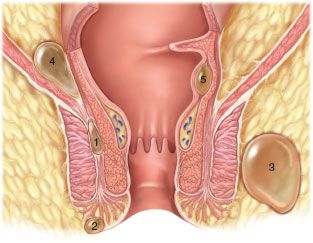
FIGURE 41.2. High abscesses: 1. Intersphincteric; 2. Perianal; 3. Ischiorectal; 4. Supralevator; 5. Submucosal/intermuscular.
High abscesses , that is, those located proximal to the anorectal ring (e.g., high intermuscular/submucosal or supralevator), often present with minimal local symptoms such as pelvic or rectal pressure on sitting or defecation. However, they may be associated with more systemic symptoms of fever, chills and malaise, and ketoacidosis in diabetics. These patients often identified as having “fever of unknown origin” are subjected to unnecessary laboratory and imaging studies and ineffective nonoperative treatment with oral or intravenous antibiotics. A high index of suspicion and a careful gentle rectal examination is all that is needed to arrive at the correct diagnosis. If the patient does not tolerate the examination in the outpatient setting, then he/she should be examined under anesthesia where proper and expeditious surgical procedure can be performed at the same time.1
The principle of surgical therapy of anorectal abscess is early, adequate, and dependent drainage. Small superficial abscesses may be drained under local infiltration anesthesia. A cruciate incision is preferable to a simple incision because its edges retract and the corners can be excised with a scalpel or iris scissors to create a small opening and prevent premature sealing of the incision with the thick proteinaceous pus. The incision should be made on the prominent point of the abscess and it must be placed as close to the anus as possible to shorten the length of a subsequent fistula should one develop postoperatively. Packing or placement of mushroom drains is usually unnecessary and may cause undue pain at insertion and removal.
Larger abscesses must be drained in the operating room under regional or general anesthesia. This allows exploration of adjacent spaces to drain the abscess thoroughly and also to probe and identify an associated fistula tract. If the abscess is very large, multiple openings (unroofing) is preferable to a long anteroposterior incision. Smaller (1–2 cm) openings can be connected with Penrose drains looped around the intact skin bridges and sutured to itself to maintain postoperative drainage as long as necessary. These openings heal within 4–6 weeks of removal of Penrose drains while a long anteroposterior, circumanal incision undergoes a step-off deformity (due to retraction of sphincter mechanism medially) and may take months to heal, leaving significant postoperative scarring.2 Contrary to popular belief, there is no septation in an abscess cavity to be broken up. Exploration of cavity is only indicated to exclude extension to adjacent spaces.
If infection spreads bilaterally (horseshoe abscess), the patient should be taken to the operating room for adequate drainage. A horseshoe abscess always originates from an infection in the deep postanal space. If the surgeon is adequately trained to deal with the primary source, a midline sphincterotomy should be done. Otherwise, bilateral abscesses should be drained to deal urgently with sepsis and leave the fistula to be dealt with subsequently and in more experienced hands if necessary.
High abscesses need to be drained in the operating room under anesthesia for good exposure. If the submucosal or high intermuscular abscess bulges into the rectal lumen, it should be drained into the rectum. A small (1 × 1 cm) window overlying the abscess should be excised for biopsy as well as for prolonging drainage and to delay premature healing of the incision. A supralevator abscess pointing into the rectum may be drained in a similar fashion. But if it has tracked caudad into the ischiorectal fossa, as it often does, it should be drained through ischiorectal space, providing it with dependent drainage. A supralevator abscess should never be drained both through the rectum as well as externally as this will result in an extrasphincteric fistula, which is extremely difficult if not impossible to cure later on.3
The natural history of anorectal abscesses after early drainage is as follows: (a) It may heal and never recur; (b) It may heal and recur at the same area, months or years later; or (c) It may never heal and remain as a persistent draining sinus. The latter two scenarios signify the presence of a fistula. Therefore, in select cases when a fistula is identified at the time of abscess drainage and the portion of the sphincter mechanism overlying the fistula tract is very small, the surgeon may elect to perform a primary fistulotomy. This will treat the fistulous abscess definitively, shorten sick days, minimize morbidity, and prevent recurrences.4 However, primary fistulotomy in inexperienced hands may result in unintended extensive sphincterotomy and subsequent fecal incontinence. Therefore, when a fistula is identified but the surgeon is uncertain about its extent and complexity, it is best to place a nonabsorbable braided suture (No. 1 or 2 silk) or silastic (vessel) loop into the tract, tying it loosely as a draining Seton. This will provide long-term drainage, prevent recurrence of abscess, and allow the definitive treatment of the fistula to be postponed to a later date or referral to a more experienced surgeon.5,6
FOURNIER’S GANGRENE
Fournier’s gangrene or synergistic perianal or scrotal gangrene was first described in 1883. The symptoms and tissue necrosis may evolve rapidly, within a few hours in young men, or follow a more insidious course lasting 2–3 days in the elderly. Enriquez et al.,7 in a retrospective comparison of Fournier’s gangrene, found that those secondary to GI causes had slower onset than those related to GU causes.
The illness typically begins with perianal, scrotal or penile pain, swelling, fevers, chills, and urinary retention. Symptoms may be present for a few days but the patient may present with septic shock without anorectal or urogenital complaints. A careful history must be taken to elicit presence of comorbidities, especially instrumentation, unusual sexual practices, HIV, and most importantly, diabetes mellitus which is present in over 50% of the patients.
Physical examination reveals gross swelling of perineum, penis, scrotum, and gluteal regions (Fig. 41.3). Overlying skin may show purpura, necrosis (black spots), and is often associated with crepitus. In extreme cases, these signs may extend to thighs, groins, lower abdominal wall, and anterior or posterior chest wall. The area may be exquisitely tender but necrotic skin is often anesthetic. Spontaneous drainage from watery brown liquid to frank pus may occur and is associated with characteristic feculent odor. Signs and symptoms of systemic toxicity such as fever, tachycardia, hypotension, or altered mental status may be present.

FIGURE 41.3. Fournier’s gangrene involving bilateral ischiorectal fossa and scrotum.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








