Bladder perforation with extravasation of the irrigating fluid is a well-known risk of transurethral bladder resection.
 VIDEO 42-1
VIDEO 42-1
Transurethral Resection of the Prostate
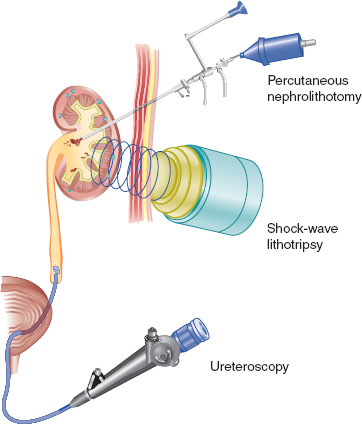
FIGURE 42-1 Urinary tract stones: Intervention choices. (From Stafford-Smith M, Shaw A, Sandler A, et al. The renal system and anesthesia for urologic surgery. In: Barash PG, Cullen BF, Stoelting RK, et al. Clinical Anesthesia, 7th ed. Philadelphia: Lippincott Williams & Wilkins, 2013:1114.)
C. Resection of the Prostate
Benign prostatic hyperplasia (BPH), the most common benign tumor in men, is responsible for the majority of urinary symptoms in men older than 50 and results in a need for prostatectomy in approximately one-third of all men who live to age 80. Transurethral resection of the prostate (TURP) is the primary treatment for symptomatic BPH. In this procedure, a resectoscope is used to remove prostatic tissue that is protruding into the urethra with preservation of the prostatic capsule. Continuous irrigation of the bladder and prostatic urethra is required to maintain visibility, distend the operative site, and remove dissected tissue and blood. During TURP, violation of the prostatic capsule results in absorption of large amounts of irrigation solution into the circulation and the periprostatic and retroperitoneal spaces.

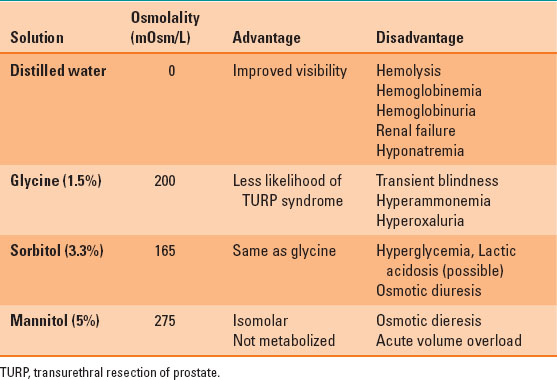
Most of the irrigating solutions are hypoosmolar and acidic. Transient blindness is associated with glycine irrigation, hyperglycemia is associated with sorbitol and volume overload is associated with the use of mannitol.
Irrigating Solutions for Transurethral Resection of the Prostate
The ideal irrigating fluid should be isotonic, nonhemolytic, nontoxic, electrically inert (if a monopolar electrical resecting electrode is used), transparent, rapidly excreted, and inexpensive. Most of the irrigating solutions are hypo-osmolar and acidic, as shown in Table 42-1. Isotonic irrigation solutions (normal saline and lactated Ringer’s solution) are available, but these electrolyte solutions are ionized and conduct electrical currents.
Table 42-1 Properties of Commonly Used Irrigating Solution during Transurethral Resection of Prostate Procedure

Absorption of the irrigating fluid during TURP is directly related to the number and size of opened venous sinuses, duration of resection, and the height of the bag of irrigating solution above the surgical table.
Transurethral Resection Syndrome
Absorption of large volumes of irrigating solution leads to respiratory distress secondary to intravascular volume overload, hyponatremia, and hypo-osmolality (1). The average amount of irrigating fluid absorbed during TURP is ~20 mL/min of resection time. The volume of fluid absorbed during the procedure can be estimated with the following formula:
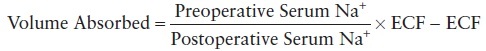
where ECF is extracellular fluid volume and Na+ is the sodium ion.
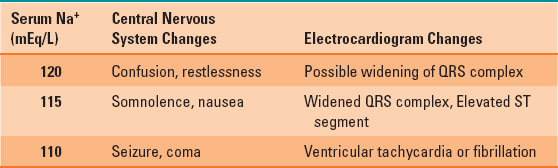
Absorption of the irrigating fluid during TURP is directly related to the number and size of venous sinuses opened, the duration of resection, and the height of the bag of irrigating solution above the surgical table, which determines the hydrostatic pressure driving fluid into prostatic veins and sinuses. Resection time should be limited to <1 hour and the bag of irrigating solution should be suspended no more than 30 cm above the operating table at the beginning of the resection and 15 cm in the final stages of resection. Irritability, restlessness, nausea, shortness of breath, dizziness, hypertension, and headache are early manifestations of TURP syndrome. They provide an early warning of developing hyponatremia and serum hypo-osmolality. The acute decrease in serum sodium concentration is responsible for many of the signs and symptoms of TURP syndrome, as shown in Table 42-2.

Absorption of large volumes of irrigating solution leads to intravascular volume overload, hyponatremia and hypoosmolality.
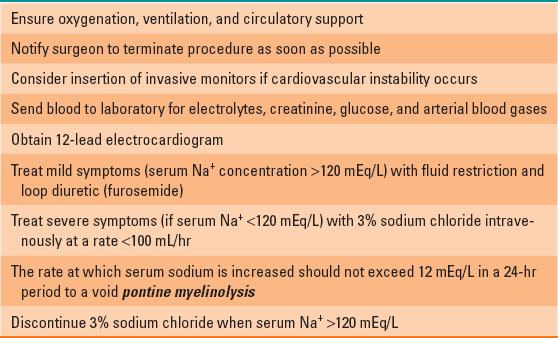
Symptoms related to absorption of a specific irrigating solution during the procedure may further complicate TURP syndrome, as shown in Table 42-1. Prompt treatment is necessary when neurologic or cardiovascular complications of TURP are recognized. Table 42-3 summarizes those treatments.
Table 42-2 Signs and Symptoms Associated with Acute Changes in Serum Na+ Levels
Bleeding and Coagulopathy
Several factors influence blood loss during TURP, such as the vascularity and size of the gland, duration of surgery, the number of sinuses opened during resection, and the presence of infection (2). Blood loss is difficult to assess because of its mixing with the irrigating fluid. Therefore, both intravascular volume assessment and serial hematocrit values may be necessary to estimate blood loss and the need for red cell transfusion. Excessive bleeding after TURP occurs in <1% of cases. In theory, primary fibrinolysis may result from prostatic release of tissue plasminogen activator, which converts plasminogen to plasmin. However, there is little evidence to support this factor as clinically significant or to support the practice of administering an antifibrinolytic such as aminocaproic acid. Disseminated intravascular coagulopathy is the likely etiology of abnormal bleeding after TURP.

Disseminated intravascular coagulopathy is the likely etiology of abnormal bleeding after TURP.
Bladder Perforation
The incidence of bladder perforation is ~1%, and most perforations are extraperitoneal, resulting in periumbilical, inguinal, or suprapubic pain in a conscious patient. The urologist may suspect perforation by noting the irregular return of irrigating fluid. Intraperitoneal bladder perforation occurs less frequently, and pain is more generalized in the upper part of the abdomen or referred to the precordial or shoulder. Pallor, restlessness, sweating, abdominal rigidity, nausea, vomiting, and hypotension usually accompanied this generalized pain.

The urologist may suspect perforation by noting the irregular return of irrigating fluid.
Table 42-3 Treatment of Transurethral Resection of Prostate Syndrome
Transient Bacteremia and Septicemia
Bacteremia is usually asymptomatic and easily treated with commonly used antibiotic combinations that are effective against gram-positive and gram-negative bacteria. In 7% of patients, septicemia may occur. Common manifestations include chills, fever, and tachycardia. In severe cases, bradycardia, hypotension, and cardiovascular collapse may occur, with mortality rates of 25% to 75%. Aggressive treatment with antibiotics and critical care support employing a sepsis protocol should be instituted.
Hypothermia
Heat loss results from irrigation, and absorption of room temperature irrigating fluid may lead to a significant decrease in the patient’s body temperature and shivering. The use of warmed irrigating solutions has been shown to minimize or prevent this problem.
Positioning Complications
TURP is performed in the lithotomy position with slight Trendelenburg. Without proper positioning and padding, the common peroneal, sciatic, and femoral nerves may be injured.
Anesthetic Techniques
Regional anesthesia (spinal or epidural) has been the technique of choice for TURP because the conscious patient can alert the clinicians to the early signs of TURP syndrome or bladder perforation. A sensory level to T10 is required to eliminate the discomfort caused by bladder distention. Spinal anesthesia is usually preferred over lumbar epidural anesthesia because sacral segments are sometimes inadequately blocked with lumbar epidural techniques. However, general anesthesia can be used safely as well, and the anesthetic technique should be tailored to the individual patient and surgical requirements.

Regional anesthesia has been the anesthetic technique of choice for TURP as the conscious patient can alert the clinicians to the early signs of TURP syndrome or bladder perforation.
Morbidity and Mortality After Transurethral Resection of the Prostate
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








