Did you know that the Hasson technique is preferred to the Veress needle technique in patients with abdominal adhesions?
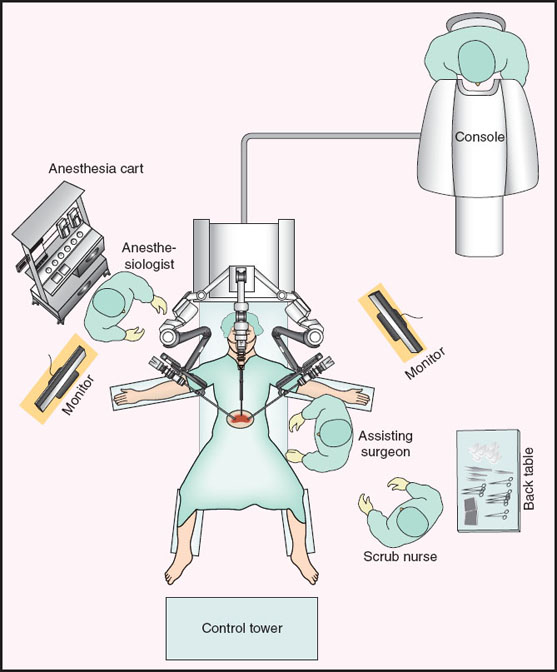
FIGURE 27-1 Layout of the operating room during robotic surgery. (From Joshi GP, Cunningham A. Anesthesia for laparoscopic and robotic surgeries. In: Barash PG, Cullen BF, Stoelting RK, et al., eds. Clinical Anesthesia. 7th ed. Philadelphia: Lippincott Williams & Wilkins; 2013:1260, with permission.)

FIGURE 27-2 A control console where the surgeon is stationed and operates the robotic arms and camera. (© 2012 Intuitive Surgical, Inc., with permission.)
II. Physiologic Effects
A. Systemic Cardiovascular Effects
Cardiovascular changes during laparoscopy become apparent when the intra-abdominal pressure exceeds 10 mm Hg, resulting from the combination of increased intra-abdominal pressure, CO2 absorption, general anesthesia, and patient positioning. Cardiac output decreases due to decreased venous return, which is secondary to the increased intra-abdominal pressure, causing inferior vena cava compression and pooling of blood in the lower extremities. Systemic vascular resistance increases secondary to the catecholamine release stimulated by the absorbed CO2 and to the release of vasopressin and activation of the renin-angiotensin system caused by the pneumoperitoneum. In addition, during the insufflation phase of laparoscopy, stretching of the peritoneum stimulates a vagal reflex and may cause bradycardia or even asystole. These changes occur in the first minutes after establishing the pneumoperitoneum. Subsequently, both cardiac output and systemic vascular resistance normalize within 10 to 15 minutes. When steep Trendelenburg positioning is required, as it is for robot-assisted radical prostatectomies, it increases venous return and cardiac output, thereby opposing the changes due to pneumoperitoneum. In contrast, reverse Trendelenburg and lithotomy positioning further decrease cardiac output by further impairing venous return.
B. Regional Perfusion
Pneumoperitoneum induces a modest splanchnic hyperemia due to the vasodilating effects of the absorbed CO2. In contrast, pneumoperitoneum decreases renal blood flow, glomerular filtration rate, and urine output by up to 50%. Cerebral blood flow increases during pneumoperitoneum due to an increase in arterial carbon dioxide partial pressure (PaCO2). This may be a transient effect if normocarbia is re-established by increasing minute ventilation appropriately. However, if steep Trendelenburg is employed, it increases intraocular pressure and could further increase intracranial pressure (2). Clearly, patients at risk for cerebral hypertension and those with poorly controlled glaucoma may not be appropriate candidates for this positioning (Table 27-1).
Table 27-1 Physiologic Changes during Laparoscopy
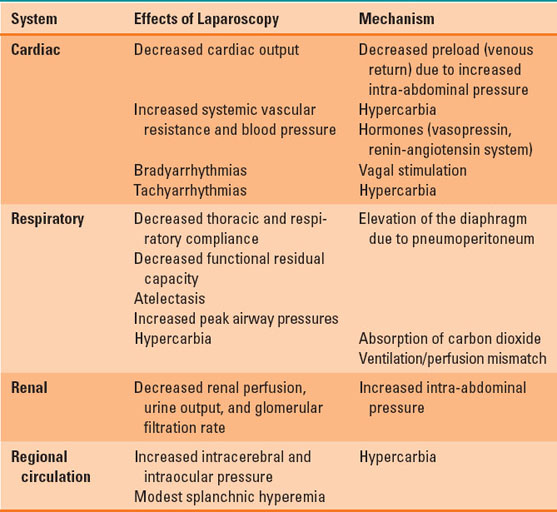
C. Respiratory Effects
Intra-abdominal insufflation elevates the diaphragm, causing a decrease in thoracic and respiratory compliance and in functional residual capacity. These changes lead to atelectasis unless countered by positive end-expiratory pressure and periodic recruitment maneuvers. General anesthesia and the combined respiratory effects of pneumoperitoneum increase mismatching of ventilation and perfusion, and through that mechanism decreases PaO2 (3). Postoperative pulmonary function tests demonstrate a reduction in one-second forced expiratory volume (FEV1) and forced vital capacity (FVC) (Table 27-1).

Did you know that the pneumoperitoneum induced for laparoscopy decreases respiratory compliance and functional residual capacity and worsens pulmonary perfusion and ventilation matching?
III. Anesthetic Management
A. Patient Selection
Patients with cardiac disease, especially severe valvular heart, may not tolerate the cardiovascular effects of pneumoperitoneum. Similarly, morbidly obese patients, patients with severe chronic obstructive pulmonary disease, and those with severe cardiac disease may not be able to compensate for the steep Trendelenburg position often required for some laparoscopic or robotic-assisted procedures. For routine laparoscopic cholecystectomy, obesity and even morbid obesity do not seem to increase the rate of significant complications (4).
B. Induction of Anesthesia and Airway Management
Regional or local anesthesia may be adequate for procedures performed quickly and with low intra-abdominal pressure (<10 to 15 mm Hg) and only mild degrees of Trendelenburg. However, general endotracheal anesthesia is most often required for laparoscopic procedures because of the discomfort from the pneumoperitoneum and the required ventilator support. Virtually any well-managed anesthetic induction technique is acceptable, but propofol may be the preferred agent for its antiemetic properties (5). Like regional and local anesthesia, use of a laryngeal mask airway instead of endotracheal intubation is reserved for patients undergoing short procedures requiring low insufflation pressures and minimal Trendelenburg.
C. Maintenance of Anesthesia
Because neuromuscular relaxation is required to limit the insufflating pressure in the abdomen, the maintenance anesthetic usually includes an inhaled anesthetic to ensure full unconsciousness. Nitrous oxide is usually avoided given the risk of worsening postoperative nausea and vomiting (PONV) and its potential for diffusing into the bowel, worsening surgical conditions. Total intravenous anesthesia can be used if the risk of PONV is significant. But the remote risk of patient awareness may be higher than when an inhaled agent is used with monitored exhaled gas analysis. Controlled normocapnic ventilation with positive end-expiratory pressure is required for most laparoscopic and robot-assisted procedures to counter the respiratory impact of the pneumoperitoneum and positioning.
Monitoring other than the American Society of Anesthesiologists standards for general anesthesia should be dictated by the each patient’s comorbidities. Because of the extremes of positioning and case duration sometimes required, adequate padding of the ulnar and common peroneal nerves, appropriate positioning of the arms and padding of the shoulders to avoid brachial plexus injury, and safety belt securing of the patient to the operating room table must be confirmed prior to incision. If the Trendelenburg or reverse Trendelenburg position is required, it should be achieved slowly to allow for management of hemodynamic changes or migration of the endotracheal tube. Prior to emergence, antiemetic medications should be administered because the incidence of PONV after laparoscopic procedures is high.
IV. Pain Prevention
Pain after laparoscopy procedures is far less than after comparable procedures performed through open laparotomy. However, the insertion sites of the instruments are painful, and CO2 insufflation and residual pneumoperitoneum cause diaphragmatic irritation, leading to referred pain to the shoulder (6
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








