SOME BACKGROUND ON RISK
A more complete understanding of risk necessarily flows from the development of an accurate definition of the term risk. One dictionary definition of risk is “possibility of suffering harm or loss (danger), a factor, course or element involving uncertain danger (hazard)”.1 To increase our knowledge of this area of medicine, we must first explore society’s understanding of risk. Ultimately, the anesthesiologist can then define risk effectively as it pertains to the practice of the specialty (see Box 1-1).
BOX 1-1 The Anesthesiologist and Risk: Essential Concepts
 Balancing patient benefit to anesthetic risk
Balancing patient benefit to anesthetic risk
 Understanding emotional aspects of risk
Understanding emotional aspects of risk
 Caring for the patient in a comprehensive manner
Caring for the patient in a comprehensive manner
 Understanding risk analysis
Understanding risk analysis
 RISK CONCEPTS
RISK CONCEPTS
We live in a society that struggles with balancing risks. When one takes a step back from risk analysis, it becomes clearer that risk analysis is, in fact, decision analysis. The decision imparts action to balancing the risk involved. For example, many people worry a great deal about flying, despite an outstanding safety record in commercial air travel. Many of these same travelers continue to smoke and to overeat, and it is statistically clear that an individual is more at risk from chronic health conditions than from a commercial air accident.2 Nevertheless, many in our society worry more about an aviation accident than they do about the risks of smoking or overeating.
It is worthwhile to clarify the difference between “risk” and “hazard.” Many people consider these terms to be synonymous, yet they are not. Risk expresses not only the potential for an undesired consequence but the probability that such a consequence will occur. In contrast, hazard expresses the potential for an undesired consequence but without an estimate of how likely it is to occur.3 Most of us, believing we are reflecting on risk, are really focused on the hazard. As an example, the authors of Freakonomics outline that when considering the risks of a school-age girl playing at the home of friends, whose parents own either a swimming pool or a handgun, most parents believe the risk is lower if the girl plays in the home whose parents own a swimming pool.4 Even with this example, risk analysis is often further confounded. To produce a more accurate analysis, the emotional aspect of risk needs to be understood. Sandman identifies that the outrage principle is operative when people contemplate outrage as part of their risk analysis.5
I believe this understanding—or perception of understanding (really a quality of caring)—is quite important for our patients and yet is executed poorly by many physicians. Morgan outlined clearly that any risk analysis needs to place the risk in question on a grid stratified by two important concepts that affect an individual’s response to risk decision making. As shown in Figure 1-1, the two axes are controllable/uncontrollable and observable/not observable. These two concepts provide further insight into how an individual responds to risk.6 As an example, when we explore a common fear (risk) in today’s culture (such as terrorism), most of us dread it. We cannot control the events surrounding a terrorist act, and we know little about it, which places it in the upper right-hand (fearful) quadrant of the risk grid (Fig. 1-1).When we consider regional anesthesia risks, we must keep in mind that many patients and their families dread needles and surgery and often do not understand regional anesthesia. Thus, it is not difficult to imagine one of our poorly communicating colleagues carrying out regional anesthesia in an anxious patient and thereby relating to the individual in the upper right-hand (fearful) quadrant of the risk grid. It is also not difficult to imagine one of our chronic pain patients experiencing an uncontrollable fear of their pain state and being in the upper right-hand quadrant of the risk grid, in that chronic pain is largely unobservable.

FIGURE 1-1. Risk space has axes that correspond roughly to a hazard’s “dreadfulness” and to the degree to which it is understood. Risks in the upper right-hand quadrant of this space are most likely to provoke calls for government regulation. (Modified after Morgan MG. Risk analysis and management. Sci Am 1993;269:32–41.)
If we go back in time for another perspective on risk analysis, de Gondi (an early French statesman) likely said it best. He articulated the essence of all risk analysis as7 “That which is necessary is never a risk.” During any risk (decision) analysis, the real issue is to come to agreement on what is “necessary,” what specific risks (hazard plus the incidence) accompany the prescribed technique, and any alternatives that should be considered. As a result of increased subspecialization in medicine in Western countries, the balance of risk and benefit continues to be perplexing. Increasingly, subspecialists have only a few of the facts available for a specific patient’s risk/benefit question, making a patient-focused risk analysis difficult. I believe this is a fundamental issue as anesthesiologists seek to balance risk and benefit for patients (Fig. 1-2).
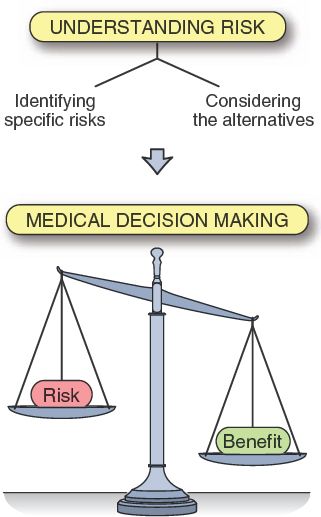
FIGURE 1-2. Understanding risk improves medical decision making. By considering the specific components of risk and determining if the proposed procedure is necessary, we can thereby optimize medical decision making.
For this reason, as anesthesiologists interested in subspecialty areas of anesthesia, we must remain engaged in all of medicine, not just the technical features of our subspecialty. For example, becoming technical experts in regional blocks and ultrasound and limiting our understanding of the whole of medical practice is a seductive trap we must avoid. Avoiding this trap is not a unique idea. Rather, it has been expostulated by many, including the late Roy Vandam during his 1979 Rovenstine lecture in San Francisco at the American Society of Anesthesiologists’ annual meeting. Dr. Vandam reflected on Dr. Rovenstine and stated8: “Rovenstine was truly a clinician who cared for patients in a total manner, considering all of the ramifications, because that is what treatment of pain is all about.” Pain management is not the only area of practice that demands our continued clinical experience. Regional anesthesia application in surgical patients also requires this comprehensive knowledge. We as physicians are skilled at making decisions, and this ability in its most developed form is the end result of truly understanding risk (Fig. 1-2).
Returning to the dilemma of increased subspecialization within medicine and reflecting on the decision analysis used to guide a judgment to operate, the risk/benefit judgment for a surgical procedure has typically already been made by a surgical colleague prior to the anesthesiologist examining the patient and assessing that patient’s anesthetic risks. This confounds a real balancing of risk and benefit for the patient, unless the anesthesiologist maintains a true interaction and open communication with the surgical colleague. Thus, anesthesiologists must determine which anesthetic should be prescribed for the patient, most often without a complete understanding of expected surgical benefit. The dilemma of risk/benefit analysis “cuts both ways”: from surgeon to anesthesiologist and anesthesiologist to surgeon.
An even more interesting modifying influence on our risk analysis is observed as we consider a concept termed risk homeostasis. A Canadian psychologist, Gerald Wilde, developed the concept of societal risk homeostasis after investigating data on traumatic injury and death during the last century.9 He and others postulate that as activities become safer in some area of our life, we extend risk in other areas and keep the overall risk (mortality in their studies) at approximately the same level.10 Teleologically, it is as if we are endowed with a hypothalamic risk feedback loop that keeps our overall risk of traumatic mortality at a specific set point.
For example: “It was in 1987 that Daimler-Benz showed off microprocessor-controlled brakes on a Detroit parking lot that had been soaped on one side and not on the other. The cars stopped beautifully on the soaped parking lot without swerving, and it is reported that the automotive reporters went away convinced that the new anti-lock brakes were the best automotive idea since safety glass. Customers were also impressed, and today most cars carry anti-lock brakes, adding about $500 per car”.10 It appears from National Highway Traffic Safety Administration data that antilock braking system-equipped cars showed a decline in some accidents, yet the overall accident rate went up. Thus, no overall benefit to automobile drivers and passengers resulted from this technological advance.11 Another example is Wilde’s opinion that as downhill skiing has seen safety advances (helmets) added to the sport, deaths have not decreased due to skiers embracing behavior that keeps the risk at a steady level.12
This concept makes me wonder what intraoperative, perioperative, and chronic pain care risk behavior we and our surgical colleagues have embraced with the advent of ever more sophisticated monitors such as pulse oximetry and end-tidal carbon dioxide monitors, “safer” intraoperative anesthetic regimens, our increasing use of continuous neuraxial infusions of local anesthetics via sophisticated continuous-flow pumps, and invasive neuraxial instrumentation in our chronic pain patients. Are we impacted by the concept of risk homeostasis in our anesthetic practice? For example, could it be that our postoperative evaluation of motor and sensory block of patients receiving continuous analgesia regimens is less vigorous than it was when the techniques were more difficult to carry out and hence less common? It is my belief that opportunities for effective clinical intervention (rescue) from epidural hematomas have been missed due to the attribution of motor weakness during the first postoperative night to the “epidural running,” even in a setting with the infusion containing only opioid. Another example of risk homeostasis might be anesthesiologists being less prepared to treat local anesthetic systemic toxicity than in the past, in that patients are increasingly outpatients and simply do not demand everything our typically more compromised inpatients require. Could it be that even with advantages of lipid rescue from local anesthetic toxicity, the solution is often “too far” from the patient care area to be ideal?13 I believe we all need to consider the possibility that risk homeostasis does affect our anesthetic and pain practices (see Box 1-2).
BOX 1-2 Risk Homeostasis
As we decrease risk and consequently make one part of our practice safer, we frequently extend risk in other facets of patient management. Overall, risk remains unchanged.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


