Shireen Ahmad
The most recent update available from the Centers for Disease Control and Prevention regarding Ambulatory Surgery in the United States from 2006 indicates that outpatient surgery visits in the United States increased from 20.8 million visits in 1996 to 34.7 million in 2006. Additionally, the proportion of outpatient surgeries has increased from one-half to two-thirds of all surgeries over the same time period (1). The most common ambulatory procedures performed were endoscopy and cataract surgery, both typically performed under monitored anesthesia care (MAC). Therefore, it is important for anesthesiologists to be able to formulate an appropriate anesthetic plan. This includes an expeditious return of consciousness without significant side effects, thereby allowing the timely discharge of patients undergoing ambulatory procedures. This chapter will discuss the principles applied in MAC, the techniques and common medications used in ambulatory anesthesia, and a brief introduction to office-based anesthesia.
I. Monitored Anesthesia Care
A. Terminology
According to the American Society of Anesthesiologists (ASA) position statement, MAC is a specific anesthesia service for a diagnostic or therapeutic procedure and does not describe the continuum of depth of sedation (2). Indications for MAC include the type of procedure, the patient’s clinical condition, and the potential need to convert to a general or regional anesthetic (2). Furthermore, it includes all aspects of anesthetic care, including a preprocedure visit, intraprocedure care, and postprocedure recovery management (2).
The anesthesia provider must be prepared and qualified to convert to general anesthesia if necessary (3). If the patient loses consciousness and the ability to respond purposefully, the anesthesia care is a general anesthetic, irrespective of whether airway instrumentation is required (2). ASA standard monitoring, which includes electrocardiography (ECG), pulse oximetry, noninvasive blood pressure, and more recently end-tidal carbon dioxide (ETCO2) monitoring, must be used for every anesthetic including MAC.
B. Preoperative Assessment
Patients scheduled for MAC should receive a preoperative assessment similar to any other preoperative patient. MAC is unique in that it also requires an element of cooperation on the part of the patient. It is important for the patient to accept the possibility to some degree of awareness during the procedure, to tolerate positioning required for surgery, and in some instances, to be able to communicate with the surgeon or proceduralist.

Patients scheduled for MAC should receive a preoperative assessment similar to any other preoperative patient.
C. Techniques of Monitored Anesthesia Care
Successful MAC involves the use of combinations of anesthetic agents. Typically, a combination of a sedative hypnotic and an analgesic agent is used in dosages that vary depending on the goals of the anesthetic and the requirements of the procedure. Medications with minimal side effects and short duration of action are preferable in ambulatory anesthesia, where efficiency and rapid recovery are highly desirable.
D. Pharmacologic Basis of Monitored Anesthesia Techniques: Optimizing Drug Administration
Pharmacokinetics and pharmacodynamics are important to consider when selecting medications for any anesthetic. Simply defined, pharmacokinetics is what the body does to the drug, as opposed to pharmacodynamics, which is the effect of the drug on the body (4). Knowledge of this information is essential in order to select the appropriate medications for specific procedures and individual patients. Many anesthetic drugs are administered as a bolus. However, it is generally preferable to deliver the drugs in smaller doses or as titratable infusions that allow the maintenance of a suitable therapeutic level of drug in the patient, thereby enhancing safety (5). Furthermore, patients require smaller amounts of drug during infusions compared with bolus dosing, which affects both recovery time and resource utilization (6). A more thorough discussion of the principles of pharmacokinetics and pharmacodynamics can be found in Chapter 7.

Patients require smaller amounts of drug during infusions compared with bolus dosing, which affects both recovery time and resource utilization.
E. Distribution, Elimination, Accumulation, and Duration of Action
Elimination Half-life
Elimination half-life is the time taken for a drug to lose half of its pharmacologic or physiologic activity. It is significant only if elimination is the exclusive route for the decline in plasma drug concentration. Therefore, this parameter is only useful in single compartment models, which do not typically apply to the human body.
Context-sensitive Half-time
The context-sensitive half-time is a more relevant parameter, and it is defined as the time required for plasma drug concentration to decrease by 50% after discontinuing an infusion of a specific duration (Fig. 25-1) (7). At the beginning of an infusion, plasma drug levels are decreased primarily by distribution to other body compartments as opposed to elimination. After the infusion is discontinued, drug that has been distributed to other compartments will return to the central plasma compartment for elimination. Factors that affect context-sensitive half-time include elimination mechanisms and propensity for distribution. A lipophilic drug, such as fentanyl, is much more likely to be transported into the tissues and to re-emerge into the plasma compartment after the infusion is stopped, resulting in a prolonged context-sensitive half-time. This phenomenon is unlike that of remifentanil, which is rapidly hydrolyzed by plasma esterases and has a smaller amount of drug available for transport into tissues and a significantly shorter context-sensitive half-time.
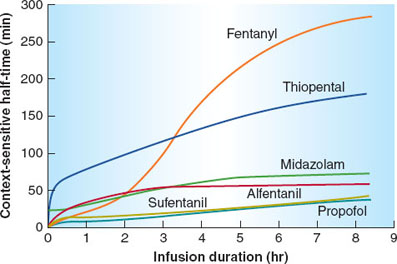
FIGURE 25-1 Context-sensitive half-time as a function of infusion duration. These data were generated from the computer model of Hughes et al. It can be seen that the context-sensitive half-time of propofol demonstrates a minimal increase as the duration of the infusion increases. Also note that for infusions of short duration, sufentanil has a shorter half-time than alfentanil. (From Hillier SC, Mazurek MS, Havidich, JE. Monitored anesthesia care. In: Barash PG, Cullen BF, Stoelting RK, et al. Clinical Anesthesia, 7th ed. Philadelphia: Lippincott Williams & Wilkins, 2013:827.)
How Does the Context-sensitive Half-time Relate to the Time of Recovery?
Context-sensitive half-time merely refers to the time it takes for the plasma concentration to decline by 50% after terminating an infusion. It may not have a direct correlation with the time required for an individual patient to awaken or recover from the infusion, which is a function of the time it takes for the drug to clear the brain compartment to a sufficient level to allow arousal.

Context-sensitive half-time merely refers to the time it takes for the plasma concentration to decline by 50% after terminating an infusion.
Effect-site Equilibration
The delay between drug administration and effect reflects the effect-site equilibration. It is important to observe the effects of the drugs prior to the administration of repeated doses to avoid oversedation.
F. Drug Interactions in Monitored Anesthesia Care
Because there is no intravenous agent that provides all of the desired qualities in an anesthetic, namely anxiolysis, amnesia, analgesia, and anesthesia, multiple medications are often combined to produce these characteristics. These agents potentiate one another. Therefore, it is important to administer smaller doses of each medication when they are given in combination with one another. This synergism applies not only to desired therapeutic effects of medications, but also to potentially dangerous side effects of these drugs.
G. Specific Drugs Used during Monitored Anesthesia Care
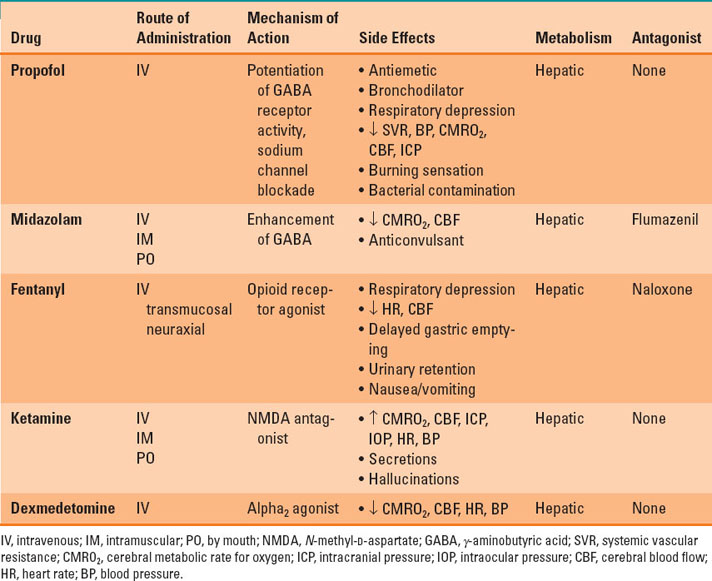
This section presents a brief description of the drugs most commonly used in MAC. For a more in-depth discussion of these medication classes, please refer to their dedicated chapters (see Chapters 9 and 10). Table 25-1 provides a succinct profile of several drugs commonly used in MAC.
Table 25-1 Profile of Drugs Frequently Used in Monitored Anesthesia Care
Propofol
Propofol is a short-acting, intravenous, sedative-hypnotic agent and is one of the most ubiquitous anesthetic drugs across all types of anesthesia. It is used for induction and maintenance of general anesthesia, for procedural sedation, and as a sedative for mechanically ventilated patients in the intensive care unit. Propofol has multiple mechanisms of action, including potentiation of γ-aminobutyric acid (GABA) receptor activity and sodium channel blockade. It has a favorable side-effect profile, possesses antiemetic and bronchodilator properties, and has a short context-sensitive half-time that is minimally affected by the duration of infusion. In addition to its desired therapeutic effects, propofol also decreases systemic vascular resistance, blood pressure (BP), cerebral metabolic rate for oxygen (CMRO2), cerebral blood flow (CBF), and intracranial pressure (ICP) and produces respiratory depression. Propofol is metabolized by the liver and excreted by the kidneys. Propofol is associated with a burning sensation at the injection site. However, a small dose of lidocaine alone or combined with propofol is the most effective strategy to attenuate this effect (8). Because propofol is prepared in a lipid emulsion, this presents the risk of bacterial contamination if the drug is not discarded within 6 hours of being withdrawn from the vial. Additionally, propofol contains an egg phospholipid as an emulsifier and should be avoided in patients with egg allergies.

Propofol is a short-acting, intravenous, sedative-hypnotic agent and is one of the most ubiquitous anesthetic drugs across all types of anesthesia.
Fospropofol
Fospropofol is a water-soluble prodrug form of propofol. It is metabolized by alkaline phosphatases to its active metabolite, propofol, and therefore has a slower onset. Potential advantages over propofol include less chance of bacterial contamination, less pain on injection, and lower risk of hyperlipidemia associated with long-term administration. Although fospropofol has been approved by the U.S. Food and Drug Administration for use during MAC, there are limited data on the safety and efficacy of the drug, and it is not commonly used in clinical practice at this time.

Benzodiazepines are also potent anticonvulsants and may be used to treat status epilepticus and seizures related to local anesthetic toxicity or alcohol withdrawal.
Benzodiazepines
Benzodiazepines, most commonly midazolam, are used prior to induction of most anesthetics to provide anxiolysis and amnesia. The therapeutic effects of midazolam are related to the enhancement of the effect of GABA on its receptors. The effects of benzodiazepines on the body include minimal respiratory depression when used alone and decreased CMRO2 and CBF, with no effect on ICP. Benzodiazepines are also potent anticonvulsants and may be used to treat status epilepticus and seizures related to local anesthetic toxicity or alcohol withdrawal. Midazolam is metabolized by the liver and subsequently excreted by the kidneys. In addition to the intravenous route, it can be administered intramuscularly, intranasally, or orally. The oral dose of midazolam is much higher than the intravenous dose due to poor oral bioavailability. Although midazolam has a short elimination half-life, larger doses may be associated with delayed emergence. For this reason, it is typically used in small doses at the beginning of an anesthetic to facilitate patient comfort through anxiolysis and amnesia, while sedation is maintained with a drug that has a more favorable recovery profile, such as propofol. Benzodiazepines offer an advantage over propofol, in that there is a specific benzodiazepine antagonist, flumazenil. However, the effects of midazolam frequently outlast the dose of flumazenil, resulting in resedation.

Intravenous opioid administration may induce skeletal muscle rigidity and chest wall rigidity that can be severe enough to make ventilation difficult when large doses are administered rapidly.
Opioids
The analgesia during MAC is typically provided by the injection of local anesthetic at the surgical site. However, opioids, most commonly fentanyl, are administered for additional analgesia and to improve the patient’s comfort. Opioids are administered by various routes, including oral, intramuscular, subcutaneous, transmucosal, neuraxial, and most commonly in anesthesia, intravenous. The mechanism of action of opioids is through an agonist action at specific opioid receptors in the central and peripheral nervous systems, decreasing the transmission of pain signals. Potential side effects of opioids include bradycardia, a dose-dependent respiratory depression, decreased CBF, delayed gastric emptying, increased urinary sphincter tone leading to failure to void, and most commonly, nausea and vomiting. Additionally, it is possible to induce skeletal muscle rigidity when large doses of opioids are administered rapidly. Chest wall rigidity can be severe enough to make ventilation difficult and, therefore, large doses should be avoided. It is also important to note that opioids alone do not provide amnesia.

Opioids alone do not provide amnesia.
Opioids are metabolized by the liver and excreted mainly in the urine. The differences in lipid solubility within this class of drugs account for varying pharmacokinetic profiles of individual opioids. Like benzodiazepines, opioids also have a specific antagonist. Naloxone can be given to reverse the respiratory effects of opioids. But it should be used judiciously due to the potential adverse side effects such as tachycardia and hypertension, as well as pulmonary edema.

Naloxone can precipitate tachycardia and hypertension when given to reverse the respiratory effects of opioids.
Ketamine
Ketamine is a phencyclidine derivative that produces intense analgesia and amnesia. Although small doses are often used as an adjunct in MAC, larger doses can be used to induce general anesthesia. Its primary mechanism of action is antagonism at the N-methyl-D-aspartate receptor. Ketamine can be administered by oral, intramuscular, or intravenous routes. Ketamine has bronchodilator properties, making it beneficial in asthmatic patients. It has minimal effect on respiration, in contrast to other intravenous sedatives and opioids. In addition to its therapeutic effects, ketamine is also associated with increased CMRO2, CBF, ICP, and stimulation of the sympathetic nervous system, resulting in increased heart rate (HR) and BP. For these reasons, ketamine may be a poor choice in patients with increased ICP or intraocular pressure and patients with coronary artery disease. Ketamine may have a paradoxical cardiac effect in patients with disease states associated with catecholamine depletion (e.g., septic shock), resulting in direct myocardial depression. Ketamine may also produce increased secretions, which are often managed with administration of an antisialagogue. The incidence of hallucinations with ketamine is minimized by administration of a benzodiazepine. Ketamine is metabolized in the liver to norketamine, which has approximately one-fifth the potency of ketamine and may contribute to lingering effects.

Ketamine and dexmedetomidine are the only drugs in the analgesic sedative armamentarium that do not suppress ventilatory drive.
Dexmedetomidine
Dexmedetomidine is an intravenous selective α2 receptor agonist that can be used to provide sedation. Its major benefit is that it has little effect on respiratory drive when used alone. Dexmedetomidine has no intrinsic amnestic properties. Side effects of dexmedetomidine include decreased CMRO2 and CBF, as well as a combination of decreased sympathetic outflow and increased vagal activity, commonly precipitating hypotension and bradycardia, which can be profound. Dexmedetomidine is extensively metabolized in the liver and excreted by the kidneys.
Amnesia during Sedation with Dexmedetomidine or Propofol
Because dexmedetomidine has no amnestic properties, it must be supplemented with a drug such as propofol or midazolam if amnesia is desirable.
H. Patient-controlled Sedation and Analgesia
Patient-controlled analgesia (PCA) is a familiar concept for management of postoperative pain. PCA has a favorable safety profile compared with intermittent larger boluses of analgesics as well as increased patient satisfaction with pain control compared with medical-provider analgesic administration. Patient-controlled sedation has been shown to be effective for use during procedural sedation (9). The cumbersome nature of the PCA pump and set up as well as a decreased margin of safety when dealing with anesthetic doses of medications rather than analgesic doses are the major limiting factors.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








