Key Concepts
 A pressure of 1000 psig indicates an E-cylinder that is approximately half full and represents 330 L of oxygen.
A pressure of 1000 psig indicates an E-cylinder that is approximately half full and represents 330 L of oxygen.
 The only reliable way to determine residual volume of nitrous oxide is to weigh the cylinder.
The only reliable way to determine residual volume of nitrous oxide is to weigh the cylinder.
 To discourage incorrect cylinder attachments, cylinder manufacturers have adopted a pin index safety system.
To discourage incorrect cylinder attachments, cylinder manufacturers have adopted a pin index safety system.
 A basic principle of radiation safety is to keep exposure “as low as reasonably practical” (ALARP). The principles of ALARP are protection from radiation exposure by the use of time, distance, and shielding.
A basic principle of radiation safety is to keep exposure “as low as reasonably practical” (ALARP). The principles of ALARP are protection from radiation exposure by the use of time, distance, and shielding.
 The magnitude of a leakage current is normally imperceptible to touch (<1 mA, and well below the fibrillation threshold of 100 mA). If the current bypasses the high resistance offered by skin, however, and is applied directly to the heart (microshock), current as low as 100 μA may be fatal. The maximum leakage allowed in operating room equipment is 10 μA.
The magnitude of a leakage current is normally imperceptible to touch (<1 mA, and well below the fibrillation threshold of 100 mA). If the current bypasses the high resistance offered by skin, however, and is applied directly to the heart (microshock), current as low as 100 μA may be fatal. The maximum leakage allowed in operating room equipment is 10 μA.
 To reduce the chance of two coexisting faults, a line isolation monitor measures the potential for current flow from the isolated power supply to the ground. Basically, the line isolation monitor determines the degree of isolation between the two power wires and the ground and predicts the amount of current that could flow if a second short circuit were to develop.
To reduce the chance of two coexisting faults, a line isolation monitor measures the potential for current flow from the isolated power supply to the ground. Basically, the line isolation monitor determines the degree of isolation between the two power wires and the ground and predicts the amount of current that could flow if a second short circuit were to develop.
 Almost all surgical fires can be prevented. Unlike medical complications, fires are a product of simple physical and chemistry properties. Occurrence is guaranteed given the proper combination of factors but can be eliminated almost entirely by understanding the basic principles of fire risk.
Almost all surgical fires can be prevented. Unlike medical complications, fires are a product of simple physical and chemistry properties. Occurrence is guaranteed given the proper combination of factors but can be eliminated almost entirely by understanding the basic principles of fire risk.
 Likely the most common risk factor for surgical fire relates to the open delivery of oxygen.
Likely the most common risk factor for surgical fire relates to the open delivery of oxygen.
 Administration of oxygen to concentrations of greater than 30% should be guided by clinical presentation of the patient and not solely by protocols or habits.
Administration of oxygen to concentrations of greater than 30% should be guided by clinical presentation of the patient and not solely by protocols or habits.
 The sequence of stopping gas flow and removal of the endotracheal tube when fire occurs in the airway is not as important as ensuring that both actions are performed quickly.
The sequence of stopping gas flow and removal of the endotracheal tube when fire occurs in the airway is not as important as ensuring that both actions are performed quickly.
 Before beginning laser surgery, the laser device should be in the operating room, warning signs should be posted on the doors, and protective eyewear should be issued. The anesthesia provider should ensure that the warning signs and eyewear match the labeling on the laser device as laser protection is specific to the type of laser.
Before beginning laser surgery, the laser device should be in the operating room, warning signs should be posted on the doors, and protective eyewear should be issued. The anesthesia provider should ensure that the warning signs and eyewear match the labeling on the laser device as laser protection is specific to the type of laser.
The Operating Room Environment: Introduction
Anesthesiologists, who spend more time in operating rooms than any other group of physicians, are responsible for protecting patients and operating room personnel from a multitude of dangers during surgery. Some of these threats are unique to the operating room. As a result, the anesthesiologist may be responsible for ensuring proper functioning of the operating room’s medical gases, fire prevention and management, environmental factors (eg, temperature, humidity, ventilation, and noise), and electrical safety. The role of the anesthesiologist also may include coordination of or assistance with layout and design of surgical suites, including workflow enhancements. This chapter describes the major operating room features that are of special interest to anesthesiologists and the potential hazards associated with these systems.
Safety Culture
Patients often think of the operating room as a safe place where the care given is centered around protecting the patient. Medical providers such as anesthesia personnel, surgeons, and nurses are responsible for carrying out several critical tasks at a fast pace. Unless members of the operating room team look out for one another, errors can occur. The best way of preventing serious harm to a patient is by creating a culture of safety. When the safety culture is effectively applied in the operating room, unsafe acts are stopped before harm occurs.
One tool that fosters the safety culture is the use of a surgical safety checklist. Such checklists are used prior to incision on every case and can include components agreed upon by the facility as crucial. Many surgical checklists are derived from the surgical safety checklist published by the World Health Organization (WHO). For checklists to be effective, they must first be used; secondly, all members of the surgical team should be engaged when the checklist is being used. Checklists are most effective when performed in an interactive fashion. An example of a suboptimally executed checklist is one that is read in entirety, after which the surgeon asks whether everyone agrees. This format makes it difficult to identify possible problems. A better method is one that elicits a response after each point; eg, “Does everyone agree this is John Doe?”, followed by “Does everyone agree we are performing a removal of the left kidney?”, and so forth. Optimal checklists do not attempt to cover every possibility but rather address only key components, allowing them to be completed in less than 90 seconds.
Some practitioners argue that checklists waste too much time; they fail to realize that cutting corners to save time often leads to problems later, resulting in a net loss of time. If safety checklists were followed in every case, significant reductions could be seen in the incidence of surgical complications such as wrong-site surgery, procedures on the wrong patient, retained foreign objects, and other easily prevented mistakes. Anesthesia providers are leaders in patient safety initiatives and should take a proactive role to utilize checklists and other activities that foster the safety culture.
Medical Gas Systems
The medical gases commonly used in operating rooms are oxygen, nitrous oxide, air, and nitrogen. Although technically not a gas, vacuum exhaust for waste anesthetic gas disposal (WAGD or scavenging) and surgical suction must also be provided and is considered an integral part of the medical gas system. Patients are endangered if medical gas systems, particularly oxygen, are misconfigured or malfunction. The main features of such systems are the sources of the gases and the means of their delivery to the operating room. The anesthesiologist must understand both these elements to prevent and detect medical gas depletion or supply line misconnection. Estimates of a particular hospital’s peak demand determine the type of medical gas supply system required. Design and standards follow National Fire Protection Association (NFPA) 99 in the United States and HTM 2022 in the United Kingdom.
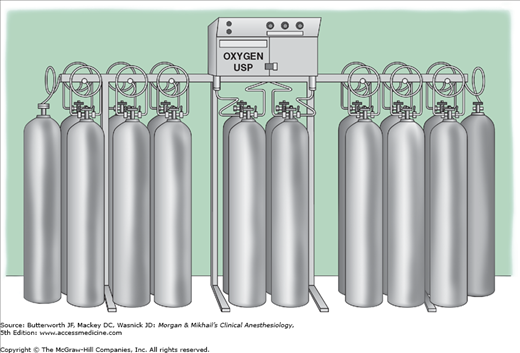
A reliable supply of oxygen is a critical requirement in any surgical area. Medical grade oxygen (99% or 99.5% pure) is manufactured by fractional distillation of liquefied air. Oxygen is stored as a compressed gas at room temperature or refrigerated as a liquid. Most small hospitals store oxygen in two separate banks of high-pressure cylinders (H-cylinders) connected by a manifold (Figure 2-1). Only one bank is utilized at a time. The number of cylinders in each bank depends on anticipated daily demand. The manifold contains valves that reduce the cylinder pressure (approximately 2000 pounds per square inch [psig]) to line pressure (55 ± 5 psig) and automatically switch banks when one group of cylinders is exhausted.
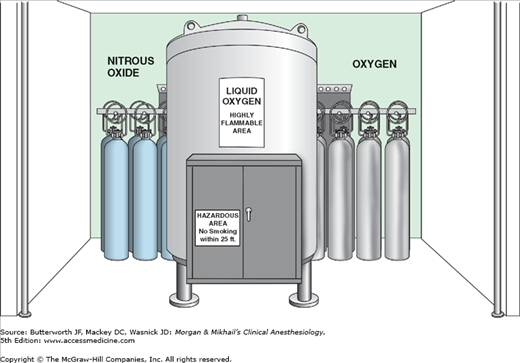
A liquid oxygen storage system (Figure 2-2) is more economical for large hospitals. Liquid oxygen must be stored well below its critical temperature of −119°C because gases can be liquefied by pressure only if stored below their critical temperature. A large hospital may have a smaller liquid oxygen supply or a bank of compressed gas cylinders that can provide one day’s oxygen requirements as a reserve. To guard against a hospital gas-system failure, the anesthesiologist must always have an emergency (E-cylinder) supply of oxygen available during anesthesia.
Most anesthesia machines accommodate E-cylinders of oxygen (Table 2-1). As oxygen is expended, the cylinder’s pressure falls in proportion to its content.  A pressure of 1000 psig indicates an E-cylinder that is approximately half full and represents 330 L of oxygen at atmospheric pressure and a temperature of 20°C. If the oxygen is exhausted at a rate of 3 L/min, a cylinder that is half full will be empty in 110 min. Oxygen cylinder pressure should be monitored before use and periodically during use. Anesthesia machines usually also accommodate E-cylinders for medical air and nitrous oxide, and may accept cylinders of helium. Compressed medical gases utilize a pin index safety system for these cylinders to prevent inadvertent crossover and connections for different gas types. As a safety feature of oxygen E-cylinders, the yoke has integral components made from Wood’s metal. This metallurgic alloy has a low melting point, which allows dissipation of pressure that might otherwise heat the bottle to the point of ballistic explosion. This pressure-relief “valve” is designed to rupture at 3300 psig, well below the pressure E-cylinder walls should be able to withstand (more than 5000 psig).
A pressure of 1000 psig indicates an E-cylinder that is approximately half full and represents 330 L of oxygen at atmospheric pressure and a temperature of 20°C. If the oxygen is exhausted at a rate of 3 L/min, a cylinder that is half full will be empty in 110 min. Oxygen cylinder pressure should be monitored before use and periodically during use. Anesthesia machines usually also accommodate E-cylinders for medical air and nitrous oxide, and may accept cylinders of helium. Compressed medical gases utilize a pin index safety system for these cylinders to prevent inadvertent crossover and connections for different gas types. As a safety feature of oxygen E-cylinders, the yoke has integral components made from Wood’s metal. This metallurgic alloy has a low melting point, which allows dissipation of pressure that might otherwise heat the bottle to the point of ballistic explosion. This pressure-relief “valve” is designed to rupture at 3300 psig, well below the pressure E-cylinder walls should be able to withstand (more than 5000 psig).
| Gas | E-Cylinder Capacity1 (L) | H-Cylinder Capacity1 (L) | Pressure1 (psig at 20°C) | Color (USA) | Color (International) | Form |
|---|---|---|---|---|---|---|
| O2 | 625-700 | 6000-8000 | 1800-2200 | Green | White | Gas |
| Air | 625-700 | 6000-8000 | 1800-2200 | Yellow | White and black | Gas |
| N2O | 1590 | 15,900 | 745 | Blue | Blue | Liquid |
| N2 | 625-700 | 6000-8000 | 1800-2200 | Black | Black | Gas |
Nitrous oxide is manufactured by heating ammonium nitrate (thermal decomposition). It is almost always stored by hospitals in large H-cylinders connected by a manifold with an automatic crossover feature. Bulk liquid storage of nitrous oxide is economical only in very large institutions.
Because the critical temperature of nitrous oxide (36.5°C) is above room temperature, it can be kept liquefied without an elaborate refrigeration system. If the liquefied nitrous oxide rises above its critical temperature, it will revert to its gaseous phase. Because nitrous oxide is not an ideal gas and is easily compressible, this transformation into a gaseous phase is not accompanied by a great rise in tank pressure. Nonetheless, as with oxygen cylinders, all nitrous oxide E-cylinders are equipped with a Wood’s metal yoke to prevent explosion under conditions of unexpectedly high gas pressure (eg, unintentional overfilling), particularly during fires.
Although a disruption in supply is usually not catastrophic, most anesthesia machines have reserve nitrous oxide E-cylinders. Because these smaller cylinders also contain nitrous oxide in its liquid state, the volume remaining in a cylinder is not proportional to cylinder pressure. By the time the liquid nitrous oxide is expended and the tank pressure begins to fall, only about 400 L of nitrous oxide remains. If liquid nitrous oxide is kept at a constant temperature (20°C), it will vaporize at the same rate at which it is consumed and will maintain a constant pressure (745 psig) until the liquid is exhausted.
 The only reliable way to determine residual volume of nitrous oxide is to weigh the cylinder. For this reason, the tare weight (TW), or empty weight, of cylinders containing a liquefied compressed gas (eg, nitrous oxide) is often stamped on the shoulder of the cylinder. The pressure gauge of a nitrous oxide cylinder should not exceed 745 psig at 20°C. A higher reading implies gauge malfunction, tank overfill (liquid fill), or a cylinder containing a gas other than nitrous oxide.
The only reliable way to determine residual volume of nitrous oxide is to weigh the cylinder. For this reason, the tare weight (TW), or empty weight, of cylinders containing a liquefied compressed gas (eg, nitrous oxide) is often stamped on the shoulder of the cylinder. The pressure gauge of a nitrous oxide cylinder should not exceed 745 psig at 20°C. A higher reading implies gauge malfunction, tank overfill (liquid fill), or a cylinder containing a gas other than nitrous oxide.
Because energy is consumed in the conversion of a liquid to a gas (the latent heat of vaporization), the liquid nitrous oxide cools. The drop in temperature results in a lower vapor pressure and lower cylinder pressure. The cooling is so pronounced at high flow rates that there is often frost on the tank, and pressure regulators may freeze.
The use of air is becoming more frequent in anesthesiology as the popularity of nitrous oxide and unnecessarily high concentrations of oxygen has declined. Cylinder air is medical grade and is obtained by blending oxygen and nitrogen. Dehumidified but unsterile air is provided to the hospital pipeline system by compression pumps. The inlets of these pumps must be distant from vacuum exhaust vents and machinery to minimize contamination. Because the critical temperature of air is −140.6°C, it exists as a gas in cylinders whose pressures fall in proportion to their content.
Although compressed nitrogen is not administered to patients, it may be used to drive some operating room equipment, such as saws, drills, and surgical handpieces. Nitrogen supply systems either incorporate the use of H-cylinders connected by a manifold or a wall system supplied by a compressor driven central supply.
A central hospital vacuum system usually consists of independent suction pumps, each capable of handling peak requirements. Traps at every user location prevent contamination of the system with foreign matter. The medical-surgical vacuum may be used for waste anesthetic gas disposal (WAGD) providing it does not affect the performance of the system. Medical vacuum receptacles are usually black in color with white lettering. A dedicated WAGD vacuum system is generally required with modern anesthesia machines. The WAGD outlet may incorporate the use of a suction regulator with a float indicator. The float should be maintained between the designated markings. Excess suction may result in inadequate patient ventilation, and insufficient suction levels may result in the failure to evaluate WAGD. WAGD receptacles and tubing are usually lavender in color.
Many surgical procedures are performed using laparoscopic or robotic-assisted techniques requiring insufflation of body cavities with carbon dioxide, an odorless, colorless, nonflammable and slightly acidic gas. Large cylinders containing carbon dioxide, such as M-cylinders or LK-cylinders, are frequently found in the operating room; these cylinders share a common size orifice and thread with oxygen cylinders and can be inadvertently interchanged.
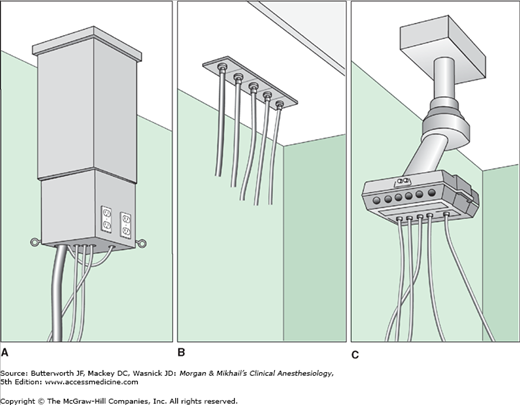
Medical gases are delivered from their central supply source to the operating room through a piping network. Pipes are sized such that the pressure drop across the whole system never exceeds 5 psig. Gas pipes are usually constructed of seamless copper tubing using a special welding technique. Internal contamination of the pipelines with dust, grease, or water must be avoided. The hospital’s gas delivery system appears in the operating room as hose drops, gas columns, or elaborate articulating arms (Figure 2-3). Operating room equipment, including the anesthesia machine, interfaces with these pipeline system outlets by color-coded hoses. Quick-coupler mechanisms, which vary in design with different manufacturers, connect one end of the hose to the appropriate gas outlet. The other end connects to the anesthesia machine through a noninterchangeable diameter index safety system fitting that prevents incorrect hose attachment.
Figure 2-3
Typical examples of (A) gas columns, (B) ceiling hose drops, and (C) articulating arms. One end of a color-coded hose connects to the hospital medical gas supply system by way of a quick-coupler mechanism. The other end connects to the anesthesia machine through the diameter index safety system.
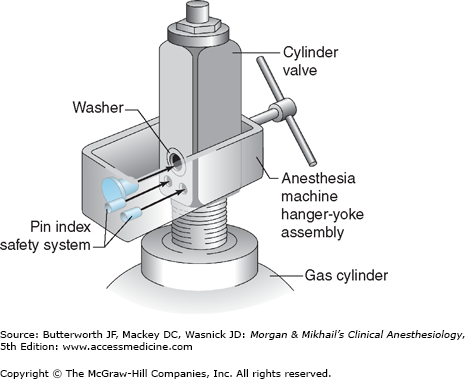
E-cylinders of oxygen, nitrous oxide, and air attach directly to the anesthesia machine.  To discourage incorrect cylinder attachments, cylinder manufacturers have adopted a pin index safety system. Each gas cylinder (sizes A-E) has two holes in its cylinder valve that mate with corresponding pins in the yoke of the anesthesia machine (Figure 2-4). The relative positioning of the pins and holes is unique for each gas. Multiple washers placed between the cylinder and yoke, which prevent proper engagement of the pins and holes, have unintentionally defeated this system. The pin index safety system is also ineffective if yoke pins are damaged or the cylinder is filled with the wrong gas.
To discourage incorrect cylinder attachments, cylinder manufacturers have adopted a pin index safety system. Each gas cylinder (sizes A-E) has two holes in its cylinder valve that mate with corresponding pins in the yoke of the anesthesia machine (Figure 2-4). The relative positioning of the pins and holes is unique for each gas. Multiple washers placed between the cylinder and yoke, which prevent proper engagement of the pins and holes, have unintentionally defeated this system. The pin index safety system is also ineffective if yoke pins are damaged or the cylinder is filled with the wrong gas.
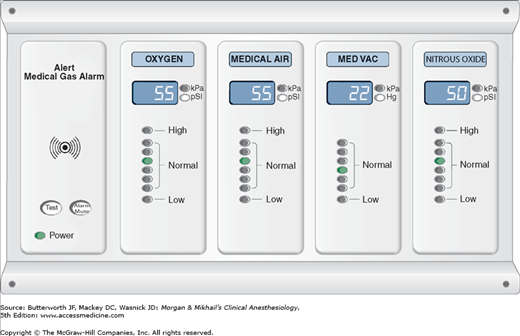
The functioning of medical gas supply sources and pipeline systems is constantly monitored by central and area alarm systems. Indicator lights and audible signals warn of changeover to secondary gas sources and abnormally high (eg, pressure regulator malfunction) or low (eg, supply depletion) pipeline pressures (Figure 2-5).
Modern anesthesia machines and anesthetic gas analyzers continuously measure the fraction of inspired oxygen (FiO2). Analyzers have a variable threshold setting for the minimal FiO2 but should be configured to prevent disabling this alarm. The monitoring of FiO2 does not reflect the oxygen concentration distal to the monitoring port and should not be used to reference the oxygen concentration within devices such as endotracheal tubes or at the distal tip of the tube. Due to gas exchange, flow rates, and shunting a marked difference can exist between the monitored FiO2 and oxygen concentration at the tissue level.
Environmental Factors in the Operating Room
The temperature in most operating rooms seems uncomfortably cold to many conscious patients and, at times, to anesthesiologists. However, scrub nurses and surgeons stand in surgical garb for hours under hot operating room lights. As a general principle, the comfort of operating room personnel must be reconciled with patient care. Hypothermia has been associated with an increased incidence of wound infection, greater intraoperative blood loss (impaired coagulation assessed by thromboelastography), and prolonged hospitalization (see Chapter 52).
In past decades, static discharges were a feared source of ignition in an operating room filled with flammable anesthetic vapors. Now humidity control is more relevant to infection control practices. Optimally humidity levels in the operating room should be maintained between 50% and 55%. Below this range the dry air facilitates airborne motility of particulate matter, which can be a vector for infection. At high humidity, dampness can affect the integrity of barrier devices such as sterile cloth drapes and pan liners.