Key Concepts
 Induction of anesthesia in patients receiving long-term levodopa therapy may result in either marked hypotension or hypertension.
Induction of anesthesia in patients receiving long-term levodopa therapy may result in either marked hypotension or hypertension.
 In patients with multiple sclerosis, increases in body temperature cause exacerbation of symptoms.
In patients with multiple sclerosis, increases in body temperature cause exacerbation of symptoms.
 The major risk of anesthesia in patients with autonomic dysfunction is severe hypotension, compromising cerebral and coronary blood flow.
The major risk of anesthesia in patients with autonomic dysfunction is severe hypotension, compromising cerebral and coronary blood flow.
 Autonomic hyperreflexia should be expected in patients with lesions above T6 and can be precipitated by surgical manipulations.
Autonomic hyperreflexia should be expected in patients with lesions above T6 and can be precipitated by surgical manipulations.
 The most important interaction between anesthetic agents and tricyclic antidepressants is an exaggerated response to both indirect-acting vasopressors and sympathetic stimulation.
The most important interaction between anesthetic agents and tricyclic antidepressants is an exaggerated response to both indirect-acting vasopressors and sympathetic stimulation.
Anesthesia for Patients with Neurologic & Psychiatric Diseases: Introduction
Patients with vascular and nonvascular neurologic diseases and/or psychiatric disorders are frequently encountered by anesthesia staff. Anesthesiologists must have a basic understanding of the major neurologic and psychiatric disorders and their drug therapy. Failure to recognize potential adverse anesthetic interactions may result in avoidable perioperative morbidity.
Cerebrovascular Disease
Patients with diagnosed cerebrovascular disease typically have a history of transient ischemic attacks (TIAs) or stroke. Patients with TIAs undergoing surgery for other indications have an increased risk of perioperative stroke. Asymptomatic carotid bruits occur in up to 4% of patients older than age 40 years, but do not necessarily indicate significant carotid artery obstruction. Fewer than 10% of patients with completely asymptomatic bruits have hemodynamically significant carotid artery lesions. An asymptomatic carotid bruit may not increase the risk of stroke following surgery, but increases the likelihood of coexisting coronary artery disease. Moreover, the absence of a bruit does not exclude significant carotid obstruction.
The risk of perioperative stroke increases with patient age and varies with the type of surgery. The overall risk of stroke associated with surgery is low, but is greater in patients undergoing cardiovascular surgery. Rates of stroke after general anesthesia and surgery range from 0.08% to 0.4%. Even in patients with known cerebrovascular disease, the risk is only 0.4% to 3.3%. Patients at greatest risk of postoperative stroke are those undergoing open heart procedures for valvular disease, coronary artery disease with ascending aortic atherosclerosis, and diseases of the thoracic aorta. Stroke following open heart surgery is usually due to embolism of air, clots, or atheromatous debris. In one study, 6.1% of patients experienced an adverse neurological outcome following cardiac surgery. Stroke following thoracic aortic surgery may be due to emboli or ischemia secondary to prolonged circulatory arrest or a clamp placed close to the origin of the carotid artery.
The pathophysiology of postoperative strokes following noncardiovascular surgery is less clear, but may involve severe sustained hypotension or hypertension. Hypotension with severe hypoperfusion can result in so-called “watershed” zone infarctions or thrombosis of cerebral arteries, whereas hypertension can result in intracerebral hemorrhage (hemorrhagic stroke). Sustained hypertension can disrupt the blood-brain barrier and promote cerebral edema. Widened pulse pressure (>80 mm Hg) can produce endothelial vessel injury, potentially resulting in cerebral hypoperfusion or embolism. Perioperative atrial fibrillation can likewise lead to atrial clot formation and cerebral embolism. The period of time during which anesthesia and surgery should best be avoided following a stroke has not been determined. Abnormalities in regional blood flow and metabolic rate usually resolve after 2 weeks, whereas alterations in CO2 responsiveness and the blood-brain barrier may require more than 4 weeks. However, urgent surgery is performed for acute intracranial hemorrhage, symptomatic carotid disease, and cardiac sources of emboli.
Patients with TIAs have a history of transient (<24 h) impairment, and, by definition, no residual neurologic impairment. These attacks are thought to result from emboli of fibrin-platelet aggregates or atheromatous debris from plaques in extracranial vessels. Unilateral visual impairment, numbness or weakness of an extremity, or aphasia is suggestive of carotid disease, whereas bilateral visual impairment, dizziness, ataxia, dysarthria, bilateral weakness, or amnesia is suggestive of vertebral-basilar disease. Patients with TIAs have a 30% to 40% chance of developing a frank stroke within 5 years; 50% of these strokes occur within the first year. Patients with TIAs should not undergo any elective surgical procedure without an adequate medical evaluation that generally includes at least noninvasive (Doppler) flow and imaging studies. The presence of an ulcerative plaque of greater than 60% occlusion is generally an indication for carotid endarterectomy or endovascular intervention.
Preoperative assessment requires neurologic and cardiovascular evaluations. The type of stroke, the presence of neurologic deficits, and the extent of residual impairment should be determined. Thromboembolic strokes usually occur in patients with generalized atherosclerosis. Most patients are elderly and have comorbid conditions, such as hypertension, hyperlipidemia, and diabetes. Coexisting coronary artery disease and renal impairment are common. Following nonhemorrhagic strokes or TIAs, many patients are placed on long-term warfarin and/or antiplatelet therapy. Management of antiplatelet therapy and antithrombotic therapy should be reviewed by the anesthesia, primary care, and surgical teams to determine the risk/benefit of the discontinuation or maintenance of such therapy perioperatively. Other systemic diseases, such as diabetes, hypertension, coronary artery disease, heart failure, and chronic obstructive lung disease frequently manifest in the patient with cerebrovascular disease.
Patients may present for surgery following embolic, thrombotic, and hemorrhagic strokes.
Management of the patient following acute embolic stroke is directed toward the embolic source. Cardiac surgery is performed to remove atrial myxomas. Systemic emboli can also be produced from endocarditic vegetations, as well as from degenerated heart valves and intracardiac thrombus.
Patients with acute strokes secondary to carotid occlusive disease present for carotid endarterectomy and endovascular procedures. When an awake carotid endarterectomy is undertaken, the patient serves as a monitor of the adequacy of cerebral blood flow during application of vessel clamps to facilitate the surgical repair. When general anesthesia is used electroencephalography, evoked potentials, carotid stump pressure, cerebral infrared spectroscopy, transcranial Doppler, and surgeon subjective sense of collateral back flow are all used to estimate the adequacy of cerebral oxygen delivery during cross clamp. When monitors or lack of appropriate patient response indicate hypoperfusion, the surgeon places a shunt to deliver blood to the brain around the cross-clamped vessel. Even with adequate cerebral blood flow, perioperative stroke can occur during carotid surgery secondary to emboli.
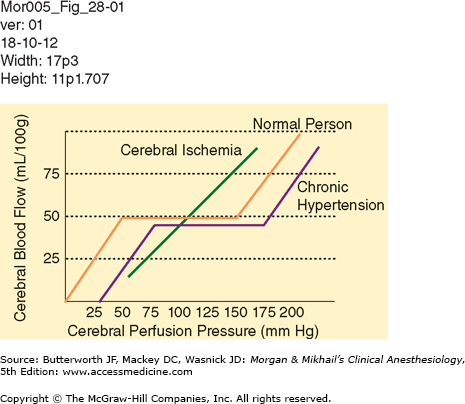
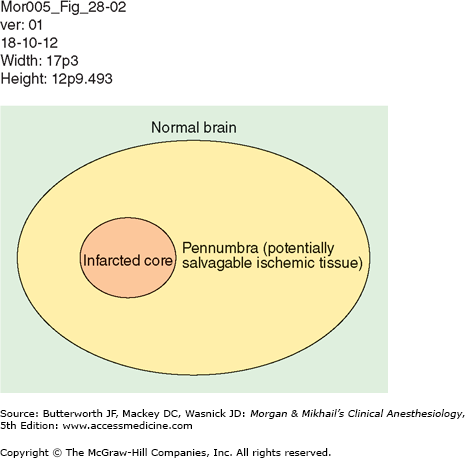
Management of patients following thrombotic or hemorrhagic stroke for nonneurological surgery must be individualized. Cerebral autoregulation of blood flow may fail, leaving flow directly dependent upon cerebral perfusion pressure (Figure 28-1). The penumbra of potentially salvageable neurologic tissue may therefore be very sensitive to injury from the effects of both hypotension and hypertension (Figure 28-2).
Patients taken to surgery following administration of thrombolytic therapy are at risk of cerebral hemorrhage, and tighter blood pressure control may be indicated to mitigate the possibility of cerebral bleeding.
Patients with intracerebral hemorrhage or traumatic brain injury undergo evacuation of hematoma and decompressive craniectomy. These patients usually require invasive arterial pressure monitoring to facilitate blood pressure management in settings where cerebral autoregulation is likely deranged (Figure 28-1). Hypertension is frequently treated with intravenous vasodilators and β-blockers. Subarachnoid hemorrhage is discussed in Chapter 27.
Patients with intracranial mass lesions present to surgery with both malignant and nonmalignant lesions. Such patients frequently present to their primary care physicians with complaints of headache, vision disturbance, or seizures. Radiologic studies confirm the presence of a lesion, and initial treatment is aimed at decreasing cerebral edema with dexamethasone. Electrolytes should be reviewed perioperatively in all patients undergoing cranial surgery, as both hyponatremia and hypernatremia can develop secondary to cerebral salt wasting, inappropriate antidiuretic hormone secretion, or central diabetes insipidus (Table 28-1). Patients with altered mentation preoperatively may likewise be dehydrated. Hyperglycemia secondary to steroid use is frequently seen.
| Condition | Serum Sodium Concentration | Plasma Volume | Serum Osmolality | Urine Sodium Concentration | Urine Osmolality | Treatment |
|---|---|---|---|---|---|---|
| SIADH | Low | Normal or increased | Low | High | High | Fluid restriction |
| CSWS | Low | Decreased | Normal or high | High | Normal or high | Isotonic or hypertonic saline |
| DI | High | Decreased | High | Normal | Low | Hypotonic saline + vasopressin |
Seizure Disorders
Seizures represent abnormal synchronized electrical activity in the brain. They may be a manifestation of an underlying central nervous system disease, a systemic disorder, or idiopathic. Potential underlying mechanisms are thought to include (1) loss of inhibitory activity, (2) enhanced release of excitatory amino acids, and (3) enhanced neuronal firing due to abnormal voltage-mediated Ca2+ currents. Up to 2% of the population may experience a seizure in their lifetime. Epilepsy is a disorder characterized by recurrent paroxysmal seizure activity. Healthy individuals who experience an isolated nonrecurrent seizure are not considered to have epilepsy.
Seizure activity may be localized to a specific area in the brain or may be generalized. Moreover, initially localized (focal) seizures can subsequently spread, becoming generalized. A simple classification scheme is presented in Table 28-2. Partial seizures (also called focal) are clinically manifested by motor, sensory, autonomic, or psychiatric symptoms, depending on the cortical area affected. Focal seizures associated with impairment in consciousness are termed “complex partial” (psychomotor or temporal lobe) seizures. Generalized seizures characteristically produce bilaterally symmetric electrical activity without local onset. They result with or without abnormal motor activity, loss of consciousness, or both. Generalized activity resulting in isolated, transient lapses in consciousness are called absence (petit mal) seizures. Other generalized seizures are usually classified according to the type of motor activity. Tonic-clonic (grand mal) seizures are most common and are characterized by a loss of consciousness followed by clonic and then tonic motor activity.
Anesthetic evaluation should focus primarily on the underlying disorder and secondarily on the seizures. One should determine the cause and type of seizure activity and the drugs with which the patient is being treated. Seizures in adults are most commonly due to structural brain lesions (head trauma, tumor, degeneration, or stroke) or metabolic abnormalities (uremia, hepatic failure, hypoglycemia, hypocalcemia, drug toxicity, or drug/alcohol withdrawal). Idiopathic seizures occur most often in children, but may persist into adulthood. Characterization of the type of seizure is important in detecting such activity perioperatively. Seizures—particularly grand mal seizures—are serious complicating factors in surgical patients and should be treated promptly to prevent musculoskeletal injury, hypoventilation, hypoxemia, and aspiration of gastrointestinal content. Even partial seizures can progress to grand mal seizures. If a seizure occurs, maintaining an open airway and adequate oxygenation are the first priorities. Intravenous propofol (50-100 mg), phenytoin (500-1000 mg slowly), or a benzodiazepine such as diazepam (5-10 mg) or midazolam (1-5 mg) can be used to terminate the seizure.
Most patients with seizure disorders receive antiepileptic drugs preoperatively (Table 28-3). Antiseizure medications should be continued throughout the perioperative period to maintain therapeutic levels.
| Drug | Mechanism of Action | Major Side Effects | Comments |
|---|---|---|---|
| Phenytoin | Blocks voltage sensitive Na+ channels |
|
|
| Phenobarbital |
| Sedation, dizziness, confusion, excitement | |
| Carbamazepine | Blocks voltage sensitive Na+ channels | Allergic reactions | Introduced slowly |
| Oxycarbamazepine |
| Titrated to side effects | |
| Valproic acid |
|
|
|
| Lamotrigine | Blocks voltage sensitive Na+ channels | Allergic reactions | Non-sedative |
| Ethosuximide |
|
| |
| Vigabatrine |
| Visual field defects | |
| Topiramate | Potentiates GABAergic inhibition |
| Pulmonary embolism |
| Gabapentin |
| Somnolence, fatigue Ataxia | Used in intractable complex partial seizures |
In selecting anesthetic agents, drugs with epileptogenic potential should be avoided, most notably the general anesthetic enflurane (now of only historic interest). Theoretically, ketamine and methohexital (in small doses) can precipitate seizure activity. Hypothetically, large doses of atracurium, cisatracurium, or meperidine may be relatively contraindicated because of the reported epileptogenic potential of their respective metabolites, laudanosine, and normeperidine. Hepatic microsomal enzyme induction should be expected from chronic antiseizure therapy. Enzyme induction may increase the dose requirement and frequency of intravenous anesthetics and nondepolarizing neuromuscular blockers (NMBs) and may increase the risk for hepatotoxicity from halothane.
Degenerative & Demyelinating Diseases
Parkinson disease (PD) is a common movement disorder that typically afflicts individuals aged 50-70 years; it has a prevalence of 3% in the United States and Canada. This neurodegenerative disease is characterized by bradykinesia, rigidity, postural instability, and resting (pill-rolling) tremor. Additional frequently occurring findings include facial masking, hypophonia, dysphagia, and gait disturbances. Increasing problems with freezing, rigidity, and tremor eventually result in physical incapacitation. Early in the course of the disease, intellectual function is usually preserved, but declines in intellectual function may be severe as the disease progresses. PD is caused by a progressive loss of dopamine in the nigrostriatum. The severity of loss of dopamine correlates with the severity of bradykinesia. Concurrent with the loss of dopamine, the activity of the gamma-aminobutyric acid (GABA) nuclei in the basal ganglia increases, leading to an inhibition of thalamic and brainstem nuclei. Thalamic inhibition, in turn, suppresses the motor system in the cortex, resulting in the characteristic signs and symptoms.
Medical treatment is directed at controlling the symptoms. A variety of drugs may be used for mild disease, including the anticholinergic agents trihexyphenidyl, benztropine, and ethopropazine; the irreversible monoamine oxidase (MAO) inhibitors selegiline and rasagiline; and the antiviral drug, amantadine. Moderate to severe disease is typically treated pharmacologically with dopaminergic agents, either levodopa (a precursor of dopamine) or a dopamine-receptor agonist. Levodopa, which is given with a decarboxylase inhibitor to retard the peripheral breakdown of the drug (thereby increasing its central delivery and decreasing the dose of levodopa that is required to control symptoms), is the most effective therapy and is used to treat moderate to severe symptoms. Catechol methyltransferase inhibitors are also used to prevent the decarboxylation of levodopa. Levodopa is available in either an immediate or sustained-release formulation, with durations of action of 2-4 hr and 3-6 hr, respectively. Side effects include nausea, vomiting, dyskinesias, sudden sleepiness, cardiac irritability, and orthostatic hypotension. Dopamine receptor agonists include both ergot derivatives (bromocriptine, cabergoline, lisuride, and apomorphine) and nonergot derivatives (pramipexole and ropinirole). The nonergot derivatives have been shown to be beneficial when used as monotherapy in early PD; all dopamine receptor agonists are effective when given as combination therapy with levodopa in the treatment of moderate to severe PD. Side effects are similar to those found with the use of levodopa alone, and, in addition, include headache, confusion, and hallucinations. Pulmonary and retroperitoneal fibrosis, pleural effusion and thickening, Raynaud syndrome, and erythromyalgia are more common side effects with the use of ergot derivatives than with nonergot derivatives.
The surgical treatment of PD includes both ablative procedures (thalamotomy and pallidotomy), as well as electrical stimulation of the ventral intermediate nucleus of the thalamus, the globus pallidus internus, or the subthalamic nucleus. Pallidotomy is effective for treating the dyskinesia (70% to 90%), as well as the tremor, rigidity, bradykinesia, and gait symptoms (30% to 50%) of the disorder. Thalamotomy is most effective in treating the contralateral tremor, but not for the other symptoms of the disease, and has been largely replaced by the use of thalamic stimulation. The efficacy of deep brain stimulation of the thalamus is related to the effect on tremor; it has little to no effect on the other symptoms of PD. Subthalamic stimulation improves all of the primary symptoms of PD and decreases the amount of medication necessary for symptom relief. Bilateral stimulation has greater efficacy than unilateral stimulation. Some decrease in cognitive function may occur with this treatment, and, therefore, it should be used with caution in patients with cognitive impairment. The effects of globus pallidus internus stimulation are similar to those of pallidotomy with improvements in dyskinesia.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree