I. INTRODUCTION
A. “Telemedicine,” as defined by the American Telemedicine Association, is the use of medical information exchanged from one site to another via electronic communications to improve a patient’s clinical health status. Many forms of technology have been used to support telemedicine. Telemedicine and telehealth are often used interchangeably. Telehealth, in broad term, encompasses population health care management using telemedicine technology. Telemedicine is not a separate medical specialty, but is meant to supplement traditional models of health care as a delivery tool or system. Consultation is a cornerstone of modern hospital care, particularly in the intensive care unit (ICU). The focus of telemedicine in the ICU (“Tele-ICU”) is to supplement traditional ICU care by delivering collaborative, multiprofessional care using telemedicine technology. Goran defined tele-ICU as the provision of team-based critical care via a computer in combination with audio-visual or telecommunication systems.
B. Currently only 10% of hospitals in the United States use tele-ICU technology to provide intensive care. Given the aging of the U.S. population and a continued shortage of available intensivists nationally, tele-ICU has been utilized to bridge the gap between supply and demand for intensive care expertise. Tele-ICU can also expand access to intensivist expertise in rural and critical access hospitals alike. This chapter addresses a number of applications of telemedicine and electronic monitoring systems in the ICU, describing potential benefits as well as barriers of implementation.
II. TELE-ICU MODELS AND ORGANIZATION OF SERVICE
Grundy et al. published the first report of a clinical trial of tele-ICU in 1982. This was a teleconsultative model providing intermittent consultative advice to an inner-city hospital via two-way video and telephones. The report concluded that patients were more likely to survive when intensivists’ suggestions were implemented. The around-the-clock model whereby a remote intensivist provides telemedicine care to adult ICU patients was first reported in 2000 by Rosenfeld et al. Since then, three basic delivery models of tele-ICU have been popularized. Each of them can be used to deliver tele-ICU care recommendations successfully.
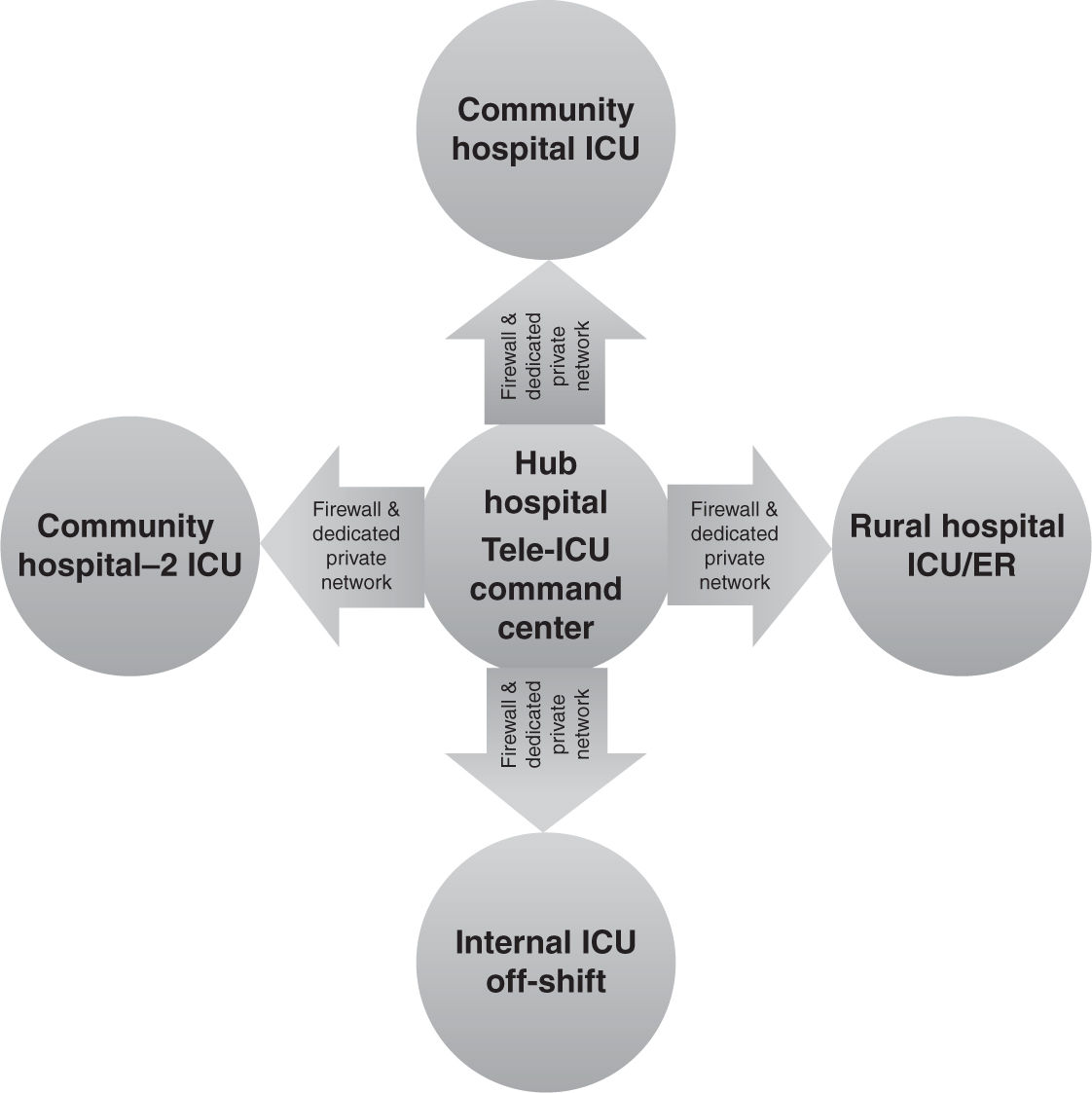
A. Centralized (Hub-and-Spoke) Model
The centralized model, also known as the hub-and-spoke model, is the most commonly utilized model for Tele-ICU (Fig. 40.1). In this model, tele-ICU intensivists and support personnel are located in a central location in an urban hospital (the hub) and provide tele-ICU interventions to several types of outlying units or rural/community hospitals (the spokes). The intensivists and support personnel work in shifts providing 24 × 7 (i.e., around the clock) monitoring and recommended interventions for these ICU patients. Recent reports suggestions that compliance with evidence-based ICU protocols is improved with this centralized tele-ICU care model. This model is typical with the commonly used term “electronic ICU” or “eICU care.” This model typically has higher setup and operational costs (in thousands of dollars per bed).
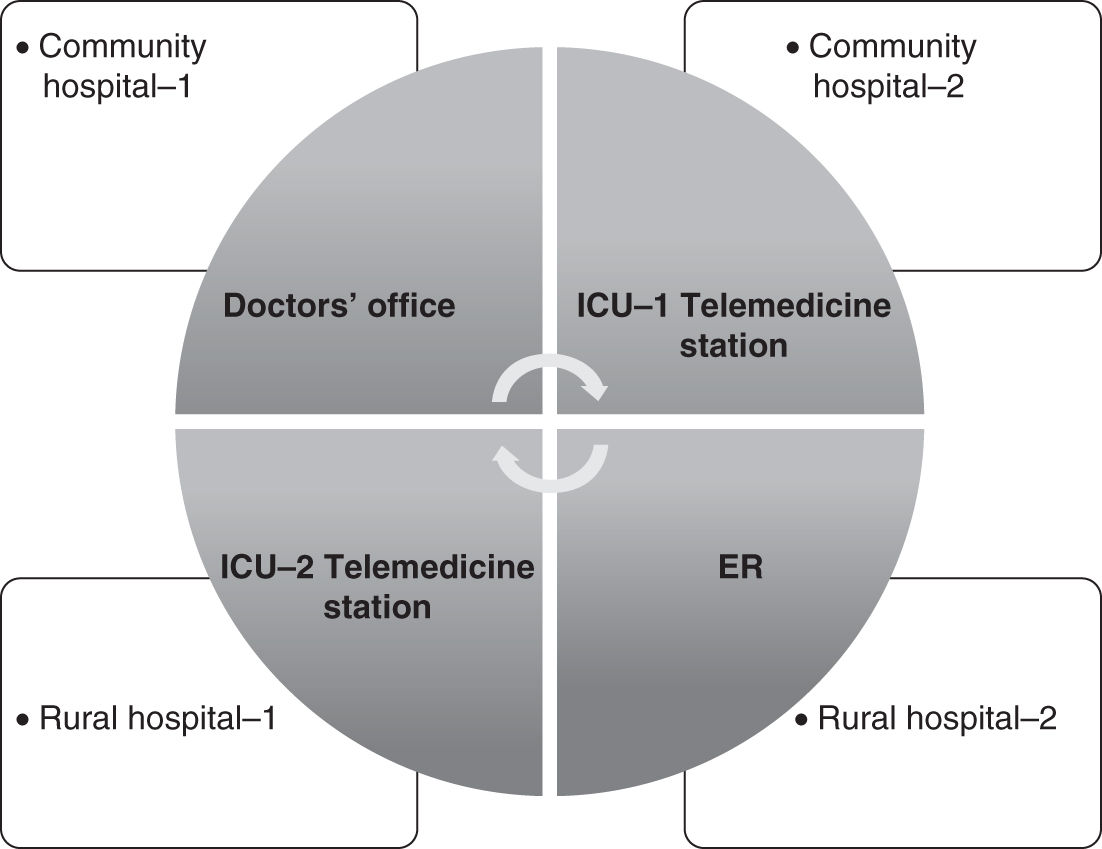
B. Decentralized Model
The decentralized model allows intensivists in different locations to access the tele-ICU via desktop or laptop without relying on a central hub from which to practice (Fig. 40.2). This is associated with significantly reduced startup cost for both the consulting and receiving organization.
C. Hybrid Model
This model combines features of both the centralized and decentralized models. The consulting intensivists are not located in one central location, but may be in multiple facilities, and the model has the ability to provide tele-ICU care to multiple facilities. Similar to the decentralized model, startup and operational costs for the hub are typically lower with this model.
III. ORGANIZATION OF TELE-ICU SERVICE
Successful organization of tele-ICU service requires clinical, business/administrative, and legal collaboration between two or more health care facilities with the common goal of improving access to high-quality critical care. The collaborative domains include personnel, technology, and patient populations.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree