Fig. 14.1
Topographic position of the superior cervical ganglion: (1) glossopharyngeal nerve, (2) superior cervical ganglion, (3) vagus nerve (With permission from Danilo Jankovic)
Fig. 14.2
The superior cervical ganglion has an average size of 26.6 mm (14–43 mm) ×7.2 mm × 3.4 mm. (1) Superior cervical ganglion, (2) sympathetic trunk, (3) vagus nerve with inferior vagal ganglion, (4) masseter muscle, (5) angle of the mandible (With permission from Danilo Jankovic)
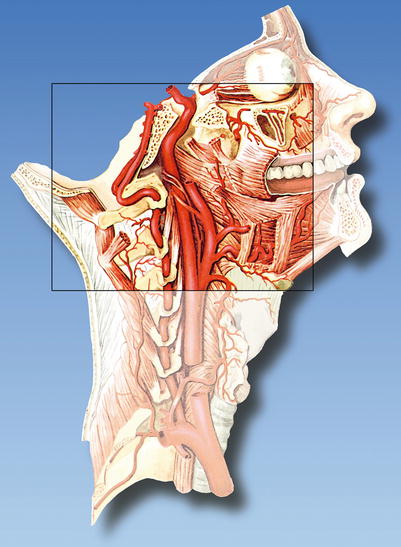
Fig. 14.3
Arteries in the immediate vicinity of the ganglion. Course of the vertebral artery and internal carotid artery (risk of intra-arterial injection) (With permission from Danilo Jankovic)
Fig. 14.4
Immediate vicinity of the superior cervical ganglion: (1) sternocleidomastoid muscle, repositioned dorsally, and the accessory nerve, (2) anastomosis between the C2 vertebral branch and nerve XII, (3) scalenus medius muscle, (4) superior cervical ganglion, (5) hypoglossal nerve, (6) external branch of the superior laryngeal nerve, (7) neurovascular fascicle, repositioned anteriorly (With permission from Danilo Jankovic)
Blocks of the Superior Cervical Ganglion
Indications
The areas of application are partly identical to those for the stellate block, but due to its marked cerebrofacial effects, the superior cervical ganglion block is particularly suitable for the head and facial region—although controlled studies are still lacking here.
Therapeutic [3]
2.
Complex regional pain syndrome (CRPS) in the head region
3.
Perfusion disturbances and vasospastic diseases
4.
Central poststroke syndrome (contralateral block!)
5.
Facial pain
6.
Vertigo (of vertebral origin)
7.
Peripheral facial paralysis
8.
Trigeminal neuralgia in the first and second branches
9.
Postherpetic neuralgias (otic, ophthalmic)
10.
Sudden deafness and tinnitus
11.
Hyperhidrosis in the head region
Specific Contraindications
Grade 2 atrioventricular (AV) block, recent antithrombotic therapy after myocardial infarction or pulmonary embolism, anticoagulation treatment, contralateral paresis of the phrenic nerve, or recurrent laryngeal nerve.
Simultaneous bilateral block.
Procedure
Lateral Extraoral Technique
This block should only be carried out by an experienced anesthetist. The patient should have a full explanation of the procedure before it is carried out.
Preparations
Check that the emergency equipment is complete and in working order. Sterile precautions. Intravenous access, ECG monitoring, pulse oximetry, and ventilation facilities.
Materials
5-mL syringe, 23-G needle (60 mm), intubation kit, emergency drugs, and disinfectant.
Skin Prep
In all blocks.
Patient Positioning
Supine, with the head turned about 30–40° to the opposite side.
Landmarks
Mastoid process, angle of the mandible, and medial margin of the sternocleidomastoid muscle (Fig. 14.5). The angle of the mandible and the mastoid are marked with the index and middle finger. From the anterior margin of the mastoid process, a vertical line is drawn downward; about 1 cm above the angle of the mandible, a horizontal mark is applied. The intersection of these two lines defines the injection point (Fig. 14.6).










