CHAPTER 16

PREHOSPITAL TRAUMA CARE
This chapter is divided into two parts: the first is what the acute care surgeon (ACS) needs to know about the care provided to the patient before the patient arrives in the hospital and the second is a kinematics discussion for understanding the mechanism of injury (MOI). In the best of Emergency Medical Services (EMS) systems, the prehospital providers manage the injured patient for at least the first half of the proverbial “Golden Hour.” It is the responsibility of the ACS to make sure that these providers understand the care of the trauma patient during this critical time period. This care may ultimately determine the outcome for the injured patient. The ACS must teach these principles to the person caring for his or her patient in the field.
Patient care begins when the first person reaches the patient. It does not start when the patient arrives in the hospital. From his experiences in the Spanish American War, Dr. Nicholas Senn, the 49th president of the American Medical Association, surgeon general of the Wisconsin National Guard, and founder of the Association of Military Surgeons stated “The fate of the wounded rests in the hands of one who applies the first dressing.” He was probably quoting the German physician, Johann Nepomuk von Nussbaum from the early 1800s.1
If physicians believe that the care in their particular community in the prehospital period is not good, then they have the duty to teach the prehospital providers the correct methods.
The American College of Surgeons endorsed PreHosptial Life support (PHTLS) training, which is an excellent example of a physician–prehospital provider educational collaboration.2 Involvement with this educational program will go a long way to achieving these educational goals by the ACS.
The philosophy of the continuum of care, which begins in the field and continues to rehab, is an important part of the ACS’s career. The ACS must ensure that the prehospital provider provides this management for trauma patients before they get to the emergency department (ED). Mismanagement in the first 30–90 minutes of care and when the patient is with the prehospital provider is critical to the outcome. It is perhaps more critical than the care provided in the ED. “The die is cast” if the prehospital care is not good.
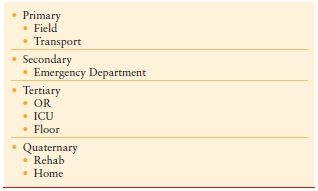
This chapter addresses the important points of the prehospital provider’s training and education. Although there are several providers who care for the patient in many locations, the goals of patient care should be the same, but the steps are different. There is one patient with the same disease in the same condition who requires the same care by different providers using different skills at different locations (Tables 16.1 and 16.2).
TABLE 16.1
CONTINUUM OF CARE
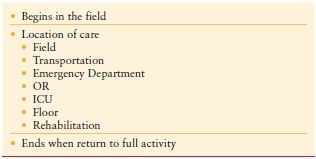
TABLE 16.2
STEPS OF CARE (BASED ON LOCATION)
Each of these providers has different skills, different resources, and different short-term goals. They each provide definitive care in the situation that they encounter the patient (Table 16.3).
TABLE 16.3
DEFINITIVE CARE
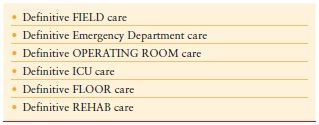
The aim is to provide definitive/appropriate care for the patient as quickly as possible in each individual area and then move to the next area; for example, for the patient who is acidotic in the ED with uncontrolled hemorrhage, the definitive emergency department is for hemorrhage control. This patient needs to be in the Operating room (OR) for hemorrhage control with clamps and ligatures (factor XIV). Keeping the patient in the ED to give crystalloids, factor VII, factor IX, prothrombin clotting complex, or to get additional images such as the CT, is inappropriate. The patient needs to be either in the OR or in the interventional radiology suite with 10 minutes in the ED for the beginning resuscitation. The patient now needs to move on.
The same concept applies to the prehospital environment. For the patient with uncontrolled hemorrhage or potential uncontrolled hemorrhage, definitive field care is rapid movement of the patient to the hospital after control of all visible hemorrhage. The steps are appropriate airway and ventilation management, control of external hemorrhage, packaging for transport, and rapid movement to the trauma center. The patient does not need detailed secondary survey in the field. This can be done during transport if time allows or can be deferred if the transport time is short. Correct definitive field care is getting the patient to a setting where hemorrhage control (damage control surgery) and restoration of energy production are aerobic with metabolism (damage control resuscitation), and can be done as quickly as possible. In the urban areas, this means bypassing a nearby community hospital to go to a trauma center.
It does not mean overloading the patient with crystalloid. Hypotensive resuscitation is the correct management in the field and in the hospital until hemorrhage control can be obtained.
The term “scoop and run” is an incorrect process and should never be the correct method of patient care either in the ED or in the field. This term implies that no care is provided for the patient when transport to the next level of care is imminent. For the prehospital provider, “scoop and run” means placing the patient on the stretcher and racing at high speed to the closest hospital. This method of patient care began to disappear when Dr. J.D. “Deke” Farington wrote his paper entitled “Death in a Ditch,” which was published in the Bulletin of the American College of Surgeons in 19673 (Box 16.1). Fortunately for the trauma patient, such an approach to patient care no longer exists in most of the United States. Unfortunately, this process continues to exist in many third world countries, usually due to a lack of proper trauma education for prehospital providers and lack of funding to provide this education. Just as “scoop and run” is the worst possible approach of addressing the patient’s needs, equally poor is attempting to address all of the patient’s needs in the prehospital arena either in the field or in the back of the ambulance.4 The judgment of the provider based on an understanding of the patient’s needs will define the extent of the field care.
BOX 16.1
DEATH IN THE DITCH3
“Come on fellow, we’ll take you and your wife to the hospital.”
He was pulled from the car, placed on a stretcher, and carried to the ambulance.
Ruth soon was placed on a similar rig. The door was slammed closed and the driver and his helper got into the front seat. The ambulance leaped forward with a screech from the tires and a shriek from the siren.
“Death in the ditch”
JD, ‘Deke’ Farrington MD 1967
The question for the Emergency Medical Technician (EMT) to answer is “what is best for the patient” and “where can this care best be provided.” In the management of any patient, one has to consider the needs of the patient and the ability of the provider to address those needs at a given time and a specific place where the patient currently is located. The provider should assess the patient and provide care according to the situation, the condition of the patient, the abilities of the provider, and the resources available at the scene. This is addressed by understanding principles and preferences. A principle is the specific medical needs of the patient. The preference is how the provider can best address such needs.5 (Table 16.4)
TABLE 16.4
PRINCIPLES AND PREFERENCES
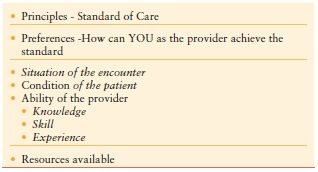
The foundation of patient care is based on certain principles of identification and management of the patient’s condition.
The preferences of how these principles are accomplished are based on the following four separate concepts: (1) the situation the patient and the provider are in at the time of their interaction, (2) the condition of the patient, (2) the skill and knowledge of the provider, and (4) the equipment, resources, and supplies that the provider has to work with at the time.
As an example, the principle is that the airway must be opened. The preference is how it is to be opened. Multiple options are available to the EMT: jaw lift, jaw thrust, nasal airway, oral airway, endotracheal tube, and cricothyrotomy. Scene conditions, situation, and patient condition will dictate which airway option is utilized. An unruly crowd on scene or hazardous weather conditions outside may dictate a rapid, basic-level airway, such as an oral airway or bag valve mask (BVM). This may change in the ambulance with more protection for the patient and the providers. The situation may change more in the ED with different equipment and skills for the provider.
The EMTs in the prehospital arena must be trained with the skills to manage the patient appropriately in a field setting.
The principles are the same, but there are different preferences depending on where the patient is located (Tables 16.3 and 16.4).
Besides principles and preferences, the other concept that requires understanding is definitive care of the patient in the field for the specific patient. Definitive field care will vary depending on the etiology. A patient with cardiac arrest needs definitive care of restoring the rhythm and cardiac output. This can be done in the field at the paramedic level.6 A diabetic patient can be managed definitively in the field using glucose or insulin. A severe trauma patient most likely is suffering from hemorrhage. The hemorrhage cannot be managed in the field definitively. The patient must be transported as quickly as possible to an appropriate facility that can provide such care. The care that might be required is an expedient celiotomy to control the hemorrhage. In the urban setting, the arena for this definitive management is the trauma center that has the availability of trauma surgeons, emergency physicians, operating rooms, and a blood bank. These are the essential components. Just as it is incorrect for the EMS provider to spend more than 10 minutes in the field with a critical hemorrhaging patient, so is it incorrect for this same patient to stay more than 10 minutes in the resuscitation room.
In the rural setting, there is usually no hospital with an immediately available surgeon, operating room, and blood bank. The hemodynamically compromised patient should go to a trauma center in the urban area, but in the rural area, to the closest appropriate facility for stabilization of definitive management. EMS is a critical component of the health care network. Triage is an essential feature of prehospital care. Approximately 5% of the patients that are injured require the facilities of a trauma center. A well-trained provider has the knowledge to understand the patient’s specific condition and understand where the patient can best get the most optimal care.
RURAL TRAUMA ORGANIZATION SYSTEM
Trauma care in the rural communities has been less than that available in the urban area for two major reasons: (1) lack of money to equip staff and train the hospital and EMS personnel and (2) skill deterioration in both groups with lack of severe trauma care experience in the smaller hospitals.
Staff and equipment availability will always be difficult in the rural communities but the training is available to improve competence when the patient does present for care.
The first step in proper management is appropriate field triage and transport of the patient to the appropriate hospital. This must be coupled with an assessment of the strengths of all the hospitals in an area with appropriate bypass or delivery of the patient to the correct facility. Part of the well-developed regional trauma system is an agreement among the hospitals involved to accept the patients when presented and to either treat or stabilize those patients and quickly move them to the appropriate facility.
Such a rural trauma system could be modeled after the Joint Theater Trauma System (JTTS) Military Echelon Casualty management system.7 Patients are taken to facilities dedicated to a specific level of care. When that care has been achieved, the patient is moved on to the next level. An example of this system in action is military personnel seen by medics (Echelon 1) and taken to an Echelon 2 facility where damage control surgery (DCS) is done (hemorrhage control only) and damage control resuscitation is initiated. The patient is sent directly from the OR to an Echelon 3 facility where definitive care is provided (or the second step of DCS). Within 24 hours when the patient is still in the ICU, he or she is moved to an Echelon 4 facility for additional definitive care if needed. Finally within 4–6 days of the injury, the patient is moved to the United States for follow-up care and rehab.
Approximately 10% of civilian injured patients will need assessment in a trauma center. The other 90% should be assessed and treated in the rural community hospital. About 80% of the patients with MOI alone will be discharged within 6 hours of admission into the ED. Of the remaining 20%, almost all will have orthopedic injures that also do not require the expertise of the trauma surgeon and can be better served by providing treatment close to the patient’s family and home. Stated differently, MOI alone is not adequate reason for transporting a patient to a trauma center. These patients should be treated in the appropriate rural or regional hospital. This will also ensure financial support to the local community and community hospitals. The patients, who may require the expertise and resources of the trauma center, can be assessed in the community hospital and then transferred to the trauma center, if necessary. The additional benefit of this type of triage will prevent an overload in the trauma center with patients, who can easily be treated elsewhere (Table 16.5). It is the responsibility of the rural area to understand the resources in the various hospitals and to triage and transport patients to the appropriate hospital.
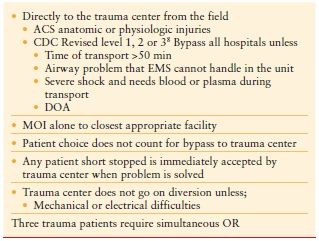
TABLE 16.5
TRAUMA DESIGNATION PROTOCOLS
CONTINUUM OF PATIENT CARE
Patient care should be a continuum from the time the first person sees the patient until the patient is discharged to home. There should be interlinking of the various locations and individuals who provide the care, with prehospital care being an important component of this continuum. The prehospital assessment and care will vary depending on the condition of the patient. A 4 minute ride to the hospital, a 40 minute ride to the hospital, and a 4 hour ride to the hospital are vastly different rides and will require different judgments based on the knowledge2 of the prehospital providers.
Priorities include initial airway management and ensuring adequate ventilation, and if possible, control of hemorrhage. External extremity hemorrhage is controlled with direct pressure and if that fails, then by tourniquet application. Torso hemorrhage control process in the field is only superficial pressure ; therefore, the optimal management is to get the patient to surgical care as quickly as possible. Fracture stabilization is next in priority and intravenous access/resuscitation can often be initiated en route to the hospital.
Patient care is provided based on principles, and these principles must meet the needs of the specific patient involved and the medical conditions present. Situation and available resources impact this decision. The prehospital provider makes a judgment based on this knowledge.2
Although the situation and location of patient care varies, the same basic process and the same attention to quality care exist throughout. There are unique steps, procedures, and techniques that are required to appropriately manage the patient in the prehospital arena—just as there are in the ED, the operating room, or other areas of patient care. This is the continuum of care through the time from injury to discharge. The basic concepts originate from the Advanced Trauma Life Support (ATLS) guidelines: primary assessment, resuscitation, secondary assessment, and definitive care. The degree of detail, the specific procedures, and the training of the providers will vary in each step according to the needs of the patient and the situation in which care is provided. The ACSs understand this concept and how they mesh in each situation to provide the best care for their patients.
The history of prehospital care, as the history of trauma, has chronicled major advances during active times of war. Those steps have been enhanced in times of peace (Tables 16.6 and 16.7).
TABLE 16.6
CHANGES IN MEDICAL CARE BROUGHT ABOUT BY WARS
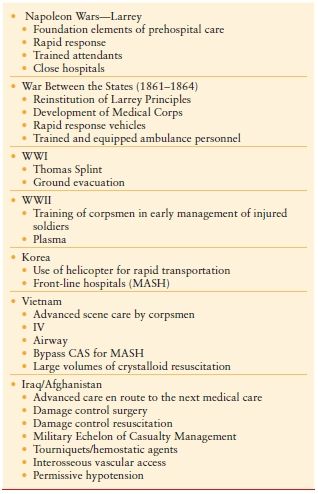
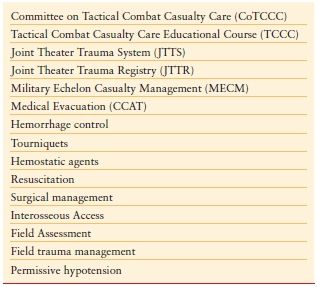
TABLE 16.7
CHANGES INITIATED FROM THE CURRENT CONFLICTS
The origin of prehospital care is credited to Baron Larrey, Napoleon’s surgeon. He first recognized that leaving a patient for 3–30 days in the field with his or her injury was not in the best interest of the patient nor of their General (Napoleon). Therefore, he devised a system of rapid response in the field, with the rapid transport of the patient to a close medical facility to provide care. Care was provided both in the field and en route to the hospital with well-trained individuals. This remains the fundamental hallmark of prehospital care in the 21st Century: (1) rapid response to the field, (2) well-trained personnel who provide care in the field and en route to the hospital, (3) rapid transport of the patient to an appropriate hospital, (4) hospital near the site of injury, and (5) well-trained personnel in the hospital to provide care. With increasing emphasis on prioritization of management and with the advancement of patient transport systems, prehospital care continued to evolve.
These principles were lost in the early years of the War Between the States (1861–1865). In the first battle of Manassas (Battle of Bull Run), July 1861, injured patients were left in the field for up to 7 days before being transported. In addition, the transferring personnel were poorly trained. Medicinal alcohol was used liberally, and overall patient care was generally poor. This defect was addressed and changed by Jonathan Letterman (1824–1872) when he was made the commandant of the medical teams and they moved from the Quartermaster Corps to the Medical Corps.
PREHOSPTIAL TIME
R Adams Cowley, MD, the founder of Maryland Institute of EMS (MIEMS), developed the slogan “the golden hour” to emphasize the importance of getting a patient to definitive hospital care as soon as possible. While the 60 minute timeline should not be interpreted literally, emphasis should be placed on expeditious and effective care in order to adequately address severe injuries and critical illness. The need to move quickly for patients needing torso, extremity, and neck hemorrhage control is critical.9
Prior to the mid 1980s, when Dr. Crowley demonstrated the importance of a trauma center for providing timely management, the concept of limited time in the field was not well understood based on the “Golden Hour.” The prehospital scene care and transport can be as little as 10–12 minutes in a well-run metropolitan EMS system or 25–30 minutes in a well-run suburban system. In the rural setting, the transport times can be hours after the initial traumatic event occurred. Prehospital time can be even longer in a wilderness setting. During this period of time, significant pathophysiologic changes can occur, resulting in deterioration of the patient’s physiologic state, which can negatively affect survival, or create complications or long-term disability.
Similarly, delay should not occur in the ED for unneeded assessment or in opening the abdomen in the ED. Directing this process is the responsibility of the ACS.
PREHOSPITAL EDUCATION AND SURGICAL CONTROL OF PREHOSPITAL CARE
Once in the surgeon’s hands and in the hospital, the outcome for the patient can be substantially affected by the care, or lack thereof, that occurred in the field. For this reason, the complete trauma care of the patient, both before and after arrival in the hospital, must be under the control of the surgeon. This is from the instant the injury occurs until the patient is discharged from the hospital. This is the important continuum of trauma care. Fragmentation of patient care by a committee of providers is not in the best interest of the patient. Each may have a different perspective. Someone must be in charge.
For the surgeon to be involved in the prehospital care does not mean that the surgeon must be physically present in the field physically on every run. However, the surgeon must be present philosophically in the field by being involved in the education of the prehospital provider, understanding what happens in the field, engaging in quality assurance, and having confidence in the EMTs’ ability and skill. The EMTs must appreciate this presence. This is achieved by (1) spending time with them, providing education both in the ED and in their classroom experiences, and (2) riding with them on the street and understanding the conditions under which they carry out their responsibilities in the field, working with the EMS committee of the medical society or the trauma center. This does not negate the responsibility of the emergency medicine physicians’ involvement in EMS.
PREHOSPITAL CARE SYSTEM
Prehospital care is divided into two distinct components: (1) the EMS system and (2) the physiology, pathophysiology, and management of the trauma patient in the field. The same components are used in the hospital but in a different environment, that is, prevention of anaerobic metabolism by assuring oxygen of the RBC in the lung with delivery of those RBCs to the tissue. A major part of this process is hemorrhage control in the hospital environment. After all, “trauma is a surgical disease from beginning to end.”10 The ACS must understand and appreciate both components of care in the field, just as s/he must understand the hospital system and the physiology, pathophysiology and management of patient care in order to function effectively.
From the beginning of a surgeon’s education in medical school, the day-to-day system in which the ACS functions in the hospital becomes apparent in the form of surgical schedules, patient admission, QA processes, peer review, morbidity and mortality conferences, and management of patient records including discharge summaries and operative notes. Such system information and much of the clinical/scientific information in the realm of prehospital care are often not taught to the surgeon in training. In order to ensure optimal patient care, it is imperative for the ACS to understand all of the key elements of the prehospital network and be involved in their teaching.
EMS SYSTEM AND PERSONNEL
An EMS system is to EMS and the EMT as the hospital is to medicine and the individual physician. It is the EMS system that provides a “home” for the EMTs, supervision of their function, quality assurance of their practice, delineation of their privileges, definition of their scope of practice, and financial support of the organization to provide patient care. But it does even more. The EMS system allows the hospital to get the critical and debilitated patients into the ED. Greater than 40% of the hospital admissions come through the ED. Patients would somehow get to the ED without EMS but not with the appropriate care en route and not to the correct hospital that is prepared to handle their specific problem.
The key to running an effective EMS system is strong physician oversight and quality control with attention to the details of patient outcome, skill utilization, skill success, proper judgment, and of the run report analysis.
Initially, there was only the EMT-A (Ambulance) certification available. In the early 1970s, the U. S. Department of Transportation codified the EMT into three levels, which with some small exceptions and modifications are the national standard of the 21st century. These are the EMT-Basic, EMT-Intermediate, and EMT-Paramedic. These have been abbreviated into EMT-B, EMT-I, and EMT-P. Many discussants further abbreviate this to use the term “EMT” meaning the basic EMT and “paramedic” meaning the EMT paramedic. Further references will utilize the terms EMT-B, EMT-I, and EMT-P and for the individual levels, EMT as a generic term indicating all three levels.
EMT-B
The EMT-Basic has completed a minimum of 110 contact hours of training following the objectives as outlined in the U. S. Department of Transportation’s (DOT) National Standard Curriculum and tested either by the National Registry for EMTs or the individual state license exams or both. Depending on the state, reregistration is required every 2–4 years to maintain that license. Each state has varying criteria for this reregistration. EMS runs are approximately 1/3 trauma, 1/3 medical, and 1/3 cardiac. The EMT-B training program is divided essentially along these lines with emphasis on life- or limb-threatening injuries such as cardiac arrest, airway problems, childbirth, hemorrhage control, fracture immobilization, and seizures.
Additional training includes defensive driving, utilization of communication systems, ethics, legal issues, and run report writing.
EMT-I
The EMT-Intermediate has been trained to the level of an EMT-B, frequently has 1 or 2 years experience on the streets functioning as an EMT-B and takes approximately 200 hours of additional education, which includes IV fluid administration, advanced airway management, automatic defibrillation and in some states, limited use of drugs.
EMT-P
The EMT-Paramedic is trained with an increased emphasis on the utilization of cardiac drugs, medication for pain control, airway assistance (RSI in some systems), and seizure management. The drugs on the EMS unit usually consist of advanced blood pressure cardiac medications, glucose and insulin for the management of diabetic patients, pain and seizure medication, which would include morphine, a sedative, rapid sequence intubation (RSI) drugs and, perhaps, fentanyl or ketamine. The training program to reach the EMT-P level varies from state to state, but it is traditionally in the range of 1,000 to 1,200 hours in addition to the EMT-I. This includes not only didactic lectures, but time in various patient care areas, in the hospital such as the operating room, ER, ICU, and a supervised field internship. At the completion of the training program, the student takes the state examination, the examination of the National Registry of EMTs, or both to obtain a license to function at the ALS level. Reregistration to maintain this license is required every 2–4 years depending on the state. The reregistration depends on sustainment education in trauma, cardiac, and medical conditions, as well as skill demonstration and practice such as IVs and endotracheal intubation and a backup airway.
A growing number of EMS services throughout the United States are utilizing RSI with drug control, for airway management. Research results of the use of RSI in the field have been mixed, with respect to effectiveness; it is believed to be less effective with shorter transport time.
EMT-PARAMEDICS WITH A PHYSICIAN
There is a fourth level of care that is used by some systems in the United States and Canada, which is with a physician as part of the medical response system. Much literature in North America has indicated that the use of a physician prolongs the EMS run, delays transports, and has a negative impact on outcome. However, in Central and South America, many services rely on physicians to provide field care. In Europe, many services use only nurses for prehospital care.
Many systems in the United States in the early 21st century have begun to have a physician riding the streets with a supervisor. This physician provides radio medical control, medical supervision, and education on the scene, and adds to the quality assurance process. This type of arrangement has been thought to be effective especially in the urban areas for immediate and retrospective medical control (see below) as medical director (this is usually an emergency medicine resident), and responds to scenes on an ad lib basis, and some systems, usually not in the United States, have a full-time physician assigned to the ambulance.
COMMUNICATIONS
Prehospital communication systems are divided into two major categories:
- Dispatch/administrative communications with the EMS system control
- Medical communications with the hospital or physician
In the United States, most of the EMS dispatch is done by an emergency citizen access arrangement, using the 9-1-1 patient access phone number. The communication arrangement may be separated into police, fire, and EMS, but some communities combine fire and EMS. Other communities combine law enforcement and EMS. There are some communities, especially in rural areas, in which all three components are combined into one unit. Other countries have a similar communication system, but a different phone number.
Regardless of the system used, the function is
Notification : to receive a phone call from a patient, a family member, or a bystander and identify the type of call
Dispatch : to send the appropriate vehicle and personnel and provide assistance by the telephone to the caller while the ambulance is en route
Scene : to survey the scene (see scene survey below), identify additional resources or backup that are required, notify the dispatch of such needs, begin to address patient care, and get the patient ready for transport to the hospital
Transport : to ensure movement of the patient to the correct hospital for care of the condition(s) found
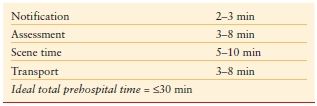
Urban EMS response times are highlighted in Table 16.8. It is clear from the table that even the best of systems use half of the “Golden Hour” in the field. The assessment and transport times will change based on the density of the population and the difficulty of the terrain.
TABLE 16.8
URBAN EMS RESPONSE TIMES
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








