MAXILLOFACIAL INJURIES
Maxillofacial trauma encompasses injuries to the soft tissue and skeletal and visceral organs of the face. Fractures occur when forces that exceed their tolerance are applied. Although facial injuries are often not life threatening, their significance cannot be understated. Facial injuries may interfere with nasal, auditory, mandibular, or ocular function. The potential for postinjury disfigurement and disability can be associated with long-term physical and psychological sequela.
The management of maxillofacial trauma can be traced back to ancient times. The Edwin Smith papyrus (1550 bc), the oldest known medical papyrus, contains detailed descriptions of the surgical management of facial skeletal and soft tissue injuries. Hippocrates described the timeless methods of closed reduction of mandible dislocations, wiring of teeth and jaw immobilization of mandible fractures, and closed reduction of nasal fractures.1 The management of these injuries in isolation is straightforward. However, facial trauma is often associated with other injuries that may be life threatening, requiring immediate attention. So when does one begin to address the maxillofacial injuries in the multiply injured patient? It is the purpose of this chapter to review the mechanisms of injury, clinical presentation, diagnostic modalities, and the initial management of the wide spectrum of maxillofacial injuries. The priority-based approach to the polytrauma patent is reviewed as pertains to the patient with facial trauma.
INITIAL ASSESSMENT
Airway
The initial assessment of the acutely injured patient, irrespective of the injury complex, remains unchanged. The Adult Trauma Life Support® (ATLS) program provides a standard prioritized approach to the initial evaluation and management of the trauma patient.2 The first priority is that of the airway. In the patient with maxillofacial trauma, the airway may be compromised by lack of support from the tongue, unstable skeletal support, or obstruction of the airway due to foreign bodies or bloody secretions. An organized approach should be utilized in managing the airway to optimize patient outcome (Algorithm. 23.1). The oral cavity should be first cleared of secretions, supplemental oxygen given, an oral airway placed, and the jaw thrust maneuver applied to assist with the opening of the posterior pharynx. The cervical spine is immobilized assuming the presence of a cervical spine injury, which occurs in approximately 1%–5% of patients with facial fractures.–36 Immobilization is maintained until the cervical spine is both radiographically and clinically evaluated to exclude an acute fracture. Patients with immediate or persistent airway problems require placement of a definitive airway defined as a cuffed tube within the trachea. The definitive airway of choice is a translaryngeal endotracheal tube.2 Care should be taken to avoid iatrogenic injury to the maxillary central incisors during intubation. Nasally placed tubes (nasotracheal, nasogastric) should be avoided in the setting of facial trauma as central bony fractures may be present allowing passage into the cranial vault. When the difficult airway is encountered, a surgical airway, cricothyroidotomy, is the definitive airway of choice.2
Breathing
Patients with facial trauma may present with oxygenation and ventilatory difficulties. Although airway compromise is often assumed, a respiratory etiology must also be sought. Penetrating injuries should be assessed for trajectory as missiles may be present in the neck or thoracic cavity. The presence of subcutaneous emphysema should prompt further investigation to rule out injury to the upper airway, aerodigestive tract, or tracheobronchial tree. A supine portable CXR serves as the initial adjunct study for further assessment of the hypoxic patient. Clinical findings consistent with a tension pneumothorax (absent breath sound, tracheal deviation, hypoxemia, and hemodynamic lability) require immediate needle decompression with subsequent thoracostomy tube placement. Hypoxemia in the stable patient with evidence of a pneumothorax or hemothorax is managed with placement of a thoracostomy tube.
Circulation
Acute hemorrhage continues to be the second most common cause of death in the trauma population.7 Fatal traumatic hemorrhage accounts for a large portion of early deaths, with the majority of exsanguinations occurring within the first 48 hours.8,9 Following stabilization of the airway and breathing, circulation with hemorrhage control is the next priority in assessing acutely injured patients. The vascular supply to the face is vast and in the setting of diffuse soft tissue injury may serve as a source of considerable blood loss. The best way to control hemorrhage in the acute setting is with well-placed direct pressure. This concept is central even in the setting of oral and maxillofacial injuries. Following placement of intravenous access, the site of hemorrhage is assessed to determine the method of pressure to be applied. Nasal fractures are often associated with bleeding. Direct pressure on the nares often controls epistaxis from an anterior source. Substantial bleeding from a posterior source may require nasal packing, balloon compression, or both to obtain hemostasis (Fig. 23.1). Patients with complex facial fractures due to either blunt or penetrating trauma have multiple sites of bleeding that may prove difficult to control. Encompassing the concept of direct pressure, facial packing and compressive dressings techniques have been described to achieve hemostasis.10 Packing of the oropharynx following airway control is in essence similar to the four-quadrant packing of the abdomen in an attempt to obtain hemorrhage control.11,12,13–14 When bleeding is refractory to compressive methods, angioembolization is employed for definitive control (Algorithm. 23.2).
FIGURE 23.1. Nasal packing: packing to control bleeding from the posterior nose, (A) catheter inserted and packing attached; (B) packing drawn into position as catheter is removed; (C) strip tied over bolster to hold packing in place with anterior pack installed “accordion pleat” style; (D) alternative method, using balloon catheter instead of gauze packing.
DEFICIT AND ENVIRONMENT
The initial neurological evaluation includes the assessment of the pupillary response and the computation of the Glasgow Coma Score (GCS).15 Abnormal pupillary response and/or a low GCS score indicate the presence of a traumatic brain injury (TBI) requiring computed tomography (CT) scan of the brain for further assessment. Certain facial fractures, are often associated with an intracranial injury. When a TBI is diagnosed, prompt neurosurgical consult should ensue. Exposure of the patient by removing all clothing allows for unobstructed evaluation of associated injuries. During the initial evaluation, the environment should be controlled. Warm fluids and external warming methods are used to prevent hypothermia as it may contribute to the development of coagulopathy.
SECONDARY SURVEY
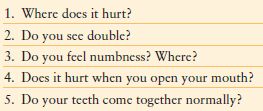
Only upon stabilization of the patient and completion of the primary survey can one proceed with the secondary assessment. Potential life-threatening injuries are assessed and managed during this stage of the evaluation. A history and complete “head-to-toe” physical examination should be performed. The information provided by the prehospital personnel about the mechanism of injury and surrounding events guides the astute provider in the assessment for possible associated injuries. Patients with facial injuries due to a blunt mechanism (MVC, falls, assaults), often have associated injuries. Once the less life-threatening injuries have been excluded, then evaluation of the maxillofacial region can begin. The approach to the maxillofacial examination should include evaluation of the soft tissues, skeleton, dentition, and nerves. In the awake patient, focused questioning can provide clues to the presence of underlying skeletal fractures (Table 23.1). The physical examination must be organized and methodical to minimize missed injuries. Inspection and palpation serves as the basis for the maxillofacial examination. Drainage from the nose, rhinorrhea, or the external auditory canal, otorrhea, should be carefully inspected for the presence of cerebral spinal fluid (CSF). Clinically the diagnosis is made upon observing the “double ring” sign (small central blood ring surrounded by a larger peripheral clear ring) that is produced when the fluid is placed on a paper towel. If there is a high index of suspicion of CSF leak, the fluid should be sent to the laboratory for a β2-transferrin (which is present only in CSF) or a quantitative glucose analysis. The presence of β2-transferrin or a glucose level >30 mg/100 mL is consistent with the presence of CSF. The oral cavity is then inspected for lacerations, soft tissue injuries, abnormal dentition, and bleeding. The tongue is often a source of non–life-threatening bleeding, but may require suture placement for hemostasis. Lacerations of the soft tissue and gingival, bony irregularities, tenderness, and numbness must be adequately evaluated to diagnose an underlying skeletal fracture. The presence of numbness is due to the involvement of the sensory branch of the trigeminal nerve and, in mandible fractures, the inferior alveolar nerve. Avulsed dentition may serve as a possible source of airway obstruction when aspirated; therefore, a CXR should be obtained. Once the examination is completed, appropriate imaging studies, (CT scan, panorex) are performed. Complete CT scans of the face with coronal views aid in the diagnosis of facial fractures and planning of operative intervention if required.
TABLE 23.1
SCREENING QUESTIONS FOR EVALUATION OF CRANIOFACIAL TRAUMA
Soft Tissue Injuries
Soft tissue injuries to the maxillofacial region present a considerable challenge in management as there can be untoward cosmetic and functional deficits if not addressed in an appropriate manner. Complex facial lacerations can cause substantial bleeding as the face is very well vascularized with the terminal branches of the external carotid artery as its main supply. This vast vascular supply also allows for lacerated tissues with small pedicles to survive if managed carefully.16,17 Therefore the initial approach to soft tissue injuries includes copious irrigation, appropriate antibiotics, and limited debridement. Primary closure of facial wounds, for up to 24 hours postinjury, is employed when adequate tissue is present. Good cosmesis is generally achieved due to an abundant blood supply and repeatable patterns of soft tissue injury.18 Proper suturing technique is essential to minimize potential disfigurement. Layered closure with approximation of deep layers using braided absorbable sutures to eliminate potential dead space and fine monofilament sutures for skin closure that is tension-free minimizes scarring. Skin sutures should be removed in 3–5 days as this also minimizes scarring. The patient should be advised to apply sunscreen to the affected area during the first year of healing to prevent discoloration of the scar.
Lip laceration repair requires careful attention. Wound management follows the general principle of soft tissue management of the face. Thorough irrigation should be used prior to closure and antibiotics that cover gram-negative anaerobes should be considered. The wound is inspected for the presence of foreign body and tooth fragments from associated dentoalveolar injuries. Wound depth evaluation is crucial as unrecognized penetration through the oral mucosa may allow salivary contamination. The oral mucosa should be approximated to prevent salivary contamination. The muscle fibers of the orbicularis oris run in a transverse manner and tend to pull the wound edges apart, giving the appearance of an avulsive tissue loss, which is rarely the case. Alignment of the vermilion border is central in the closure technique to obtain a good cosmetic result.19 When it is properly performed, cosmetic results are maximized, and scarring is minimal.
Avulsive maxillofacial injuries are typically the result of an impact with high kinetic energy. Close-range gunshot wounds (GSW) and high-speed MVC impact can lead to large full-thickness soft tissue loss. These wounds are frequently associated with other life-threatening conditions such as hypovolemic shock and airway embarrassment. Soft tissue injury management is best performed with serial dressing changes of saline-soaked gauze in the multi-injured patient. Once stabilized, extensive reconstructive procedures are often required to address large soft tissue loss. Injured soft tissue surrounding the area of initial trauma progresses to an evolving pattern of tissue loss and necrosis requiring serial debridements. Once all devitalized tissue is removed, a variety of tissue transfer techniques (local, regional, free flap) can be employed to obtain skeletal coverage.–2024 Early reconstruction provides better cosmetic and functional results as compared to delayed secondary repair.20,25
Dentoalveolar Injuries
Traumatic facial injuries frequently involve the dentition and dentoalveolar structures. Common causes of dentoalveolar trauma include MVC, falls, sports injuries, and assaults. Involvement of the maxillary incisors due to their prominent position in the mouth is common. Injury patterns range from various fractures of the teeth to fractures involving the supporting bony alveolus (Fig. 23.2). Lacerations of the lips and gingiva are frequently associated with dentoalveolar trauma and can complicate their management. Prompt diagnosis and treatment of these injuries are important when one considers the esthetic implications of tooth loss, especially since these injuries tend to occur in children and young adults.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree