Postoperative Cognitive Dysfunction
Catherine Price
J. S. Gravenstein
CASE SUMMARY
Within hours or days of a major surgery, some patients will experience disturbances of cognition, and even delirium. Clinical experience and numerous studies suggest that these changes will resolve spontaneously as the patient’s pain subsides; as active drugs in the central nervous system (CNS) undergo biotransformation and elimination; and as hormone levels return to baseline. Soon after discharge from the hospital, physicians usually lose contact with patients; occasionally, weeks or months after a surgery, we encounter a patient who claims to have been plagued by subtle changes in brain function. It is not unusual for patients to blame anesthesia because of its profound CNS effects.
The following observed stories exemplify what the clinician may hear from a patient with possible postoperative cognitive dysfunction (POCD):
An attending anesthesiologist in his thirties underwent an exploratory thoracotomy and resection of a small pulmonary nodule. He had an uneventful anesthetic procedure and smooth recovery from anesthesia. He returned to work soon after but complained for several months that he could not solve crossword puzzles because he found it difficult to concentrate.
A 54-year-old woman, an avid and apparently competent bridge player, had to undergo repeated surgeries for lysis of intra-abdominal adhesions. After each of her surgeries, she was soon able to attend to her daily chores as a housewife but for approximately 6 months, she found it difficult to play bridge because she could not remember the cards that had been played.
An 82-year-old woman was seen for the removal of a small tumor near her chin. She was accompanied by two of her children. When the option of general anesthesia was mentioned, the children strongly objected, saying that their mother had had a surgery 8 weeks ago and she had not been the same since. She was very forgetful and sometimes confused.
An executive secretary reported, approximately 3 months after a surgery under general anesthesia, difficulty in functioning at her accustomed level of intensity and perspicacity. She asked whether she could expect full recovery.
An insurance company executive had a peripheral vascular surgery. Several months postoperatively, he found it impossible to carry out required statistical calculations.
An 80-year-old woman had knee replacement surgery and a normal recovery until approximately 3 weeks postoperatively when she awoke one morning wondering why her leg was sore and painful. She had lost all memory of her surgery event and rehabilitation. She continues to have no recollection of any these events.
Concerns about cognitive or neurologic change after surgery or anesthesia have continued to grow since a publication by Bedford in 1955 claiming that anesthesia induced mental changes in the elderly.1 Despite an increase in publications related to the topic and improved understanding about possible risk factors associated with postoperative cognitive changes, we still do not know the specifics of how anesthesia influences cognitive change, what brain systems may be involved, or how best to treat symptoms when they do occur. In this chapter we aim to provide fodder for thought (and hopefully some helpful tools) for clinicians who encounter postoperative cognitive dysfunction, as well as for researchers studying the phenomenon.
What Is Postoperative Cognitive Dysfunction?
In research articles, the term, postoperative cognitive dysfunction, or POCD, denotes postoperative memory and/or thinking problems that have been corroborated by neuropsychological testing. Although not yet a recognized diagnostic code in the International Classification of Diseases (ICD), clinicians are beginning to use the term POCD as a general description of postoperative patients who complain of memory and thinking problems. Typically,
these complaints include difficulty staying focused on a task, difficulty completing more than one task at the same time, problems finding words, and difficulty recalling information recently heard or read. Postoperative cognitive dysfunction should not be confused with delirium, which, in contrast to POCD, involves fluctuating orientation and confusion.
these complaints include difficulty staying focused on a task, difficulty completing more than one task at the same time, problems finding words, and difficulty recalling information recently heard or read. Postoperative cognitive dysfunction should not be confused with delirium, which, in contrast to POCD, involves fluctuating orientation and confusion.
When POCD needs to be listed as a diagnosis, the Diagnostic and Statistical Manual‘s (DSM-IV)2 definition of “Cognitive Disorder Not Otherwise Specified” (ICD Code Number: 296.5) may be appropriate. This requires the clinician to document cognitive changes that cannot be attributed to another etiology such as delirium, dementia, or cognitive dysfunction due to a specific cause.
Are Certain Patients at Risk for Postoperative Cognitive Dysfunction?
As demonstrated by the examples in the preceding text, an individual of almost any age or education level can experience POCD. The symptoms also vary. Clinicians, therefore, need to remain attentive to all patients and listen carefully to their postoperative complaints.
A number of studies demonstrate that, at least during the first 3 postoperative months, elderly patients have higher rates of POCD than young and middle-aged adults. In large studies of patients undergoing noncardiac surgery, the prevalence of POCD among adults 60 years of age and older was between 20% and 30% at 1 week and 10% to 15% at 3 months.3,4 We know little about POCD occurring beyond 1 year. One study reports that only 1% of elderly adults experience the persistent effects of cognitive decline after surgery,5 which may indicate that POCD is reversible even among the elderly.
Apart from age, another strong risk factor for POCD appears to be years of formal education. A low educational level has been shown to predict cognitive decline, whereas high educational levels seem to protect against cognitive decline following surgical procedures involving cardiopulmonary bypass.6 One proposed rationale for this relationship involves the concept of cerebral cognitive reserve: Extensive education or high occupational attainment has been associated with the ability to recruit neuronal structures to replace damaged processing pathways.7 Other explanations for the relationship between POCD and educational level include test-taking skills, enhanced social support, and excellent postoperative medical care. Of course, there are always exceptions to these findings, as shown from the case descriptions at the beginning of this chapter, and therefore predicting who is at great risk for POCD will be at best tentative.
Surprisingly, as compared to age and level of education, comorbidity has been largely ignored in research. Intuitively, we would expect increased susceptibility to POCD in patients suffering debilitating conditions known to affect postoperative morbidity, such as high blood pressure, congestive heart failure, repeat coronary artery bypass grafting, anemia, carotid arteriosclerosis, diabetes, left ventricular ejection fraction lower than 45%, chronic pulmonary disease, and unstable angina—all conditions that have been shown to affect postoperative morbidity.
Importantly, both clinicians and researchers have a tendency to ignore the role of mental comorbidities (e.g., depression, presurgical cognitive impairment) as possible risk factors for postoperative complications. The importance of mental health influences is alluded to by a retrospective study by Berstein and Offenbartl.8 These authors report that out of 975 general surgery patients, 57 had postoperative fatal and nonfatal complications; most of those who had a fatal complication had symptoms of dementia before surgery (25 of 32 who died had dementia). These findings suggest that a patient with a presurgical mental disorder, specifically a dementia, may be particularly sensitive to surgical events.
What Type of Assessments Can Be Useful for Identifying Postoperative Cognitive Dysfunction?
As discussed in the preceding text, despite evidence pointing to population risk factors, predicting who is at risk for POCD remains problematic. Therefore, direct observations and documentation of patients’ cognitive abilities before surgery and again after surgery may be helpful.
▪ BRIEF COGNITIVE MEASURES
In addition to the customary preoperative and postoperative clinical evaluations, a clinician can consider using a few basic tests to assess general cognition. Two examples include the Mini Mental State Examination (MMSE)9 and the Clock Drawing test.10 These measures are simple to administer and provide basic information about patients’ orientation, memory, visual construction (drawing), and planning abilities.
Mini Mental State Examination
The MMSE is a frequently used measure of general cognitive status that examines orientation, learning and memory, attention, language functions, and visual construction. The MMSE requires approximately 10 minutes to administer (guidelines available in the study9). A score between 28 and 30 indicates intact cognitive functions. A comparatively low postoperative score relative to a preoperative score (e.g., presurgical score = 25, 1 day postoperative score = 19) would be cause for concern and may require enhanced postanesthesia follow-up and neurologic and/or neuropsychological consultation.
Clock Drawing Test
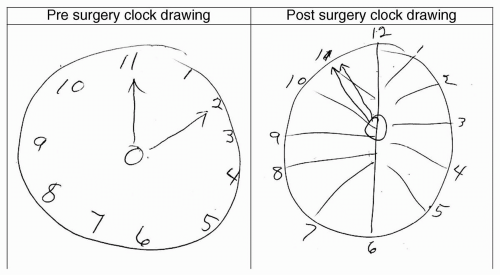
The Clock Drawing Test10 is a simple measure that assesses attention, planning, and organization. Only pencil and paper are needed for the test. The patient is asked: “Please draw the face of a clock, put in all of the numbers, and set the hands to ten after 11.” Although seemingly simple, this task assesses a number of cognitive functions. The patient has to remember what a clock looks like, plan the clock face, appropriately align the numbers, and simultaneously remember the instructions while drawing the hands to the appropriate time. The time, itself, “ten after eleven,” requires the patient to inhibit or ignore the competing visual of a “10” while drawing the hand to the appropriate number “2.” Scoring involves tallying the errors produced by the patient (guidelines available in the study10). This simple test provides a clear indication of cognitive dysfunction simply by comparing a drawing done before surgery to one done after surgery (see Fig. 27.1).
Additionally, tests that assess learning and memory may be helpful if the patient presents with memory problems. Two of these measures include word list-learning measures and story memory tests.
List-Learning Tests
List-learning tests assess how well an individual learns and retains a list of words. There are a number of list-learning tests available and they differ with regard to difficulty (i.e., number of words available) and age appropriateness. For example, the Hopkins Verbal Learning Test-Revised11 assesses an individual’s ability to learn a list of 12 words over three different learning trials. This test has multiple forms, which are valuable for repeat testing. Clinicians are urged to use only those test forms, however, that are equivalent in difficulty. See provided reference for more information.11
Paragraph or Story Memory Tests
Paragraph or story memory tests are another option for quickly assessing learning and memory. These tests involve reading a paragraph or story to an individual and then requiring him/her to repeat the story to you both immediately and then after a set time delay. A well-known story memory measure is the Logical Memory subtest from the WMS-Revised or WMS-Third Edition.12
Finally, the service of a neuropsychologist may be the optimal choice, not only for the administration of the tests but also for the comprehensive assessment and written documentation of the findings.
▪ BRAIN IMAGING
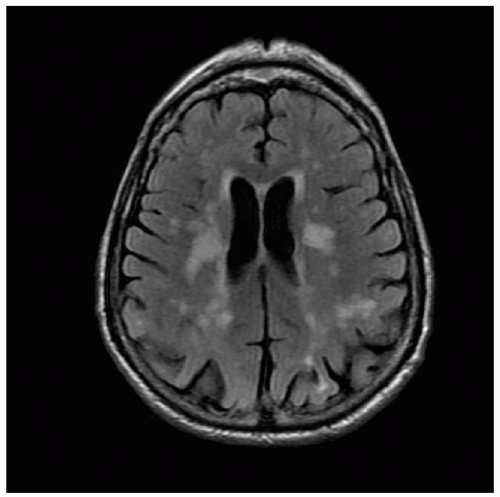
Brain magnetic resonance imaging (MRI) done either before or just after surgery can be quite valuable. A brain MRI before the surgery serves two purposes: (i) It provides a baseline for comparison with postsurgical MRI; and (ii) It may also identify neuroanatomic risk factors for surgical stroke. For example, patients with lesions in the white matter (see Fig. 27.2) may have a greater risk of acute cognitive decline post surgery.13 Pre-existing white matter lesions and lacunae also increase the risk for postoperative stroke.14,15,16 White matter changes have often been considered benign, as they occur with increasing age, but they are seen in abundance in vascular dementias17 and may play a role in the development of POCD.13
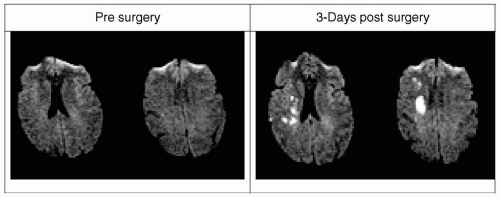
For some individuals, a brain MRI before surgery may be helpful for assessing the risk versus benefit of a given elective surgical procedure. If a preoperative MRI is not available, a postoperative brain MRI can assist in ruling out a stroke, as seen in Figure 27.3. A diffusion-weighted MRI within the first 72 hours of surgery is particularly useful for identifying new frank and “silent” strokes.
Are Certain Brain Regions Associated with Postoperative Cognitive Dysfunction?
To date, no research has directly examined which brain regions are most often associated with the primary symptoms of POCD (e.g., mild to moderate attention disturbance, word finding problems, difficulty learning new information). We can speculate, however, which anatomic zones may be most susceptible. We base this speculation not only on a general understanding of neuropsychology but also on recent research suggesting that there may be subtypes of POCD.18 Some patients experience primary disturbances in attention, whereas others experience only learning and memory difficulties.
What Anatomic Systems Can Underlie Postoperative Attention and Concentration Disturbances?
Attention is an extremely complex function that is regulated by cortical gray matter regions, subcortical nuclei, and white matter tracts. The most vulnerable regions to surgical factors, however, are likely the subcortical gray matter nuclei (e.g., caudate, putamen, nucleus accumbens, globus pallidus, substantia nigra, subthalamic nucleus, thalamus) and white matter tracts (e.g., the internal and external capsules) because they are highly susceptible to numerous neurotransmitter and small vessel changes. The importance of the basal ganglia, in particular, on one’s ability to attend and inhibit distracting information has been demonstrated mostly by elegant animal studies19 and also by studies on neurodegenerative illnesses such as Parkinson disease.20 Additionally, the thalamus is a primary subcortical structure necessary for both attention and memory. It is, unfortunately, also the most common site for ischemic changes and dysfunction, particularly among older adults.
The subcortical nuclei are in very close proximity to the intricate vessels of the Circle of Willis and smaller intracranial arterioles, such as the lenticulostriate arteries (see Fig. 27.4), which nourish important subcortical nuclei (e.g., caudate) and associated white matter tracts. Intracranial arterioles such as the lenticulostriate arteries are particularly vulnerable to hemodynamic changes.21 These changes may result in reduced arteriole wall integrity thereby leading to reduced nourishment or possible protein leakage into the white matter or gray nuclei. This would lead to the development of white matter changes (Fig. 27.2) and lacunae within the thalamus and basal ganglia.21 Such damage is hypothesized to result in a disconnection to the frontal lobe thereby leading to attention disturbances. This disconnection can be at least partially explained by neurotransmitter disruption, for the interplay between subcortical nuclei and white matter is largely regulated by inhibitory (GABAergic [γ-aminobutyric acid]) and excitatory (glutaminergic) neurotransmitters.19
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree