Introduction
Cardiac pacing devices can be either temporary or permanent. Temporary techniques include percussion (fist) pacing, transcutaneous pacing and transvenous pacing. Permanent pacemakers (PPM) are used for the treatment of severe bradycardia, and for left ventricular pacing as part of cardiac resynchronisation therapy (CRT) for the treatment of chronic heart failure; implantable cardioverter-defibrillators (ICDs) are used for the treatment of life-threatening ventricular arrhythmias.
Understanding the methods for providing temporary pacing is invaluable in resuscitation care. With the increased prevalence of pacemakers and ICDs, an awareness of the capabilities and complications associated with devices is essential.
Indications for pacing and ICDs
An abbreviated summary of indications adapted from the ACC/AHA/HRS 2008 and NICE 2007 guidelines are shown in Box 14.1.
Methods of pacing
Non-invasive pacing
Both percussion pacing and transcutaneous pacing can be used to treat profound bradycardia causing severe haemodynamic instability or cardiac arrest. Non-invasive pacing is an emergency measure used until either resolution of the bradycardia or definitive invasive pacing has been established.
Indications for emergency pacing
NB: If a permanent pacemaker is indicated, avoid temporary pacing and arrange for urgent implantation of a permanent system
Indications for permanent pacing (PPM)
Percussion pacing
When bradycardia is so profound that it causes clinical cardiac arrest, percussion pacing may produce an adequate cardiac output and negate the need for CPR. It enables either recovery of a spontaneous cardiac rhythm or maintenance of vital organ perfusion before implementation of transcutaneous or transvenous pacing. Percussion pacing is more likely to be successful when ventricular standstill is accompanied by continuing P wave activity. Percussion pacing is not as reliable as electrical pacing; if it fails, start CPR immediately. See Box 14.2 for an outline of how to perform percussion pacing.
- With the side of a closed fist raised about 10 cm above the chest, deliver repeated firm blows to the precordium lateral to the lower left sternal edge
- If these do not generate QRS complexes, try using slightly harder blows and move the point of contact around the precordium until a site is found that produces repeated ventricular stimulation
Transcutaneous pacing
Compared with transvenous pacing, non-invasive transcutaneous pacing is simpler and quicker to implement (Box 14.3).
- Attach ECG monitoring electrodes and leads if necessary—these are needed with some transcutaneous pacing devices
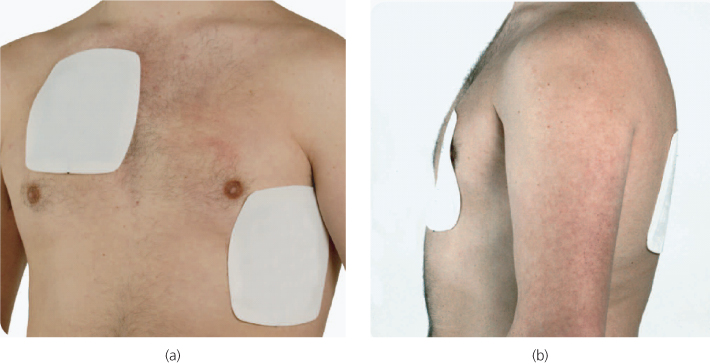
- Position the electrode pads in either the conventional right pectoral-apical (preferred) or the anterior-posterior (A-P) positions (Figure 14.1)
- If using a pacing device that is not capable of defibrillation, use A-P positions for the pacing electrodes so that defibrillator pads can still be used in the right pectoral and apical positions if cardiac arrest occurs
- Most transcutaneous pacing devices offer pacing in demand mode; the pacemaker will be inhibited if it detects a spontaneous QRS complex. Beware of movement artefact, which may also inhibit the pacemaker and may necessitate switching to fixed-rate pacing mode
- Select an appropriate pacing rate. This will usually be in the range of 60–90 min−1 for adults, but in some circumstances (for example complete AV block with an idioventricular rhythm at 50 min−1) a slower pacing rate of 40 or even 30 min−1 may be appropriate to deliver pacing only during sudden ventricular standstill or more extreme bradycardia
- If the pacing device has an adjustable energy output set this at its lowest value and turn on the pacemaker. Gradually increase the output while observing the patient and the ECG. As the current is increased the muscles of the chest wall will contract with each impulse and a pacing spike will appear on the ECG. Increase the current until each pacing spike is followed immediately by a QRS complex, which indicates electrical capture (Figure 14.2) (typically with a current of 50–100 mA using a device with adjustable output)
- Check that the apparent QRS complex is followed by a T wave. Occasionally, artefact generated by the pacing current travelling through the chest may be mistaken for a QRS complex; this artefact will not be followed by a T wave
- If the highest current setting is reached and electrical capture has not occurred, try changing the electrode positions. Continued failure to achieve electrical capture may indicate non-viable myocardium
- Having achieved electrical capture with the pacemaker, check for a pulse, which confirms ‘mechanical capture’ of the ventricle. Absence of a pulse in the presence of good electrical capture constitutes pulseless electrical activity (PEA).
Figure 14.1 Transcutaneous pacing using electrode pads in the (a) conventional right pectoral-apical or (b) anterior-posterior (A-P) positions. Photograph reproduced with kind permission by Michael Scott and the Resuscitation Council (UK).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








