The importance of high-quality cardiopulmonary resuscitation
The performance of high-quality, uninterrupted chest compressions is an important determinant of outcome from cardiac arrest (Box 19.1). Observational studies have shown that chest compression depth influences shock success, return of spontaneous circulation rates (ROSC) and survival. Higher chest compression rates (up to 125 min−1) are linked to improved ROSC. In animal models, failing to release pressure between compressions reduces coronary blood flow, which may have a negative effect on outcomes. Similarly, hyperventilation raises mean intrathoracic pressure, which reduces coronary perfusion and worsens outcome. CPR fraction (the proportion of resuscitation time spent performing chest compressions) is also a strong predictor of survival. Despite the prominence of CPR technique on outcome, observational studies provide consistent evidence of poor-quality CPR in clinical practice.
Cardiopulmonary resuscitation feedback and prompt devices
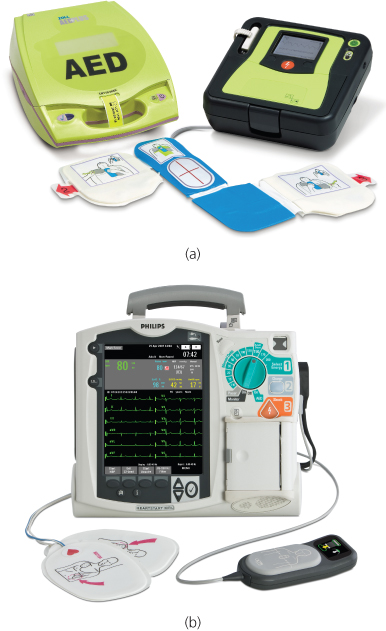
Cardiopulmonary resuscitation feedback and prompt devices aim to improve the performance of resuscitation skills by CPR providers (Table 19.1). Cardiopulmonary resuscitation feedback devices give information on the quality of CPR as it is performed, either through a visual display or audio instructions. Cardiopulmonary resuscitation prompt devices provide guidance to perform specific actions (e.g. sequence of CPR, audible beep for compression rate). The devices range in complexity from a simple metronome to an advanced defibrillator providing audio and visual feedback and prompts (Figure 19.1).
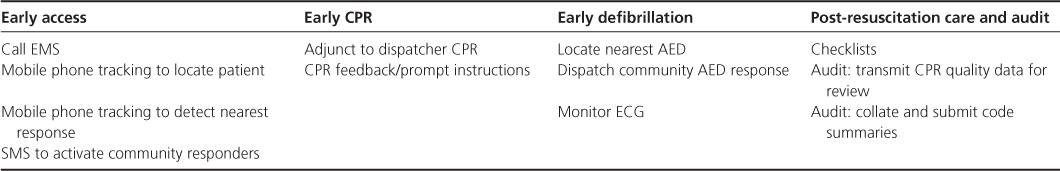
Table 19.1 Summary of different CPR feedback/prompt technology and their applications. Filled circle, currently available technology; empty circle, technology in early development phase.
- Compression depth 5–6 cm
- Compression rate 100–120 min−1
- Minimise interruptions in compressions
- Ensure full chest re-coil between compressions
- Avoid hyperventilation
The more sophisticated devices assess CPR performance by measuring transthoracic impedance through defibrillation electrodes or through the use of an accelerometer (a small device placed on the sternum) or a combination of both. Measurement of transthoracic impedance enables chest compression rate, compression fraction and ventilation rate to be calculated. The addition of an accelerometer enables compression depth and completeness of release between compressions to be quantified (Figure 19.2).
Figure 19.2 Sophisticated CPR feedback/prompt devices integrated with defibrillators. Reproduced by permission of ZOLL Medical Corporation. Reproduced by permission of Philips Electronics UK Limited.
A systematic review of the evidence for CPR feedback and prompt devices conducted as part of the International Liaison Committee for Resuscitation (ILCOR) review of resuscitation science in 2010, concluded that there is good evidence supporting the use of CPR feedback/prompt devices during CPR training to improve CPR skill acquisition and retention. Their use in clinical practice as part of an overall strategy may also be beneficial. The review highlights that accelerometers underestimate chest compression depth when CPR is performed on a soft surface such as a mattress as they do not differentiate between chest compression and mattress compression.
Since the publication of this review, a large cluster randomised study in the US examined the use of CPR feedback technology in out of hospital cardiac arrest. Although CPR feedback technology improved CPR quality, there was no difference in ROSC rates or survival to discharge. However, baseline CPR performance and survival was higher than that observed in many communities, thus leaving limited opportunity for CPR process improvement to affect outcome. The time taken for rhythm analysis with an automated external defibrillator may have negated the effect of CPR quality improvement. Finally, the study investigated a single CPR feedback system. Whether other systems or the addition of post-event debriefing of emergency medical services (EMS) staff would influence outcomes remains to be determined. Further trials of CPR feedback technology during in- and out-of-hospital cardiac arrest are in progress.
Mobile phones
The now almost universal carriage of mobile smart phones positions them as a potentially useful adjunct for CPR practice. Applications that support initial training, feedback/prompts during resuscitation and audit of outcomes have been developed (Table 19.2 and Figure 19.3).
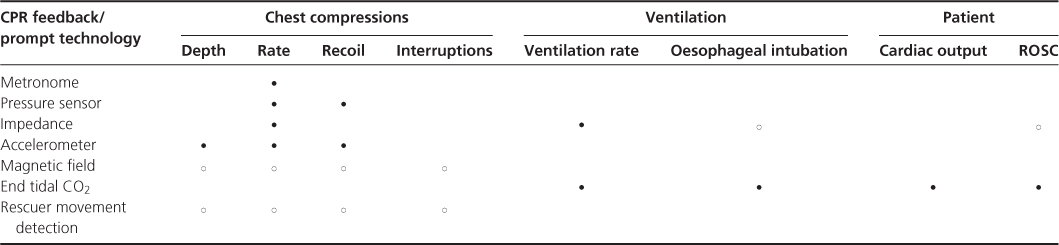
Table 19.2 Mobile phone technology can support each link of the chain of survival.