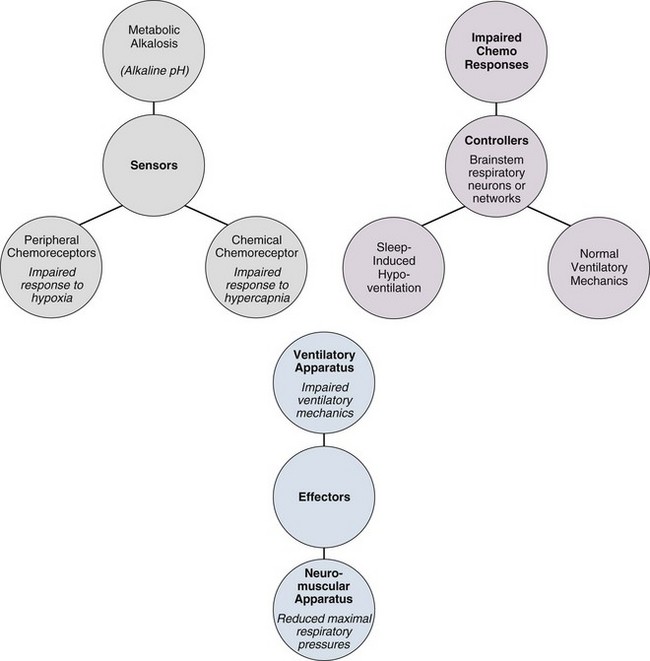
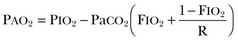
41 MECHANISMS UNDERLYING CHRONIC ALVEOLAR HYPOVENTILATION CLINICAL RECOGNITION AND MANIFESTATIONS Acute Respiratory Failure Caused by Neuromuscular Disease Noninvasive Positive Pressure Ventilation When to Use Noninvasive Ventilation in Nonpulmonary Causes of Respiratory Failure CHRONIC VENTILATORY-ASSIST DEVICES An estimated 20% of respiratory failure is a result of nonpulmonary causes such as disorders that affect the upper airway, chest wall, muscles of respiration, and nervous system. Hypoventilation is the primary pathophysiologic etiology of all of these disorders.1 Hypoventilation is defined as alveolar ventilation that is inappropriately low for metabolic demands. Alveolar (A) and arterial (a) PaCO2 are elevated. Arterial pressure is decreased. Alveolar hypoventilation exists when arterial PCO2 increases above the normal range of 37 to 43 mm Hg.2–7 Hypoventilation is associated with arterial hypoxemia (when breathing room air oxygen) and a raised arterial PCO2. The rise in PaCO2 as a result of hypoventilation can be calculated using the alveolar ventilation equation.8 In a single-compartment lung model, alveolar PCO2 and PO2 are inversely related according to the alveolar air equation. An increase in alveolar PCO2 is associated with an obligatory fall in alveolar PO2. During hypercapnia, the alveolar minus arterial P(A – a)O2 difference predicted by this model (while breathing room air) is “normal.” Regarding the combination of hypercapnia and a normal P(A – a)O2 difference as a requirement to diagnose nonpulmonary disorders associated with hypoventilation is common clinical practice. However, these disorders are also commonly complicated by microatelectasis, retention of secretions, and bronchopneumonia, which cause abnormal ventilation/perfusion inequality and increase the P(A – a)O2 difference. Conversely, the P(A – a)O2 difference has been shown to be an unreliable index of abnormal gas exchange in the presence of substantial hypercapnia. For these reasons, a normal P(A – a)O2 difference is not helpful in differentiating pulmonary from nonpulmonary causes of respiratory failure. The alveolar partial pressure of oxygen is calculated with the formula: where FIO2 is the inspired oxygen fraction (0.21 in all calculations) in the dry gas, PIO2 is the inspired PO2, and R is the respiratory exchange ratio (assumed to be 0.8). In other words, the flow of CO2 molecules across the alveolar membrane per minute is divided by the flow of O2 molecules across the membrane per minute. PaCO2 is the ideal alveolar carbon dioxide tension. This is true only if a steady state of alveolar ventilation and carbon dioxide production rate exists. In clinical practice it is common to consider the combination of hypercapnia and a normal P(A – a)O2 difference as a requirement to diagnose nonpulmonary disorders associated with hypoventilation.9 However, hypoventilation-induced atelectasis causing abnormal gas exchange will result in an increase in P(A – a)O2 difference.10 In the presence of substantial hypercapnia, an abnormal alveolar-to-arterial oxygen difference may not rule out a nonpulmonary cause of hypoventilation. Defects in the metabolic control system result in hypoventilation when abnormalities in blood gases and cerebral acid-base status are not sensed or if sensed do not produce an appropriate change in motor output of the medullary respiratory neurons. Patients with such defects fail to breathe normally in response to metabolic respiratory stimuli, but because the behavioral control system, respiratory motor pathways, and ventilatory apparatus are intact, they are capable of voluntarily driving respiration. As a result, patients with defects in the metabolic control system typically demonstrate normal ventilatory mechanics, but they have impaired responses to metabolic respiratory stimuli and often hypoventilate severely during sleep, when ventilation is critically dependent on the metabolic control system.1,3,11–17 As a result of chronic hypoventilation, these patients have a primary respiratory acidosis leading to a secondary increase in extracellular bicarbonate ion concentration.18,19 In contrast, patients with a primary metabolic alkalosis may develop secondary hypoventilation as a compensatory response. This type of hypoventilation represents not a defect in respiratory control but rather an appropriate response of the metabolic control system to a disturbance in acid-base status. It is said that patients with metabolic alkalosis “shouldn’t” breathe, in contrast to those with control defects, who “won’t” breathe, and those with mechanical defects, who “can’t” breathe. However, the degree of hypoventilation that develops in response to metabolic alkalosis depends on several factors, including associated electrolyte disturbances and the sensitivity of the peripheral chemoreceptors to the accompanying hypoxemia.19,20 Therefore, patients with weak hypoxic responsiveness tend to hypoventilate more than do patients with brisk hypoxic responsiveness. Chronic hypoventilation resulting from defects in effector elements of the respiratory system represents disturbances of ventilatory motor and mechanical function, and these defects do not in themselves mean that the metabolic control system is defective. Because the same effector elements also serve the behavioral control system, these patients are usually unable to breathe normally even when consciously attempting to do so. Hence, such defects are characterized either by reductions in the maximum inspiratory pressures that can be generated voluntarily or by impairment of lung volumes and flow rates.21 In the presence of such neural or mechanical defects, coexisting disturbances in respiratory control are often difficult to identify because the neuromuscular or mechanical defect may preclude normal responses to chemical respiratory stimuli even when the control system is intact.1 Plum and Leigh22,23 described nonrespiratory causes of respiratory failure. Causes of hypoventilation include depression of the respiratory center by drugs such as morphine derivatives and barbiturates; diseases of the brainstem such as encephalitis; abnormalities of the spinal cord conducting pathways such as high cervical dislocation; anterior horn cell diseases including poliomyelitis that affect the phoenix nerves or supplying intercostal muscles; diseases of nerves to respiratory muscles (e.g., Guillain-Barré syndrome); diseases of the myoneural junction such as myasthenia gravis; diseases of the respiratory muscles themselves such as progressive muscular dystrophy; thoracic cage abnormalities (e.g., crushed chest); upper airway obstruction (e.g., thymoma); hypoventilation associated with extreme obesity (Pickwickian syndrome); and other miscellaneous causes such as metabolic alkalosis and idiopathic states.2 In all these conditions the lungs are normal. Neuromuscular diseases are accompanied by variable degrees of involvement of the muscles of inspiration and expiration. The clinical manifestations reflect the compromise of both muscle groups.24 Disorders of respiratory control and those of peripheral neuromuscular disease are shown in Tables 41.1 and 41.2, respectively. Table 41.1 Disorders of Ventilatory Control* *Studies cited in this table may be found in the complete list of references for this chapter provided online. Table 41.2 Disorders of the Peripheral Neuromuscular System*
Nonpulmonary Causes of Respiratory Failure
Introduction
Hypoventilation
Pathophysiology (Fig. 41.1)
Mechanisms Underlying Chronic Alveolar Hypoventilation (see Fig. 41.1)
Etiologic Classification
Respiratory Failure from Neuromuscular Disease
Disorder
Associations
Mechanism
Metabolic alkalosis54
Maintenance of metabolic alkalosis for any length of time means that renal homeostatic mechanisms for HCO3– excretion have been disrupted.
Impaired autonomic control of ventilation. Voluntary control remains intact.
Ondine’s curse55,56 (congenital or acquired central alveolar hypoventilation)
Usually caused by congenital hypoventilation syndrome but can be from surgical incisions into the second cervical segment to relieve intractable pain.57 Can also be seen in medullary infarction in an intermittent form.58–60
Impaired automatic control of ventilation. Voluntary ventilation remains intact. Classically, the patient “forgets to breathe” when asleep. Patient maintains relatively normal blood gas while awake.3,61
Carotid body resection62
Introduced in Japan in the 1940s as a treatment for asthma.63,64 Also seen after bilateral endarterectomy for carotid vascular disease.
Depressed hypoxic ventilatory drive during exercise.
Generally eucapnic at rest.
Destruction of peripheral chemoreceptors.65,66
Cheyne-Stokes respiration67,68
Commonly associated with cardiac disease; can also be seen in neurologic disease sedation, sleep, altitude acclimatization.69
Delay between changes in ventilation and detection of the resulting arterial PCO2 by the central chemoreceptors maintains a cyclic pattern of respiration.
Myxedema
In critically ill patients, laboratory differentiation between severe hypothyroidism and the euthyroid-sick syndromes is difficult and may require measurement of free hormone levels.
Respiratory muscle weakness. Depression of ventilatory drive.70–72
Starvation
Nutritional intervention can return muscle ventilatory function to normal levels. Furthermore, it seems likely that the ventilatory drive can be influenced by dietary intake of amino acids and glucose.
Decreased ventilatory drive, decreased respiratory muscle function, alterations of lung parenchyma and depressed lung defense mechanisms.
Drug effects
Opiates, barbiturates, benzodiazepines
Should be used judiciously in patients with preexisting hypoventilation.
Medroxyprogesterone†
Increases ventilatory drive in normal males leading to about 5 mm fall in PaCO2.
Used in obesity hypoventilation syndrome.73–75
Theophylline†
Increases hypoxic ventilatory response and prevents the fall in hypoxic ventilatory response.
Acetazolamide†
Efficacy and side effects of long-term use are unknown. Small, crossover study reduced central apnea in patients with congestive heart failure.76
Site of Disease
Disease
Type of Respiratory Failure
Spinal Cord
Space-occupying lesions
Syringomyelia
Chronic respiratory failure
Multiple sclerosis77
Chronic respiratory failure
Mass
Chronic respiratory failure
Anterior horn cell lesions
Poliomyelitis5,16,78
Chronic respiratory failure
Amyotrophic lateral sclerosis
Chronic respiratory failure
Inhibiting neuronal blockade
Tetanus
Acute respiratory failure
Any level
Traumatic injury
Acute respiratory failure
Motor Nerves
Peripheral Neuropathy
Phrenic nerve injury54
Acute/chronic respiratory failure
Beriberi79
Chronic respiratory failure
Guillain-Barré80
Chronic respiratory failure
Critical illness polyneuropathy81,82
Chronic respiratory failure
Lyme disease83
Chronic respiratory failure
Diphtheria84
Acute respiratory failure
Neuromuscular Junction
Tick paralysis85
Organophosphate poisoning
Acute respiratory failure
Botulism86
Acute respiratory failure
Eaton-Lambert syndrome
Acute respiratory failure
Myasthenia gravis5,31
Acute/chronic respiratory failure
Muscle Involvement
Dystrophies
Muscular dystrophy5,31,87–89
Chronic respiratory failure
Myotonic dystrophy90,91
Chronic respiratory failure
Myopathy
Polymyositis, dermatomyositis, and other collagen vascular diseases92
Chronic respiratory failure
Malnutrition93
Chronic respiratory failure
Thyroid, adrenal, pituitary glands
Chronic respiratory failure
Metabolic acid-base, electrolyte4,18–20
Acute respiratory failure
Disorders of the Chest Wall
Obesity hypoventilation4,94–96
Acute/chronic respiratory failure
Asphyxiating thoracic dystrophy97
Acute/chronic respiratory failure
Fibrothorax98
Acute/chronic respiratory failure
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access