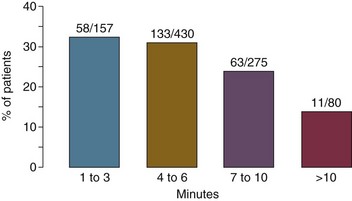
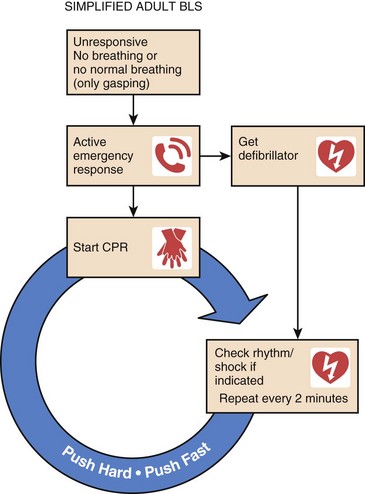
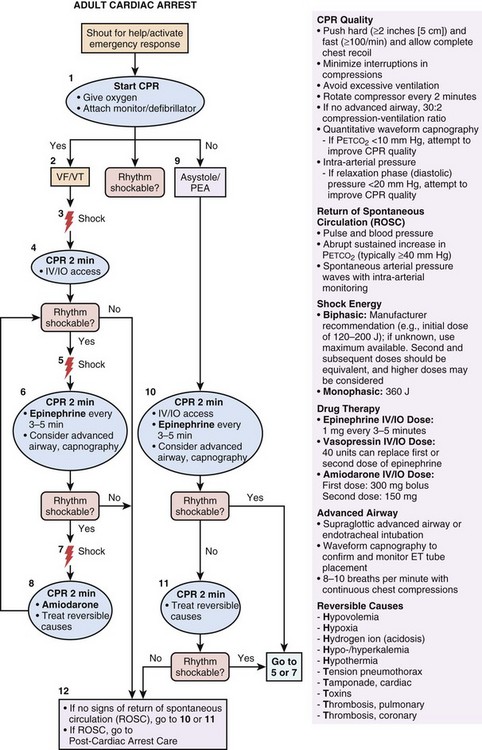
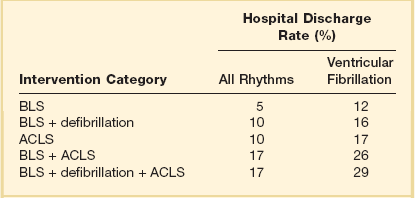
1 Sudden cardiac arrest is defined as the cessation of effective cardiac mechanical activity as confirmed by the absence of signs of circulation. Sudden cardiac arrest is the most common fatal manifestation of cardiovascular disease and a leading cause of death worldwide. In North America alone, approximately 350,000 persons annually undergo resuscitation for sudden cardiac arrest. Approximately 25% of sudden cardiac arrest events are due to pulseless ventricular arrhythmias (i.e., ventricular fibrillation [VF] or pulseless ventricular tachycardia [VT]), whereas the rest can be attributed to other cardiac rhythms (i.e., asystole or pulseless electrical activity [PEA]).1 Patients who suffer cardiac arrest due to VF or VT have a much higher chance of surviving the event compared with patients who present with PEA/asystole.2 Patients with ventricular arrhythmias have a better prognosis because (1) ventricular arrhythmias are potentially treatable with defibrillation (i.e., “shockable” initial rhythm) to restore circulation, whereas the other initial rhythms are not, and (2) ventricular arrhythmias are typically a manifestation of a cardiac cause of cardiac arrest (e.g., acute myocardial infarction), whereas the other initial rhythms are more likely to be related to a noncardiac cause and perhaps an underlying condition that is less treatable. The success with cardiopulmonary resuscitation (CPR) for VF as compared to other rhythms across varying levels of rescuer intervention is displayed in Table 1.1. The basic principles of resuscitation are an integral part of training for many health care providers (HCPs). Because timely interventions for cardiac arrest victims have the potential to be truly lifesaving, it is especially important for critical care practitioners to have a sound understanding of the evaluation and management of cardiac arrest. Table 1.1 Estimates of Success of Cardiopulmonary Resuscitation Based on 31 Published Reports ACLS, advanced cardiac life support; BLS, basic life support. Adapted from Cummins RO, Ornato JP, Thies WH, et al: Improving survival from sudden cardiac arrest: The “chain of survival” concept. Circulation 1991;83:1832-1847. A number of critical actions (chain of survival) must occur in response to a cardiac arrest event. The chain of survival paradigm (Fig. 1.1) for the treatment of cardiac arrest has five separate and distinct elements: (1) immediate recognition that cardiac arrest has occurred and activation of the emergency response system; (2) application of effective CPR; (3) early defibrillation (if applicable); (4) advanced cardiac life support; and (5) initiation of postresuscitation care (e.g., therapeutic hypothermia).3 For CPR to be effective in restoring spontaneous circulation, it must be applied immediately at the time of cardiac arrest. Therefore, immediate recognition that a cardiac arrest has occurred and activation of the emergency response system is essential. Patients become unresponsive at the time of cardiac arrest. Agonal gasps may be observed in the early moments after a cardiac arrest event, although normal breathing ceases. Pulse checks (i.e., palpation of femoral or carotid arteries for detection of a pulse) are often unreliable, even when performed by experienced HCPs.4 Because delays in initiating CPR are associated with worse outcome, and prolonged attempts to detect a pulse may result in a delay in initiating CPR, prolonged pulse checks are to be avoided. CPR should be started immediately if the patient is unresponsive and either has agonal gasps or is not breathing.3 In CPR, chest compressions are used to circulate blood to the heart and brain until a pulse can be restored. The mechanism by which chest compressions generate cardiac output is through an increase in intrathoracic pressure plus direct compression of the heart. With the patient lying in the supine position, the rescuer applies compressions to the patient’s sternum. The heel of one hand is placed over the lower half of the sternum and the heel of the other hand on top in an overlapping and parallel fashion. The recommended compression depth in adults is 2 inches. The recommended rate of compression is 100 or more per minute. “Push hard, push fast” is now the American Heart Association (AHA) mantra for CPR instruction. This underscores the importance of vigorous chest compressions in achieving return of spontaneous circulation (ROSC).5 In addition, incomplete recoil of the chest impairs the cardiac output that is generated, and thus the chest wall should be allowed to recoil completely between compressions. Owing to rescuer fatigue, the quality of chest compressions predictably decreases as the time providing chest compressions increases, and the persons providing chest compressions (even experienced HCPs) may not perceive fatigue or a decrease in the quality of their compressions.6 Therefore, it is recommended that rescuers performing chest compressions rotate every 2 minutes. The quality of CPR is a critical determinant of surviving a cardiac arrest event.7 Minimization of interruptions in chest compressions is imperative. Interruptions in chest compressions during CPR have been quite common historically, and the “hands off” time has been shown to take up a substantial amount of the total resuscitation time.7 Potential reasons for “hands off” time include pulse checks, rhythm analysis, switching compressors, procedures (e.g., airway placement), and pauses before defibrillation (“preshock pause”). All of these potential reasons for interruptions must be minimized. Pauses related to rotating compressors or pulse checks should take no longer than a few seconds.5 Eliminating (or minimizing) preshock pauses has been associated with higher likelihood of ROSC and improved clinical outcome.8 The next critically important action in the resuscitation of patients with cardiac arrest due to pulseless ventricular arrhythmias (i.e., VF or pulseless VT) is rapid defibrillation. Delays in defibrillation are clearly deleterious, with a sharp decrease in survival as the time to defibrillation increases.9 With the advent of automatic external defibrillators (AEDs) and their dissemination into public places, both elements of effective CPR (both effective chest compressions and rapid defibrillation) can be performed by lay rescuers in the field for patients with out-of-hospital cardiac arrest. Figure 1.2 shows the importance of rapid defibrillation, with decreasing success of resuscitation with increasing time to defibrillation. The most recent AHA recommendations regarding ventilation during CPR depends on who the rescuer is (i.e., trained HCPs versus lay person).5 For trained HCPs, the recommended ventilation strategy is a cycle of 30 chest compressions to two breaths until an endotracheal tube is placed, and then continuous chest compressions with one breath every 6 to 8 seconds after the endotracheal tube is placed. Excessive ventilations can be deleterious from a hemodynamic perspective due to increased intrathoracic pressure and reduction in the cardiac output generated by CPR and thus should be avoided during resuscitation. Excessive ventilation could also potentially result in alkalemia. For lay persons who are attempting CPR in the field for a victim of out-of-hospital cardiac arrest, rescue breathing is no longer recommended. Rather, the recommended strategy is compression-only (or “hands-only”) CPR.5 The rationale is that compression-only CPR can increase the number of effective chest compressions that are delivered to the patient (i.e., minimizes interruptions for rescue breaths), and does not require mouth-to-mouth contact. Mouth-to-mouth contact is one of the perceived barriers to CPR in the field. By removing this element, the hope is that an increase in attempts at bystander CPR will result. Hands-only CPR has been found to be not inferior to conventional CPR including rescue breaths for victims of out-of-hospital cardiac arrest,10–12 and thus hands-only CPR has become the preferred technique to teach lay rescuers. Figure 1.3 displays the AHA algorithm for adult basic life support. There are several additional elements of resuscitation that are intended specifically for trained HCPs (e.g., advanced cardiac life support [ACLS]), and these elements include pharmacologic therapy. Figure 1.4 displays the AHA algorithm for ACLS.13 The primary goal of pharmacologic interventions is to assist the achievement and maintenance of spontaneous circulation. The mainstay of pharmacologic interventions is vasopressor drugs. Epinephrine (1 mg) is administered by intravenous (IV) or intraosseous (IO) route every 3 to 5 minutes during CPR until ROSC is achieved.13
Cardiac Arrest and Cardiopulmonary Resuscitation
Epidemiology and General Principles
Cardiopulmonary Resuscitation and Advanced Cardiac Life Support
Chest Compressions
Defibrillation
Rescue Breathing
Advanced Cardiac Life Support
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Cardiac Arrest and Cardiopulmonary Resuscitation