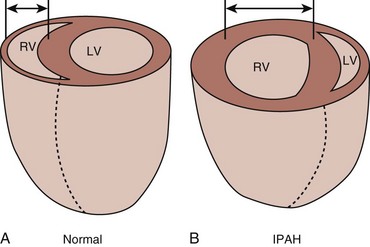
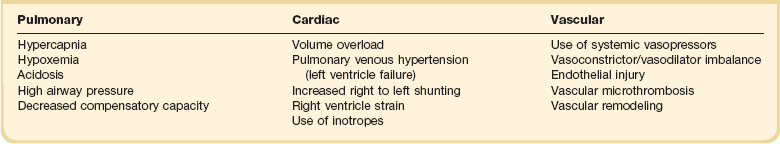
45 PATHOPHYSIOLOGY OF PULMONARY HYPERTENSION AND RIGHT VENTRICULAR FAILURE CLINICAL CLASSIFICATION OF PULMONARY HYPERTENSION INTEGRATED APPROACH TO THE DIAGNOSIS OF PULMONARY HYPERTENSION MANAGEMENT OF ARTERIAL PULMONARY HYPERTENSION AND RIGHT VENTRICULAR FAILURE IN THE INTENSIVE CARE UNIT Pulmonary hypertension (PH) is a complex and heterogeneous pulmonary vascular disorder that leads to elevated pulmonary vascular resistance (PVR) and right ventricular failure. During recent years, multiple advances in the therapy and management of PH have been made; however, this disorder continues to cause significant morbidity and mortality. PH is defined by a resting mean pulmonary arterial pressure (mPAP) greater than 25 mm Hg, associated with PVR greater than 240 dynes ⋅ second ⋅ cm−5 (or >3 Wood units) measured by right-sided heart catheterization. It is very important for the intensivist to distinguish those patients who have chronic PH secondary to any of the five groups included in the clinical classification described in Box 45.1 from other conditions that are usually faced in the intensive care unit (ICU) that can cause an acute elevation in the PVR. The acute elevation of pulmonary artery (PA) pressure observed in critically ill patients can develop on top of preexisting chronic PH (acute on chronic). It can be transient without consequences, or it can be prolonged and progress to severe acute PH, leading to life-threatening complications that include refractory systemic arterial hypotension, severe hypoxemia, right ventricular dysfunction and failure, and ultimately cardiogenic or obstructive shock and death. The most common acute elevation of PA pressures in the ICU is seen in the setting of left-sided heart disease (elevated pulmonary venous pressure) or in patients with preexisting pulmonary vascular disease. It is also well recognized after cardiothoracic surgery, during sepsis, after pulmonary embolism (PE), and in acute respiratory distress syndrome (ARDS). Unfortunately, in most cases acute PH remains underdiagnosed and its treatment begins only after serious complications have been developed. In order to understand the pathophysiology of PH and before reviewing its current clinical classification, it is important to identify where the vascular insult originates. Conditions that raise the postcapillary pressure (pulmonary venous pressures) such as left-sided heart failure or mitral stenosis differ significantly from conditions that primarily affect the pulmonary arteries and arterioles such as idiopathic pulmonary artery hypertension (IPAH). The former causes a gradient between the PA diastolic and pulmonary capillary wedge pressure (PCWP) that is relatively small, with histopathologic changes in the arterial vessels that consist of mild medial hypertrophy and reversible intimal changes. In the latter, there is an increased pulmonary arteriovenous pressure gradient, and histologic changes on the pulmonary vasculature are more marked, including significant intimal hypertrophy with fibrosis, marked smooth muscle hypertrophy, vasoconstriction, adventitial proliferation, and thrombosis in situ.1 These changes cause vascular flow obstruction and eventually lead to abnormal angiogenesis and formation of plexiform arteriopathy. Endothelial dysfunction also develops with an imbalance between vasodilation and vasoconstriction and between apoptosis and proliferation, mechanisms that are thought to play the most important role in the development of chronic progressive PH. Hypoxemic pulmonary vasoconstriction is an important determinant of arterial PH in patients with respiratory disorders.1 In many types of PH, production of endogenous vasodilators (nitric oxide [NO] and prostacyclin) is impaired and production of vasoconstrictors (endothelin-1, thromboxane A) is increased.1 That is why the common treatment strategy for PH is to achieve the balance in key molecular pathways by increasing available NO and prostacyclin, or reducing the effects of endothelin-1. Acute cases are characterized by sudden increase in pulmonary arterial pressure (PAP) as seen when mechanical obstruction with subsequent vasoconstriction develops during an acute PE. In ARDS, both hypoxemia and the accumulation of intravascular fibrin and cellular debris contribute to subsequent vascular obliteration and PH.2 Endotoxin and vasoactive mediators related to pulmonary vasoconstriction also play significant roles in development of the PH during sepsis. Several animal studies have shown that endotoxin may cause not only systemic hypotension but also pulmonary biphasic hypertension, decrease in compliance, and increase in resistance of the respiratory system.3 Those endotoxin-dependent hemodynamic and respiratory effects are mediated by excessive release of inflammatory mediators and imbalance in production of NO, prostanoids, and endothelin-1.3,4 PH in endotoxemia is characterized by a constriction of proximal pulmonary arteries during the early phase followed by decreased compliance of distal pulmonary vasculature.5 Endotoxin infusion can also dramatically affect right ventricular function: in the very early phase of endotoxemic shock, right ventricular-vascular coupling is preserved by an increase in right ventricular contractility. Later, myocardial oxygen consumption and the energy cost of right ventricular contractility are increased, which along with progressive endotoxin-induced PH lead to right ventricular dysfunction and failure.6 The right ventricle (RV) differs from the left ventricle (LV) in morphologic appearance and functionality.7 Despite the requirement for a similar cardiac output between the RV and LV, the bioenergetic requirement for right ventricular function is approximately 20% of the LV. The RV is thinner than the LV and its shape differs from that of the LV, having a crescent-shaped morphologic appearance. These differences reflect the low resistance, low impedance, and high compliance of the pulmonary circulation.7 The high compliance allows quick adaptations to changes in preload; however, unlike the LV, the RV tolerates poorly the acute increases in afterload, which could lead to hemodynamic collapse.8 It is important to emphasize these differences between the ability of the RV to adapt to sudden (acute) versus gradual (chronic) elevation of PAP. A normal RV can acutely adapt to high flow, but is barely able to tolerate any but very short acute high-pressure load.9 The normal RV cannot acutely increase the mPAP to more than 40 mm Hg.10 In chronic sustained elevation of afterload as seen in PH, the RV increases its wall thickness by hypertrophy of the muscle mass and assumes a more rounded shape (Fig. 45.1). Eventually and despite the compensatory right ventricular hypertrophy to the sustained long-term pressure overload, the RV dilates. Neurohormonal activation develops during the right ventricular dilatation and is an important mechanism in both acute and chronic right ventricular failure. The consequence of sympathetic hyperactivity is an increase in PVR with impedance of flow, causing right ventricular strain that impairs filling and causes right ventricular volume and pressure overload. Furthermore, the RV dilatation increases oxygen consumption and reduces contractility, which is going to decrease right ventricular perfusion, and a vicious circle develops that ultimately leads to death. Tricuspid regurgitation develops as a result of right ventricular dysfunction and defines a poor prognosis.11 It is important also to mention the concept of functional interdependence between the RV and the LV. Anatomically, the superficial myocardial fibers encircle both ventricles, and both chambers are contained within the pericardium, sharing the interventricular septum.12 During elevation of right-sided heart pressures, the interventricular septum shifts progressively to the left with subsequent development of left ventricular diastolic dysfunction that reduces the LV’s cardiac output and coronary perfusion pressure.8,13 A downstream adverse effect of right-sided heart failure is the development of systemic venous hypertension leading to concomitant visceral organ congestion and dysfunction. Regardless of the underlying cause of PH, the final common pathway for hemodynamic deterioration and death is right ventricular failure. The classification of PH has presented different modifications since its first classification made in 1973 at a conference endorsed by the World Health Organization. The most recent classification of PH, described in Box 45.1, is based on causative diseases and was updated during the Fourth World Symposium on PH held in Dana Point, California.14 For the intensivist, it is important to recognize two different scenarios: patients with chronic PH admitted to the ICU for an acute process that may or may not worsen the underlying PH and patients with no history of chronic PH who develop acute PH during their ICU stay secondary to various conditions. It is also important to distinguish between pulmonary arterial hypertension as seen in IPAH and pulmonary venous hypertension as seen in left ventricular failure. A classification of PH in the ICU is described in Box 45.2. Individuals with preexisting PH (i.e., IPAH or portopulmonary hypertension [group 1]) are particularly vulnerable to acute illnesses, which commonly result in rapid clinical deterioration and even death.15 Besides the entities described in group 1 of the Dana Point classification, several other conditions that are associated with chronic PH and are more commonly encountered in the ICU include left ventricular heart failure (with or without preserved ejection fraction causing pulmonary venous hypertension; group 2); interstitial lung diseases, chronic obstructive pulmonary disease (COPD), chronic hypoventilation syndromes, and sleep disorder breathing (group 3); and chronic pulmonary thromboembolic disease (group 4). Several clinical factors faced during intercurrent critical illness can aggravate or unmask the hemodynamics of patients with preexisting PH and are outlined in Table 45.1. These patients with chronic PH can rapidly deteriorate and usually die from progressive right ventricular failure (49%), progressive respiratory failure (18%), or sudden cardiac death (17%). Cardiopulmonary resuscitation (CPR), even when attempted in the hospital setting, is rarely successful. Only 6% of patients survived for more than 90 days and most of the survivors had identifiable causes of circulatory arrest that were rapidly reversible. The pulmonary blood flow is virtually absent in these patients during CPR. In 54%, cardiorespiratory arrest was associated with an intercurrent illness,15 illustrating how preexisting PH adversely affects patients’ compensatory capacity and ability to survive an acute illness. Acute PH is caused by an abrupt increase in PVR. The prototype of this process is an acute PE; however, other conditions frequently seen in the ICU can also be associated with acute increase in PVR such as acute decompensated left ventricular failure, post cardiac surgery, ARDS, and sepsis.16 Acute right ventricular failure develops in 61% of patients who present with massive PE that involves at least two lobar arteries. The mortality rate ranges from 3% in hemodynamically stable patients to 59% in unstable ones.17,18 Hemodynamic instability in the setting of PE is defined as systolic blood pressure (SBP) less than 90 mm Hg or a drop in SBP greater than 40 mm Hg from baseline for more than 15 minutes that is not otherwise explained by hypovolemia, sepsis, or new arrhythmia.18 The degree of shock inferred from the presence of metabolic acidosis, but not transthoracic echocardiography (TTE) findings, is the most powerful predictor of death in these patients.17,19 Right ventricular dysfunction as a complication of ARDS is more gradual than in patients with massive PE, usually occurring at least 48 hours after the beginning of respiratory support.16 Evaluation of right ventricular function by TTE in a group of 75 ARDS patients submitted to protective ventilation demonstrated 25% incidence of acute right ventricular failure, resulting in detrimental hemodynamic consequences associated with tachycardia. However, those changes in heart function were reversible in patients who recovered; furthermore, it did not increase mortality rate.16 Although the initial magnitude of PH was not an indicator of mortality rate, mPAP increased in nonsurvivors, but not in survivors when followed for 7 days.20 Thus, development of PH in ARDS patients seems to be a sign of poor prognosis. In another cohort of 352 ARDS patients, both mortality rate and incidence of right ventricular failure were related to the level of plateau pressure during mechanical ventilation. In patients without acute cor pulmonale, the odds ratio of mortality for an increase in plateau pressure from 18–26 to 27–35 cm H2O was 1.15 (p = 0.635); however, for patients with acute cor pulmonale, the odds ratio of mortality for an increase in plateau pressure from 18–26 to 27–35 cm H2O was 3.32 (p = 0.034), suggesting that the threshold for a safe plateau pressure depends on the presence or not of acute cor pulmonale.21 Importantly, the implementation of low tidal volume ventilation in patients with ARDS has significantly lowered not only mortality rates but also incidence of acute right ventricular failure in this patient population.16 In addition to being the major risk factor for ARDS development, sepsis itself can sometimes lead to severe acute arterial PH.22 Some surgical interventions, in particular vascular, cardiac, and thoracic surgery, may cause acute elevation of mPAP either during the surgery or shortly after the intervention has been completed. This is particularly dangerous in patients with preexisting PH, because even short-lasting increased pressure overload to the RV could lead to profound decompensation with all downstream negative hemodynamic consequences. Preexisting PH is one of the major risk factors for morbidity and death in cardiothoracic surgery patients.23 PH is a major determinant of perioperative morbidity and mortality rate in special situations such as heart and lung transplantation, pneumonectomy, and ventricular assist device placement.24 The elevated PAP during and after surgery is thought to develop secondary to acute left-sided heart failure/dysfunction, or it can also be a consequence of pulmonary parenchymal and endothelial injury with activation of the systemic and pulmonary inflammatory response to cardiopulmonary bypass circulation or ischemia-reperfusion.25 Protamine-mediated acute PH and right ventricular failure in the perioperative period are common complications of cardiopulmonary bypass circulation during open-heart operations.26 PH can also develop later as a result of ARDS27 or other complications (sepsis, PE, etc.) not directly related to either surgery or anesthesia. When PH is suspected based on presentation, examination, and risk factors, a comprehensive and structured evaluation should be performed. Physical examination is usually variable and nonspecific. The presence of an accentuated pulmonary component of S2, an early systolic click, and a midsystolic ejection murmur from turbulent pulmonary outflow should raise the suspicion. Left parasternal lift and an S4 are signs of right ventricular hypertrophy. Distended jugular veins and hepatojugular reflux indicate high central venous pressure. Right ventricular S3, hepatomegaly, ascites, systemic hypotension, peripheral edema, and cool extremities are all signs of right ventricular failure. A high level of suspicion is paramount in establishing a timely diagnosis of PH in order to initiate therapy. The diagnostic endeavor is aimed at making the diagnosis of PH and also in finding its cause. General guidelines for the evaluation of PH are described in detail in Figure 45.2. Chest radiographic findings are usually nonspecific but enlarged main and hilar PA shadows could be seen. RV enlargement best seen in the lateral views could also suggest PH. Moreover, the chest radiograph can also present findings of underlying primary lung disease such as emphysema or pulmonary fibrosis. Electrocardiography has a low sensitivity and specificity for the diagnosis of PH; however, evidence of right atrial enlargement, right axis deviation, and RV enlargement is suggestive of the disease. In many cases, PH remains undiagnosed and its treatment begins only after serious complications have developed. Some serologic markers, such as troponin and natriuretic peptides, are important for the evaluation of right ventricular dysfunction. Serum troponin may be elevated in patients with PH and has been associated with right ventricular overdistention and ischemia. Troponin I leak due to acute right ventricular strain from PE has been well studied and may predict mortality rate.28,29 Elevated B-natriuretic peptide (BNP) is an important prognostic indicator and correlates strongly with PVR, cardiac output, and functional status in patients with PH.30 A high level of plasma BNP, and in particular, a further increase in plasma BNP during follow-up, may have a strong independent association with increased mortality rates in patients with PH.31 However, the significance of measuring BNP level in patients with PH in the acute setting remains unclear. Echocardiography is the most important and useful noninvasive study for screening of PH. It is very important for diagnosing and determining the degree and clinical significance of PH in critically ill patients. It can noninvasively visualize cardiac anatomy and certain intracardiac shunts and valvular abnormalities, estimate right atrial and pulmonary arterial pressures, determine the severity of right and left ventricular dysfunction and wall motion abnormalities, and reveal other potential causes of PH. In the absence of pulmonary outflow obstruction, PA systolic pressure is equivalent to right ventricular systolic pressure (RVSP), which can be calculated from measured systolic regurgitant tricuspid flow velocity and estimated right atrial pressure. PH by TTE is usually defined as RVSP greater than 35 mm Hg with the expected upper normal limit up to 40 mm Hg in older or obese subjects.32 However, it has limitations and echocardiography has a 45% false-positive rate of diagnosis when patients subsequently undergo right-sided heart catheterization.33 Among 3790 healthy people who underwent TTE, RVSP was highly variable in the range of 15 to 57 mm Hg and was associated with age, body mass index (BMI), gender, wall thickness, and ejection fraction. An RVSP greater than 40 mm Hg was found in 6% of those older than 50 years and 5% of those with a BMI greater than 30 kg/m2.32 Therefore, not every elevation of RVSP indicates the presence of a pathologic condition. Possible explanations for mildly elevated RVSP detected by TTE include34 (1) overestimation of the RVSP in a patient with true normal pulmonary pressure; (2) serendipitous observation of a transient pressure elevation in an otherwise healthy individual; (3) discovery of stable mild PH, and (4) discovery of early progressive PH. Echocardiographic signs of significant PH include right ventricular dilation (D-shaped RV) and its hypertrophy (in sustained cases), septal dyskinesia and bowing into the LV during late systole to early diastole, RV hypokinesis, tricuspid regurgitation, right atrial enlargement, and a dilated inferior vena cava.19,35,36 In patients with chronic PH, predictors of poor outcome include right atrial enlargement, septal bowing, and the development of a pericardial effusion.37 Increased RV size combined with increased outflow resistance and reduced ejection fraction have been also described in acute right ventricular failure.19 A specific pattern of right ventricular dysfunction in acute PE has been characterized by a severe hypokinesia of the RV mid-free wall, with normal contractions of the apical segment.38 Images may be suboptimal in critically ill patients because of limitations related to the patient’s general condition, limited positioning, attached monitoring devices, wound dressings, or ventilatory support. Transesophageal echocardiography (TEE) may be more accurate and sensitive in critically ill patients than TTE, especially in acute diseases such as PE when acute PH is highly suspected.39 Newly developed handheld ultrasound devices capable of TEE may sufficiently replace a standard cart-based TEE system in unstable critically ill patients.40 Advanced Doppler echocardiographic techniques allow for comprehensive hemodynamic assessment of the patients with PH. A high correlation between PA catheter and Doppler echocardiography evaluations of cardiac output, transpulmonary gradient, and PVR were observed in patients with severe PH.41 Invasive hemodynamic assessment using right-sided heart catheterization is considered the gold standard for the diagnosis of PH35; however, this procedure must be performed thoroughly and accurately. Besides direct measurement of the hemodynamic parameters, it also provides useful information regarding response to vasodilator therapy. Analysis of mixed venous oxygen saturations during passage of the PA on its way through the cardiac chambers can allow diagnosis of intracardiac shunts. A PCWP measurement reflects left ventricular end-diastolic (filling) pressure. Values less than 15 mm Hg rule out left ventricular, valvular, and pulmonary venous diseases as possible causes of the PH.35 It is important to emphasize that misinterpretation of the PCWP is a common pitfall during right-sided heart catheterization and it should be measured at the end of expiration and in several segments of the pulmonary vasculature because pulmonary veno-occlusive disease can cause elevated wedge pressure only in affected segments.42 In the ICU, placement of a PA catheter for diagnosis and monitoring is highly desirable in patients with severe PH and in patients with progressive heart failure.43 Although there is a little doubt that the hemodynamic data are valuable in the care of critically ill patients with acute conditions complicated by PH, there are no data available on how PA pressure monitoring could affect management and outcome of these patients. Indeed, placing a PA catheter could be a challenging and dangerous procedure in such patient populations. Technical difficulties could be related to severe tricuspid regurgitation, right ventricular dilatation, elevated PAP, and decreased cardiac output. Complications of PA catheterization are particularly dangerous in patients with PH and right ventricular dysfunction/failure. Arrhythmias in response to PA catheterization can have potentially life-threatening consequences by decreasing cardiac output, or converting into fatal ventricular arrhythmias. Obtaining a PCWP may be technically difficult in patients with markedly elevated PAP and also carries a high risk of sometimes fatal pulmonary arterial rupture. Finally, the presence of tricuspid regurgitation can significantly decrease accuracy of cardiac output calculations by thermodilution. Theoretically, the Fick method may be more accurate, but in critically ill patients with increased pulmonary metabolism and high or very low cardiac output, its accuracy may not be optimal.44
Pulmonary Hypertension
Pathophysiology of Pulmonary Hypertension and Right Ventricular Failure
Development of Pulmonary Hypertension
Right Ventricular Failure
Clinical Classification of Pulmonary Hypertension
Acute on Chronic Pulmonary Hypertension
Acute Pulmonary Hypertension
Acute Respiratory Distress Syndrome and Sepsis
Postsurgical Pulmonary Hypertension
Integrated Approach to the Diagnosis of Pulmonary Hypertension
Echocardiography
Right-Sided Heart Catheterization
Pulmonary Hypertension

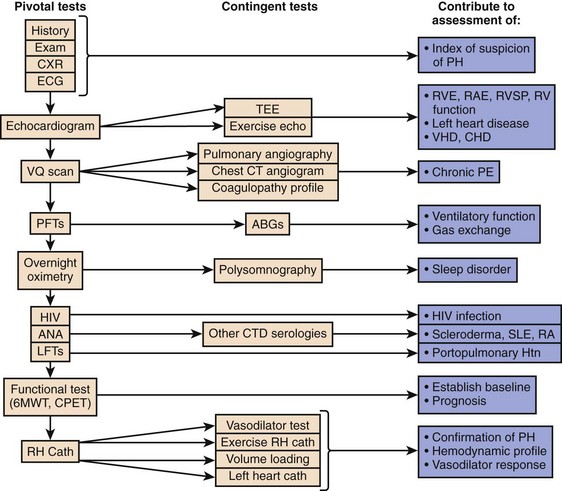
 scan and pulmonary angiogram) is contributing or predominant. Contingent tests are recommended to elucidate or confirm results of the pivotal tests and need only be performed in the appropriate clinical context. The combination of pivotal and appropriate contingent tests contributes to assessment of the differential diagnoses in the right-hand column. It should be recognized that definitive diagnosis may require additional specific evaluations not necessarily included in this general guideline. 6MWT indicates a 6-minute walk test. ABGs, arterial blood gases; ANA, antinuclear antibody serologic test; CHD, congenital heart disease; CPET, cardiopulmonary exercise test; CT, computed tomography; CTD, connective tissue disease; CXR, chest x-ray; ECG, electrocardiogram; HIV, human immunodeficiency virus screening; Htn, hypertension; IPAH, idiopathic pulmonary artery hypertension; LFT, liver function test; PAH, pulmonary artery hypertension; PE, pulmonary embolism; PFT, pulmonary function test; PH, pulmonary hypertension; RA, rheumatoid arthritis; RAE, right atrial enlargement; RHC, right-sided heart catheterization; RVE, right ventricular enlargement; RVSP, right ventricular systolic pressure; SLE, systemic lupus erythematosus; TEE, transesophageal echocardiography; VHD, valvular heart disease;
scan and pulmonary angiogram) is contributing or predominant. Contingent tests are recommended to elucidate or confirm results of the pivotal tests and need only be performed in the appropriate clinical context. The combination of pivotal and appropriate contingent tests contributes to assessment of the differential diagnoses in the right-hand column. It should be recognized that definitive diagnosis may require additional specific evaluations not necessarily included in this general guideline. 6MWT indicates a 6-minute walk test. ABGs, arterial blood gases; ANA, antinuclear antibody serologic test; CHD, congenital heart disease; CPET, cardiopulmonary exercise test; CT, computed tomography; CTD, connective tissue disease; CXR, chest x-ray; ECG, electrocardiogram; HIV, human immunodeficiency virus screening; Htn, hypertension; IPAH, idiopathic pulmonary artery hypertension; LFT, liver function test; PAH, pulmonary artery hypertension; PE, pulmonary embolism; PFT, pulmonary function test; PH, pulmonary hypertension; RA, rheumatoid arthritis; RAE, right atrial enlargement; RHC, right-sided heart catheterization; RVE, right ventricular enlargement; RVSP, right ventricular systolic pressure; SLE, systemic lupus erythematosus; TEE, transesophageal echocardiography; VHD, valvular heart disease;  scan, ventilation-perfusion scintigram.
scan, ventilation-perfusion scintigram. 







