Miscellaneous
Aldrete Scoring System
A scale commonly used to determine when postsurgical patients can be safely discharged from the Post Anesthesia Recovery Unit.
Aldrete Scoring System
| Assessment | Postprocedure Aldrete Scoring System | |
|---|---|---|
| Activity | Able to move four extremities voluntarily or on command | 2 |
| Able to move two extremities voluntarily or on command | 1 | |
| Not able to move extremities voluntarily or on command | 0 | |
| Respiration | Able to deep breathe and cough freely | 2 |
| Dyspnea, shallow or limited breathing | 1 | |
| Apneic | 0 | |
| Circulation | Blood pressure ±20 mm Hg of presedation level: stable pulse/pediatrics: return to VS baseline | 2 |
| Blood pressure ±20–50 mm Hg of presedation level: abnormal dysrhythmia | 1 | |
| Consciousness | Blood pressure ±50 mm Hg of presedation level: symptomatic dysrhythmia | 0 |
| Fully awake | 2 | |
| Arousable on calling | 1 | |
| Not responding | 0 | |
| O2 Saturation | Able to maintain SaO2 >90% on room air | 2 |
| Needs O2 to maintain SaO2 >90% | 1 | |
| SaO2 <90% even with O2 supplement | 0 |
More recently, the system has been modified, and two additional criteria were added, to create the modified Aldrete score:
Modified Aldrete Score Criteria
| Postoperative pain assessment | None or mild discomfort | 2 |
| Moderate to severe pain controlled with IV analgesics | 1 | |
| Persistent severe pain | 0 | |
| Postoperative emetic symptoms | None or mild nausea with no active vomiting | 2 |
| Transient vomiting or retching | 1 | |
| Persistent moderate to severe nausea and vomiting | 0 |
Anti-Embolism Stockings
Proper fit is required to obtain maximum benefit from compression hose. Improper fit will produce a reversed pressure gradient and is associated with a statistically higher incidence of DVT compared with stockings that produce a proper gradient.
Measurement for Knee Length Ted Compression Stockings
Measure calf circumference at the greatest portion to determine size;
Measure the distance from the bend of the knee to the bottom of the heel to determine length.
Knee Length TED Compression Hose
| Length | ||
|---|---|---|
| Calf Circumference | Regular | Long |
| Small >10″ but <12″ | Less than 16″ | 16″ and over |
| Medium 12″-15″ | Less than 17″ | 17″ and over |
| Large 15.1″-17.5″ | Less than 18″ | 18″ and over |
| X-Large 17.6″-20″ | Less than 18″ | 18″ and over |
Measurement for Thigh Length Ted Compression Stockings
Measure upper thigh circumference at the buttock fold;
Measure calf circumference at greatest portion to determine size;
Measure distance from the base of the heel to determine length.
Thigh Length TED Compression Hose
| Length | ||||
|---|---|---|---|---|
| Thigh Circumference | Calf Circumference | Short | Regular | Long |
| Less than 25″ (If >25″ but <32″ consider XL thigh length with belt, or knee length) | Small <12″ | <29″ | 29″-33″ | 29″-33″ |
| Medium 12″-15″ | <29″ | 29″-33″ | 29″-33″ | |
| Large 15.1″-17.5″ | <29″ | 29″-33″ | 29″-33″ | |
Apache Scoring System
The Acute Physiology and Chronic Health Evaluation (APACHE) score is a tool used to calculate a patient’s risk of hospital mortality after the first day of ICU, based on severity of disease. It compares each individual’s medical profile against nearly 18,000 cases in its memory before reaching a prognosis that is, on average, 95% accurate. The system consists of 4 components:
Age;
Major disease category (reason for ICU admission);
Acute (current) physiology;
Prior site of healthcare (emergency room, general floor, etc.).
Within 24 hours of admission, the physician must enter a number for each of several easily obtained facts. The sum of these numbers results in a score ranging from 0 to 71. (After the initial score has been determined, no new score can be calculated during the hospital stay. If a patient is discharged from the ICU and readmitted, a new APACHE score needs to be calculated.) Higher scores imply a more severe disease and a higher risk of death. A score of >50 is associated with increased mortality in nonpregnant cardiac and trauma patients.
Asa (American Society of Anesthesia) Classification Scale
(see Moderate Sedation in Part 8, p. 324)
Braden Scale
The Braden scale is used to assess for risk of development of pressure ulcers; the lower the numeric score, the higher the patient’s probability for development of pressure ulcers.
Braden Risk Interpretation
| Total Score | Potential Risk |
|---|---|
| 9 or less | Very high risk |
| 10–12 | High risk |
| 13–14 | Moderate risk |
| 15–18 | Low risk |
| 19–23 | No risk |
Braden Skin Assessment Scale
| SENSORY PERCEPTION Ability to respond meaningfully to pressure-related discomfort | 1. Completely Limited: Unresponsive (does not moan, flinch, or grasp) to painful stimuli due to diminished level of consciousness or sedation. OR limited ability to feel pain over most of body surface. | 2. Very Limited: Responds only to painful stimuli. Cannot communicate discomfort except by moaning or restlessness. OR has a sensory impairment that limits the ability to feel pain or discomfort over the half of body. | 3. Slightly Limited: Responds to verbal commands but cannot always communicate discomfort or needs to be turned. OR has some sensory impairment that limits ability to feel pain or discomfort in one or two extremities. |
| MOISTURE Degree to which skin is exposed to moisture | 1. Constantly Moist: Skin is kept moist almost constantly by perspiration, urine, etc. Dampness is detected every time patient is moved or turned. | 2. Very Moist: Skin is often but not always moist. Linen must be changed at least once a shift. | 3. Occasionally Moist: Skin is occasionally moist, requiring an extra linen change approximately once a day. |
| ACTIVITY Degree of physical activity | 1. Bedfast: Confined to bed. | 2. Chairfast: Ability to walk severely limited or nonexistent. Cannot bear own weight and/or must be assisted into chair or wheelchair. | 3. Walks Occasionally: Walks occasionally during the day, but for very short distances, with or without assistance. Spends majority of each shift in bed or chair. |
| MOBILITY Ability to change and control body position | 1. Completely Immobile: Does not make even slight changes in body or extremity position without assistance. | 2. Very Limited: Makes occasional slight changes in body or extremity position but unable to make frequent or significant changes independently. | 3. Slightly Limited: Makes frequent though slight changes in body or extremity position independently. |
| NUTRITION Usual food intake pattern | 1. Very Poor: Never eats complete meal. Rarely eats more than one third of any food offered. Eats two servings or less of protein (meat or dairy products) per day. Takes fluids poorly. Does not take a liquid dietary supplement. OR is NPO and/or maintained on clear liquids or IVs for more than 5 days. | 2. Probably Inadequate: Rarely eats a complete meal and generally eats only about half of any food offered. Protein intake includes only three servings of meat or dairy products per day. Occasionally will take a dietary supplement. OR receives less than optimum amount of liquid diet or tube feeding. | 3. Adequate: Eats over half of most meals. Eats a total of four servings of protein (meat, dairy products) each day. Occasionally will refuse a meal but will usually take a supplement if offered, OR is on a tube feeding or TPN regimen that probably meets most of nutritional needs. |
| FRICTION AND SHEAR | 1. Problem: Requires moderate to maximum assistance in moving. Complete lifting without sliding against sheets is impossible. Frequently slides down in bed or chair, requiring frequent repositioning with maximum assistance. Spasticity, contractures, or agitation lead to almost constant friction. | 2. Potential Problem: Moves feebly or requires minimum assistance. During a move, skin probably slides to some extent against sheets, chair, restraints, or other devices. Maintains relatively good position in chair or bed most of the time but occasionally slides down. | 3. No Apparent Problem: Moves in bed and in chair independently and has sufficient muscle strength to lift up completely during move. Maintains good position in bed or chair at all times. |
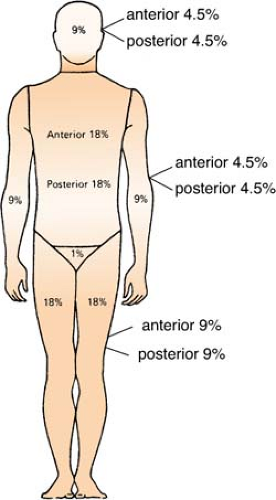
Burns
The rule of nines is a clinical calculation used to determine the percentage of body surface area burned on an adult. It provides a useful guide for fluid resuscitation and further treatment decisions.
Fluid Resuscitation
Fluid resuscitation is the major goal during the initial treatment of a burn patient. There are two common methods to determine this number:
Parkland (also known as the Baxter or Consensus) formula:
Lactated Ringer’s solution: 4 mL × kg body weight × % BSA burned
Half to be given over the first 8 hours postburn; remainder over the next 16 hours
Modified Brooke formula:
Lactated Ringer’s solution: 2 mL × kg body weight × % BSA burned
Half to be given over the first 8 hours postburn; remainder over the next 16 hours
There is a large difference in the amount of fluid between these two formulas. Which one to use will depend upon the needs of the patient. Remember, formulas are a guide only, and the goals are response to fluid administration and tolerance of the patient during therapy. For example, patients with inhalation injury or electrical burns, and those who were burned while intoxicated may require additional fluid, yet fluid overload can easily cause pulmonary or cerebral edema. However, if an inadequate amount of fluid is used in resuscitation, it may result in further insult to the pulmonary, renal, and mesenteric vascular bed. Ultimately, the fluid resuscitation effort will be determined by the patient’s response to it and needs to be reassessed hourly. Urine output of 0.5 to 1 cc/kg/hr for adults is commonly used as a resuscitation goal.
The addition of colloids during resuscitation is the subject of much controversy. Some clinicians assert that adding colloids to the fluid regime decreases the amount of fluid needed and also prevents massive edema formation. Others believe that after 24 hours, the integrity of the capillaries begins to be restored and the use of colloids during that time has no advantage at all. Further investigational studies are required.
Characteristics of Burns According to Depth
| Depth of Burn and Causes | Skin Involvement | Symptoms | Wound Appearance | Recuperative Course |
|---|---|---|---|---|
| SUPERFICIAL (FIRST DEGREE) | ||||
| Sunburn Low-intensity flash | Epidermis | Tingling Hyperesthesia (super sensitivity) Pain that is soothed by cooling | Reddened; blanches with pressure Minimal or no edema | Complete recovery within a week Peeling |
| PARTIAL THICKNESS (SECOND DEGREE) | ||||
| Scalds Flash flame | Epidermis and part of dermis | Pain Hyperesthesia Sensitive to cold air | Blistered, mottled red base; broken epidermis; weeping surface Edema | Recovery in 2 to 3 wk Some scarring and depigmentation Infection may convert it to third degree |
| FULL THICKNESS (THIRD DEGREE) | ||||
| Flame Prolonged exposure to hot liquids Electric current | Epidermis, entire dermis, and sometimes subcutaneous tissue | Pain free Shock Hematuria (blood in the urine) and, possibly, hemolysis (blood cell destruction) Possible entrance and exit wounds (electrical burn) | Dry; pale white, leathery, or charred Broken skin with fat exposed Edema | Eschar sloughs Grafting necessary Scarring and loss of contour and function Loss of digits or extremity possible |
Calculating Drug Doses
(see Drug Dose Calculations, p. 381)
Central Venous Catheters
A central venous catheter is any infusion device whose distal end is placed in the central venous system (superior vena cava or right atrium). Major types of vascular access catheters are:
Nontunneled
Tunneled
PICC (peripherally inserted central catheter)
Implanted
Nontunneled Catheters
These catheters are common in hospitalized patients and are useful because of their larger caliber. They are designed to be inserted into a relatively large central vein such as the internal jugular, subclavian, or femoral. Some types of nontunneled catheters are:
Single, double, triple, or quad lumen central venous catheters
Swan-Ganz catheters (see Swan-Ganz: Catheter Information in Part 2, p. 152)
Frequently, these catheters are used to monitor central venous pressure and/or pulmonary artery pressures and have an in-line flush device.
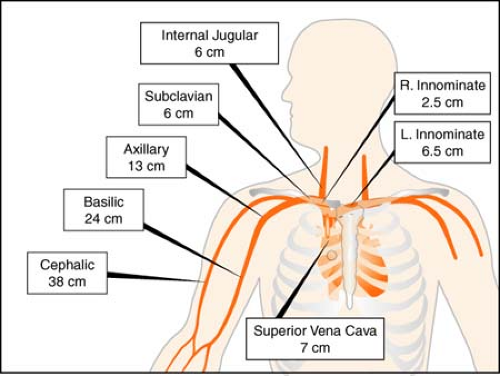 Figure. Central venous catheter lengths. (From Marino, P. L. [2007]. The ICU book [3rd ed.]. Philadelphia: Lippincott Williams & Wilkins.) |
To remove a nontunneled central venous catheter:
Place the patient in a supine position to prevent emboli.
Wash hands, and put on clean gloves and a mask.
Turn off all infusions, and prepare a sterile field, using a sterile drape.
Remove and discard the old dressing, and change to sterile gloves.
Clean the site with alcohol sponge or povidone-iodine solution.
Clip the sutures, and remove the catheter in a slow, even motion. Have the patient perform a Valsalva maneuver to prevent emboli.
Apply povidone-iodine ointment to the site to seal it, then cover with a gauze pad and transparent dressing. Keep site covered for 48 hours.
Inspect the catheter to see if any portions have broken off during removal. If so, notify the physician immediately, and monitor the patient closely.
Tunneled Catheters
These catheters travel under the skin before going into a vein, and contain a Dacron cuff that allows the surrounding tissue to grow in and secure the catheter in place. A tunneled catheter is usually the best choice when long-term access is required, and is more stable than a PICC. These catheters require flushing with normal saline before and after administration of a medication as well as a heparin flush. Examples of tunneled catheters are:
Hickman
Broviac
Groshong
Picc (Peripherally Inserted Central Catheters)
PICC lines can be from 20 to 25 inches in length and are inserted in the arm and threaded to a location deep in the large veins of the chest. Frequently used to receive fluids, blood products, and nutritional supplements, they may also be used to withdraw blood for lab tests. With proper care, a PICC line may be left in place from 2 weeks to 6 months. The line requires flushing with 10 cc’s of normal saline before and after medication administration, and at least two times weekly if the port is not used daily. While it is generally accepted that the site dressing should be changed weekly, referral to institution-specific policy is recommended.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree