Labs
Abg Values
(see also ABG Interpretation in Part 3, p. 168; Base Excess/Deficit in Part 3, p. 174; Mixed Venous ABGs in Part 3, p. 191)
Normal Arterial Blood Gas Values
| Arterial Blood | Mixed Venous Blood | |
|---|---|---|
| pH | 7.35-7.45 | 7.33-7.43 |
| PO2 | 80-100 mm Hg | 35-49 mm Hg |
| O2 Sat | 95% or greater | 70%-75% |
| PCO2 | 35-45 mm Hg | 41-51 mm Hg |
| HCO3 | 22-26 mEq/L | 24-28 mEq/L |
| Base excess | -2 to +2 | 0 to +4 |
Bilirubin
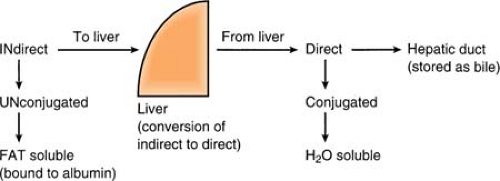
Bilirubin is the pigmented end product of hemoglobin breakdown and a component of bile. Bilirubin is normally excreted with bile into the duodenum; then, it is broken down by bacteria in the lower intestines. When the hepatic or biliary ducts become blocked for any reason, bile is no longer excreted into the bowel. It is absorbed in the blood, causing jaundice, and is excreted by the kidneys.
Any increase in indirect bilirubin = liver disease (hepatitis or cirrhosis). Liver cannot convert bilirubin, and it remains unchanged.
Any increase in direct bilirubin = biliary tract obstruction. Liver converts bilirubin, but obstruction is met, and direct bilirubin accumulates.
Any increase in both direct and indirect bilirubin = hepatic failure.
Bnp
(see also Chemistry Lab Values, p. 344; Heart Failure in Part 2, p. 110)
B-type natriuretic peptide (BNP) is a neurohormone secreted from the cardiac ventricles in response to ventricular stretch and pressure overload. It counteracts the vasoconstriction that occurs as a compensatory mechanism in heart failure. Dyspnea associated with cardiac dysfunction is highly unlikely in patients with levels <100 pg/mL, whereas most patients with significant CHF have levels >400 pg/mL. REMEMBER: Natrecor (nesiritide) is a recombinant form of human BNP used to treat patients with acutely decompensated CHF. Many assays cannot differentiate between the infused BNP and the patient’s natural BNP. Since the half-life of Natrecor is 20 minutes and is eliminated from the body within 2 hours, it is recommended that blood draws for BNP analysis not be done until a 2-hour suspension of the drug has been allowed.
C-Diff
(see Clostridium Difficile, p. 346)
C-Reactive Protein
C-reactive protein (CRP) is an acute-phase protein produced by the liver during systemic inflammation or a bacterial infection, such as rheumatic fever. The test does not, however, indicate where the inflammation is or what is causing it. It may be used to monitor risk after a surgical procedure (rises within 2-6 hours after surgery, then decreases by the third day).
Normal CRP (varies from lab to lab): Less than 10 mg/L
More recently, a special type of CRP test, the high-sensitivity CRP (hs-CRP) has been developed and is used as a risk predictor for recurrent cardiovascular and stroke events as well as indicating the increased risk of reclosure after angioplasty. (True independent association between hs-CRP and new cardiovascular events has not yet been established.)
hs-CRP < 1.0 mg/L = low risk
hs-CRP 1.0 to 3.0 mg/L = average risk
hs-CRP > 3.0 mg/L = high risk
Calcium
(see also Calcium in Part 8, p. 306; Hypocalcemia in Part 9, p. 352; Hypercalcemia in Part 9, p. 350)
Total Calcium
Normal range 8.5 to 10.2 mg/dL
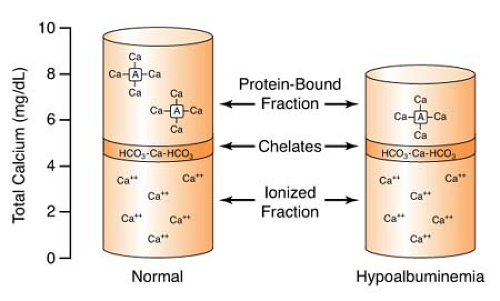
Approximately 40% of the body’s serum calcium is loosely bound to proteins, rendering it unavailable for use by the body. 13% is chelated to anions, and the remaining 47% is UNbound or “ionized,” and is metabolically active and readily available for use. Typical serum calcium measurements take into account all of these values (bound + ionized) to calculate the total calcium level.
Remember:
Calcium has an inverse relationship with phosphorus and serum pH.
Ionized Calcium
Normal range 4.7 to 5.1 mg/dL
Because albumin is responsible for 80% of the protein-bound calcium in plasma, any hypoalbuminemia will result in hypocalcemia reported on the total calcium value. However, as shown
in the figure below, while total calcium in the plasma may decrease, the ionized (unbound) calcium that is metabolically active remains unchanged, and therefore, the hypocalcemia is not physiologically significant. To determine a true hypocalcemia in the face of a low albumin level, an ionized calcium level must be obtained from the laboratory.
in the figure below, while total calcium in the plasma may decrease, the ionized (unbound) calcium that is metabolically active remains unchanged, and therefore, the hypocalcemia is not physiologically significant. To determine a true hypocalcemia in the face of a low albumin level, an ionized calcium level must be obtained from the laboratory.
Corrected Calcium
Corrected Ca (mg/dL) = (0.8 × [normal albumin – patient’s albumin]) + serum calcium
While this correction factor has been used in the past for adjusting the calcium value in patients with low albumin levels, its reliability has come into question. The use of direct laboratory testing of ionized calcium is recommended as the only method of identifying true hypocalcemia in the face of low albumin levels. The correction factor can be employed as a quick “estimate” but therapy should not be based on the results.
Cardiac Markers
The best marker to determine MI depends on the time from onset of symptoms. Earliest markers are myoglobin and the CK-MB isoforms. CK-MB and troponin are used in the intermediate period of 6 to 24 hours. Troponins are recommended in evaluating patients who present >24 hours after symptom onset. Lactic dehydrogenase (LDH) isoenzymes are rarely used.
Cardiac Markers
| Marker | Normal, Absent MI | In Presence of MI |
|---|---|---|
| CK | Males: 38-174 IU/L Females: 96-140 IU/L | Onset: 3-6 hours Peak: 24-36 hours Stays elevated 3-5 days |
| CK-MB* | Males: 0-4.2 ng/mL Females: 0-3.1 ng/mL | Onset: 3-6 hours Peak: 12-24 hours Stays elevated 2-3 days |
| *CK-MB can be separated into two isoforms: CK-MB1 and CK-MB2. The normal ratio of the two is < 1.0. Since CK-MB2 is initially released from the myocardium after an MI, a ratio that elevates > 1.7 yields a positive result. | ||
| Myoglobin** | Males: 20-90 ng/mL Females: 10-75 ng/mL | Onset: 2-4 hours Peak: 8-12 hours Returns to normal 24-36 hours |
| **Myoglobin is a protein that is released into the circulation after damage to heart or skeletal muscle. Compared to CK, it is more sensitive in the evaluation of myocardial damage but is not as specific because of its release after skeletal muscle injury as well. | ||
| Troponin I (TnI)*** | 0-2 ng/mL, but may be undetectable in normal healthy individual Rule in MI: > 2.0 ng/mL with a serial rise Rule out MI: < 0.6 with no rise | Onset: 3-4 hours Peak: 10-24 hours Stays elevated 1-2 weeks |
| Troponin T (TnT)*** | 0-3.1 ng/mL | Onset: 3-4 hours Peak: 10-24 hours Stays elevated 1-2 weeks |
| ***Both troponins are found in the myocardium and will elevate in the event of myocardial infarction. However, because troponin I is found exclusively in the myocardium and has 100% sensitivity for MI, it is emerging as the most accurate test for confirming the presence of myocardial damage. | ||
Cerebrospinal Fluid (Csf) Lab Values
| CSF Lab Values | ||
|---|---|---|
| Pressure | 70-180 | mm H2 O |
| Albumin | 20-48 | mg/dL |
| Ammonia | 25-80 | μ g/dL |
| Bicarbonate | 20-24 | mEq/L |
| Calcium | 2.1-3.0 | mEq/L |
| Cell count | 0-5 | Cells |
| Chloride | 116-122 | mEq/L |
| Glucose | 50-80 | mg/dL |
| Magnesium | 2.0-2.5 | mEq/L |
| Osmolality | 292-297 | mOsm/L |
| Phosphorus | 1.2-2.0 | mEq/L |
| Potassium | 2.7-3.9 | mEq/L |
| Protein | 20-45 | mg/dL |
| Sodium | 137-145 | mEq/L |
| Urea | 4.4-4.8 | mmol/L |
| Uric acid | 0.23-0.27 | mg/dL |
Chemistry Lab Values
| Chemistry Lab Values | Note: Values listed are guidelines only for the adult patient. Reference values are institution-specific | ||||
|---|---|---|---|---|---|
| A/G ratio | 1.2-2.3 | ||||
| Acetone, serum | Negative | ||||
| Acid phosphatase | 0-0.8 | U/L | |||
| Albumin | 3.8-5.0 | g/dL | |||
| Alcohol, ethyl | Negative | ||||
| Alkaline phosphatase | 36-120 | U/L | |||
| ALT | 0-35 | U/L | |||
| Ammonia, plasma | 11-35 | μ mol/L | |||
| Amylase, serum | 23-85 | U/L | |||
| Amylase, urine | 4-37 | U/2 hr | |||
| Anion gap | 7-17 | mEq/L | |||
| AST | 17-59 | U/L | |||
| Bilirubin direct | 0-0.4 | mg/dL | |||
| Bilirubin, indirect | 0-1.1 | mg/dL | |||
| Bilirubin total | 0-1.5 | mg/dL | |||
| BNP (see also BNP text) | 5-1,300 | pg/mL | |||
| >2,300 pg/mL significant for CHF | |||||
| BUN | 10-23 | μ g/dL | |||
| C-reactive protein (see also C-reactive protein text) | <10 | mg/L | |||
| C-reactive protein (hs) | <3.0 | mg/L | |||
| Calcium, ionized | 4.7-5.1 | mg/dL | |||
| Calcium, serum (see also hyper/hypocalcemia text) | 8.5-10.2 | mg/dL | |||
| Calcium, urine | 30-200 | mg/24 hr | |||
| Chloride, serum | 99-111 | mEq/L | |||
| Cholesterol, total | <300 | mg/dL | |||
| Cholesterol, HDL | ≥40 | mg/dL | |||
| Cholesterol, LDL | <120 | mg/dL | |||
| Cholesterol, HDLC ratio | <4.45 | Calc | |||
| Cortisol, urine | 20-90 | μ g/24 hr | |||
| Cortisol, serum AM | 5-25 | μ g/dL | |||
| Cortisol, serum PM | 2.5-12.5 | μ g/dL | |||
| Cortisol stimulation | 10-50 | μ g/dL | |||
| Cortisol suppression | 0-5 | μ g/dL | |||
| Creatinine clearance | |||||
| Male | 94-140 | mL/min | |||
| Female | 72-110 | mL/min | |||
| Creatinine, serum | 0.6-1.3 | mg/dL | |||
| Creatinine, urine | 1,000-2,000 | mg/24 hr | |||
| Ferritin | 20-300 | ng/mL | |||
| Folate, serum | >2.0 | ng/mL | |||
| Free thyroxine index | 1.1-4.8 | ||||
| Gastric fasting volume | 20-100 | mL | |||
| Gastric fasting pH | 1.5-3.5 | ||||
| Gastric unstim. free acid | 0-40 | mM | |||
| Gastric stim. free acid | 10-130 | mM | |||
| Gastric, 12-hr volume | 150-1,000 | mL | |||
| GGTP | |||||
| Male | 11-63 | U/L | |||
| Female | 8-35 | U/L | |||
| Glucose, fasting | 70-115 | mg/dL | |||
| Glucose, 2-hr PP | 70-115 | mg/dL | |||
| HgbA1C (see also HgbA1C text) | 4.2-4.6 | % | |||
| IgA | 57-414 | mg/dL | |||
| IgG | 568-1,483 | mg/dL | |||
| IgM | 20-274 | mg/dL | |||
| Iron, serum | 42-135 | μ g/dL | |||
| Iron binding capacity, total | 280-400 | μ g/dL | |||
| Iron saturation | 12-50 | % | |||
| Lactate (see also lactate text) | <2.0 | mMol/L | |||
| Lipase | 4-24 | u/L | |||
| Magnesium (see also hypomagnesium text) | 1.8-2.4 | mg/dL | |||
| Osmolality, serum | 280-295 | mOsm/kg | |||
| Osmolality, urine | 500-800 | mOsm/L | |||
| Phosphorus (see also hyperphosphatemia text) | 2.5-4.9 | mg/dL | |||
| Potassium, serum (see also hyper/hypokalemia text) | 3.5-5.0 | mEq/L | |||
| Potassium, urine | 25-120 | mM | |||
| Protein, total serum | 6.0-8.0 | g/dL | |||
| Protein, total urine | 40-150 | mg/24 hr | |||
| Salicylate | 0-29 | mg/dL | |||
| Sodium, serum (see also hyper/hyponatremia text) | 137-150 | mEq/L | |||
| Sodium, urine random | 40-220 | mM | |||
| Sodium, urine timed | 40-220 | mM/L | |||
| T3 uptake | 25-40 | % | |||
| T4 | 4.5-12 | μ g/dL | |||
| TSH | 0-7 | μ U/mL | |||
| Triglycerides | 40-150 | mg/dL | |||
| Uric acid, serum | |||||
| Male | 3.0-7.4 | mg/dL | |||
| Female | 2.1-6.2 | mg/dL | |||
| Vitamin B12 | 180-960 | ρg/mL | |||
Clostridium Difficile
C. diff is a gram-positive, anaerobic, spore-forming rod bacteria. It causes severe diarrhea after normal gut flora has been eradicated by the use of antibiotics and represents one of the most common nosocomial infections in the world. Generally appearing 4 to 9 days after beginning antibiotic intake, C. diff is most frequently linked to ampicillin, amoxicillin, clindamycin, and cephalosporins, although any antibiotic can be implicated.
Detection of C. diff in the stool is made by cytotoxicity assay. Since there is no correlation between the amount of bacteria found and the severity of the infection, results are reported only as “positive” or “negative.” The drawback of this particular assay is that it requires 24 to 48 hours to read. Immunoenzymatic assays, which take just a few hours to run, are commercially available in the form of diagnostic kits. They are, however, relatively less sensitive and demonstrate lower specificity when compared with the cytotoxicity assay and should be used for rapid screening only.
Treatment includes placing the patient in isolation and strict handwashing (patient-to-patient spread is a major risk factor). Soap and water is preferred over alcohol-based hand rubs, as the soap is shown to be more effective against spore-forming bacteria. A 10- to 14-day regime of metronidazole or vancomycin is initiated in uncomplicated patients. Diarrhea should improve within 1 to 4 days, with complete resolution in 2 weeks. It is common for approximately 10% to 20% of the patients to experience relapse. The usual therapy for reappearance of the symptoms is another 1- to 4-day course of either metronidazole or vancomycin.
Coagulation Lab Values
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree